- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Acute myocardial infarction: ICD code 10, symptoms, possible complications
The content of the article:
- What is myocardial infarction?
- Causes of the disease
- Classification of acute myocardial infarction
- Disease symptoms
- First aid for a heart attack
- Diagnostics
- Video
Acute myocardial infarction is the death of heart muscle cells due to the cessation of blood supply to them. This failure is caused in most cases by blockage of the vessel by a thrombus, embolus, or severe spasm.
Myocardial infarction is one of the most dangerous diseases: up to 30% of patients die in the first hours after an attack. This is due, inter alia, to the unpreparedness of others to act in such a situation. If you have the necessary information, you can provide urgent care to the patient in time, avoiding irreversible consequences.
What is myocardial infarction?
A heart attack is an acute circulatory disorder in which a piece of tissue of any organ ceases to receive the substances it needs for adequate and full functioning and dies. This process can develop in many organs with abundant blood flow, for example, in the kidneys, spleen, lungs. But the most dangerous is myocardial infarction.

Myocardial infarction is the death of a portion of the heart muscle
The disease is devoted to a separate section in the International Classification of Diseases, ICD code 10 for acute myocardial infarction - I21. The following identifier digits indicate the localization of the necrosis focus:
- I0 Acute transmural infarction of the anterior myocardial wall.
- I1 Acute transmural infarction of the lower myocardial wall.
- I2 Acute transmural myocardial infarction of other localizations.
- I3 Acute transmural myocardial infarction of unspecified localization.
- I4 Acute subendocardial myocardial infarction.
- I9 Acute myocardial infarction, unspecified.
Clarification of the localization of the necrotic focus is necessary to develop the correct therapeutic tactics - in different parts of the heart, different mobility and ability to regenerate.
Causes of the disease
Myocardial infarction is the end stage of coronary artery disease. The pathogenetic cause is an acute disturbance of blood flow through the coronary vessels - the main arteries that feed the heart. This group of diseases includes angina pectoris as a symptom complex, ischemic myocardial dystrophy and cardiosclerosis.
Immediate causes of heart attack:
- Prolonged spasm of the coronary arteries - narrowing of the lumen of these vessels can be caused by a disorder of the adrenergic system of the body, taking stimulating drugs, and total vasospasm. Although the speed of blood movement through them increases markedly, the effective volume is less than necessary.
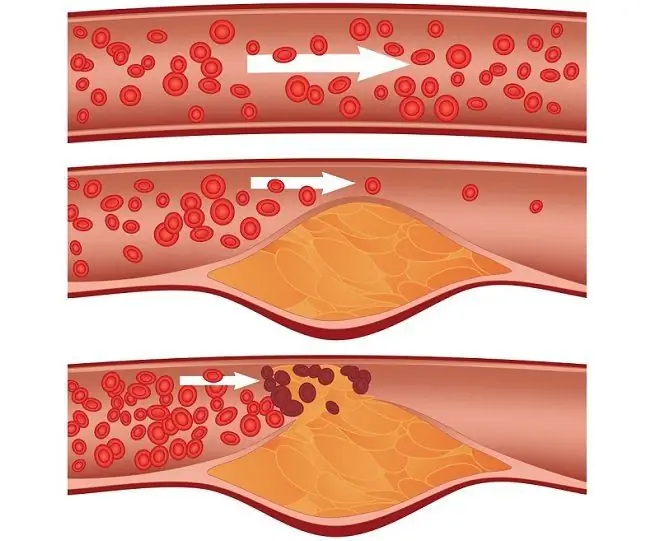
- Thrombosis or thromboembolism of the coronary arteries - Blood clots most often form in veins with low blood flow, such as the venous veins of the lower extremities. Sometimes these clots break off, move with the bloodstream and clog the lumen of the coronary vessels. Emboli can be particles of adipose and other tissues, air bubbles, foreign bodies that have entered the vessel during trauma, including surgical trauma.
- Functional overstrain of the myocardium in conditions of insufficient blood circulation. When blood flow is reduced from normal, but still covers myocardial oxygen demand, tissue death does not occur. But if at this time the needs of the heart muscle increase, corresponding to the work performed (caused by physical activity, stressful situation), the cells will exhaust their oxygen reserves and die.

A heart attack occurs when blood is blocked in an artery that feeds the heart
Pathogenetic factors that contribute to the development of the disease:
- Hyperlipidemia is an increased amount of fat in the blood. May be associated with obesity, excessive consumption of fatty foods, excessive amounts of carbohydrates. Also, this condition can be caused by dyshormonal disorders that affect, among other things, fat metabolism. Hyperlipidemia leads to the development of atherosclerosis, one of the main causative factors of heart attack.
- Arterial hypertension - an increase in blood pressure can lead to a state of shock, in which the heart, as an organ with abundant blood flow, suffers especially strongly. In addition, hypertension leads to vasospasm, which is an additional risk factor.
- Excess body weight - in addition to an increase in blood fat levels, is dangerous due to a significant load on the myocardium.
- A sedentary lifestyle - leads to a deterioration in the work of the cardiovascular system and increases the risk of obesity.
- Smoking - nicotine, together with other substances contained in tobacco smoke, causes a sharp vasospasm. When such spasms are repeated several times a day, the elasticity of the vascular wall is disrupted, the vessels become fragile.
- Diabetes mellitus and other metabolic disorders - in diabetes mellitus, all metabolic processes are dissociated, blood composition is disturbed, and the state of the vascular wall worsens. Other metabolic diseases also have a negative impact.
- Male sex - in men, unlike women, there are no sex hormones that would have a protective (protective) activity in relation to the vessel wall. However, in women after menopause, the risk of developing a heart attack increases and is compared with that in men.
- Genetic predisposition.
Classification of acute myocardial infarction
Pathology is classified according to the time of occurrence, localization, prevalence and depth of the lesion, as well as the nature of the course.
By the time of occurrence, there are:
- acute heart attack - occurring for the first time;
- repeated heart attack - occurring within 8 weeks after the first;
- recurrent - develops after 8 weeks after the primary.
The focus of tissue damage is most often localized in the apex of the heart, anterior and lateral walls of the left ventricle and in the anterior sections of the interventricular septum, that is, in the basin of the anterior interventricular branch of the left coronary artery. Less often, a heart attack occurs in the region of the posterior wall of the left ventricle and the posterior sections of the interventricular septum, that is, in the basin of the circumflex branch of the left coronary artery.
Depending on the depth of the lesion, a heart attack happens:
- subendocardial - a narrow necrotic focus runs along the left ventricular endocardium;
- subepicardial - the focus of necrosis is localized near the epicardium;
- intramural - located in the thickness of the heart muscle, without touching the upper and lower layers;
- transmural - affects the entire thickness of the heart wall.
In the course of the disease, four stages are distinguished - the most acute, acute, subacute, scarring stage. If we consider the pathological process from the point of view of pathological anatomy, two main periods can be distinguished:
- Necrotic. A zone of tissue necrosis is formed, a zone of aseptic inflammation around it with the presence of a large number of leukocytes. The surrounding tissues suffer from dyscirculatory disorders, and disorders can be observed far beyond the heart, even in the brain.
- Organization (scarring). Macrophages and fibroblasts arrive in the focus - cells that promote the growth of connective tissue. Macrophages absorb necrotic masses, and cells of the fibroblastic series fill the formed cavity with connective tissue. This period lasts up to 8 weeks.
Disease symptoms
The clinical manifestations of the disease can vary depending on the individual characteristics of the organism, the conditions under which the heart attack occurred, the specifics of the damage.
There are asymptomatic forms in which it is very difficult to recognize the disease - they are characteristic of patients with diabetes mellitus. There are other atypical forms: abdominal (manifested by abdominal pain, nausea, vomiting), cerebral (dizziness and headache dominate), peripheral (pain in the fingers of the extremities) and others.

A heart attack is accompanied by high-intensity pain that can cause painful shock, which is called anginal
The classic manifestations of a heart attack are:
- acute, burning, squeezing, so-called anginal pain behind the sternum, which extends to the entire front surface of the chest, radiates to the jaw, arm, between the shoulder blades. This unbearable pain is relieved only by narcotic analgesics;
- arrhythmia - the patient complains of a feeling of cardiac arrest, interruptions in his work, an unstable rhythm;
- tachycardia;
- pallor of the skin, blueness of the lips;
- a sharp drop in blood pressure, up to collapse. Pulse weak but fast;
- panic, fear of death.
First aid for a heart attack
The sequence of actions is presented in the form of an algorithm:
- Call an ambulance immediately - medical personnel have the skills necessary to support the patient's life, emergency means and the ability to quickly diagnose (they can conduct an ECG and confirm a heart attack, clarify its degree of damage and localization for further actions in the clinic).
- It is necessary to seat the patient, or transfer him to a reclining position. In the room, open a window, remove excess clothing from the patient - he needs a lot of oxygen.
- You can give the patient a tablet of Nitroglycerin or Aspirin - the first drug will expand the coronary vessels, and the second does not allow the blood to quickly clot, forming a thrombus. Let's take sedatives.
- Until the ambulance arrives, stay near the patient and try to calm him down.
Correctly provided first aid in the first minutes of a heart attack significantly reduces the risk of complications and increases the chances of recovery.
Complications of acute myocardial infarction
A large percentage of mortality from a heart attack falls not on the primary disease, but on its complications. The development of complications depends on the amount of assistance provided during the acute period and in the stage of scarring. There are frequent cases when patients who successfully survived a heart attack die after a few months due to delayed complications - which is why it is extremely important to take a responsible approach to medical recommendations and continue supportive treatment.
Complications of a heart attack are divided into early, arising in the first 8 weeks after manifestation, and late, developing after 8 weeks.
The early ones include:
- cardiogenic shock is a condition characterized by a discrepancy between the ejection of a portion of blood by the heart and peripheral vascular resistance. Acute heart failure occurs, while the vessels spasm from stress, which further aggravates the situation;
- myomalacia - melting of the necrotic myocardium, when autolysis of damaged tissues dominates. This process is practically irreversible, leads to a thinning of the heart wall, rupture of the heart, hemorrhages in the pericardium (the result is cardiac tamponade);
- acute aneurysm of the heart - possible with massive heart attacks, when the necrotic wall bulges outward, forming a space that quickly fills with blood, which flows poorly. Often, blood clots form in such cavities, the endocardium tears over time, and soon the pathological process spreads to other parts of the heart;
- parietal thrombi - formed in the absence of adequate treatment with fibrinolytics. Danger in increasing the risk of peripheral thromboembolic complications;
- pericarditis is an inflammation of the membranes of the heart, a frequent early complication of transmural myocardial infarction. Aseptic inflammation is aggravated by the addition of autoimmune processes;
- ventricular fibrillation is one of the most dangerous disorders of conduction and excitability of cardiac tissue, in which the heart cannot make a jolt and simply trembles, and blood circulation in the body practically stops;
- reperfusion syndrome - during the absence of blood flow in the affected tissues, many metabolites accumulate, stuck at the intermediate links of processing. If the heart attack lasts more than 40 minutes, and after that fibrinolytics were sharply injected, the blood immediately enters the affected area and activates all the accumulated reactions. As a result, many oxidants are released, which further damage the heart attack site.
Late complications:
- chronic heart failure - a condition in which a damaged heart due to a connective tissue scar is not able to fully provide the body with the necessary blood volumes, its pumping function suffers;
- Dressler's syndrome - an autoimmune disease in which antibodies are produced to necrotic tissue, which further increase inflammation and destruction in the heart attack zone;
- cardiosclerosis - replacement of specific tissues of the heart with connective tissue, which has a low capacity for elastic stretching, cannot actively contract. As a result, as the pressure or volume of blood in the heart increases, the wall can become thinner and swell.
Delayed complications slightly worsen the patient's standard of living, but have a high risk of mortality.

After suffering a heart attack, it is necessary to notify the doctor about all changes in health.
The patient should be aware of possible complications during recreation in order to warn the family and the attending physician in time about any changes in his condition. A heart attack and its complications must be entered into the medical history, in case another doctor will work with the patient. Clinical guidelines necessarily include the prevention of recurrent heart attacks and late complications.
Diagnostics
Diagnosis begins with a general examination, auscultation of heart murmurs and anamnesis. An ECG can be done in the ambulance and a preliminary diagnosis can be made. The first symptomatic treatment also begins there - narcotic analgesics are administered to prevent cardiogenic shock.
In a hospital, an echocardiogram of the heart is performed, which will allow you to see the full picture of a heart attack, its localization, the depth of damage, the nature of disturbances in the work of the heart in relation to the blood flows inside it.
Laboratory studies suggest the appointment of a biochemical blood test for specific markers of myocardial necrosis - CPK-MB, LDH1.5, C-reactive protein.
Video
We offer for viewing a video on the topic of the article.

Nikita Gaidukov About the author
Education: 4th year student of the Faculty of Medicine No. 1, specializing in General Medicine, Vinnitsa National Medical University. N. I. Pirogov.
Work experience: Nurse of the cardiology department of the Tyachiv Regional Hospital No. 1, geneticist / molecular biologist in the Polymerase Chain Reaction Laboratory at VNMU named after N. I. Pirogov.
Found a mistake in the text? Select it and press Ctrl + Enter.