- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Stages of myocardial infarction: acute, subacute, cicatricial
The content of the article:
-
Stages of myocardial infarction
- The first, most acute stage, or stage of ischemia
- Second, acute stage of myocardial infarction
- The third, subacute stage of myocardial infarction
- Stage 4 - cicatricial
- The mechanism of development of a heart attack
- Symptoms
- Diagnosis of a heart attack
- Treatment at different stages of a heart attack
- Video
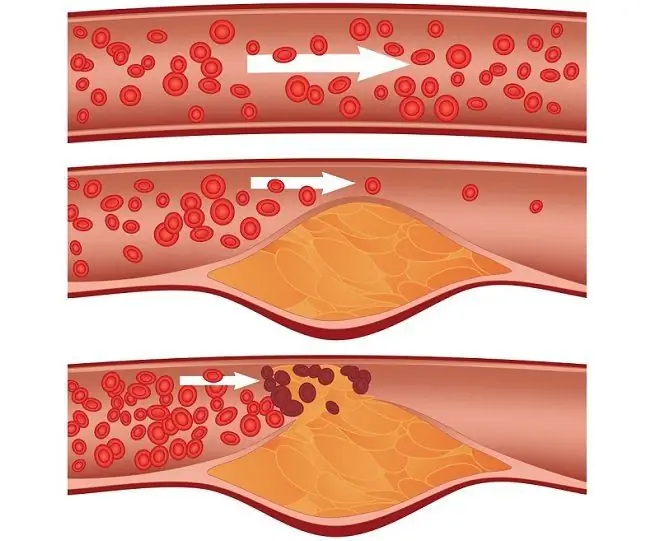
The stages of myocardial infarction, despite the rapid development of the process, are important to determine for first aid, treatment and prevention of delayed complications. Myocardial infarction is an acute violation of the circulation of the heart muscle, which leads to its damage. When a vessel that feeds a certain area of the heart becomes clogged, collapses or narrows as a result of spasm, the heart muscle experiences an acute lack of oxygen (and the heart is the most energy-consuming human organ), as a result of which the tissues of this area die - necrosis is formed.

It is important that medical care is provided in the early stages of myocardial infarction
Stages of myocardial infarction
The damage develops sequentially, in several stages. Since the immune system acts indirectly on tissues through biological transmitters, doctors have some time to help to avoid myocardial cell death, or at least minimize damage.
The first, most acute stage, or stage of ischemia
This is a very short, but most favorable period for first aid. Its duration is on average 5 hours from the onset of the attack, but it is quite difficult to clearly determine the moment of transition of angina pectoris to a heart attack, and the compensation time is individual, therefore, fluctuations in a rather wide range are possible. The pathological anatomy of the first stage consists in the formation of a primary zone of necrosis due to an acute circulatory disorder, and this focus will continue to expand subsequently. Already at this stage, the first clinical manifestations appear - acute chest pain, weakness, trembling, tachycardia. Unfortunately, very often patients cannot define this condition as a heart attack, do not attach importance to it, try to ignore it and suffer from dangerous complications.
Second, acute stage of myocardial infarction
This stage is characterized by the expansion of the zone of necrosis so much that the loss of this area of the heart muscle entails heart failure, systemic circulatory disorder. It can take up to 14 days in time. If adequate medical care is provided, this stage can also be compensated for, to stop tissue destruction. The number of cells that die during the acute stage will influence the appearance and nature of delayed complications. It is during this period that cardiogenic shock and reperfusion syndrome can develop - two dangerous early complications. Cardiogenic shock occurs when cardiac output decreases and peripheral vascular resistance prevents blood from pumping efficiently. Reperfusion syndrome develops with excessive use of fibrinolytics - then, after a long ischemia, cells abruptly return to work and are damaged by oxidized radicals.
The third, subacute stage of myocardial infarction
This is a watershed moment in the course of the disease. It lasts from two weeks to a month, at which time the cells in necrobiosis (borderline between life and death) cells still have a chance to return to work if conditions are favorable for recovery. This period is characterized by an immune response to aseptic inflammation. It is from this moment that Dressler's syndrome can develop, an autoimmune disease characterized by damage to the myocardium by immune cells. If the outcome is positive, the necrotic area is absorbed by macrophages, and the decay products are metabolized. The resulting defect begins to fill the connective tissue, forming a scar.
Stage 4 - cicatricial
The duration of the final stage of infarction is more than two months. In this phase, the connective tissue completely replaces the destroyed area. However, since this tissue is just the "cement" of the body, it is not able to take over the functions of the heart muscle. As a result, the ejection force weakens, rhythm and conduction disturbances are observed. At high pressure, the scar tissue stretches, the heart becomes dilated, the heart wall becomes thinner and may burst. However, adequate supportive therapy makes it possible to prevent this, and the absence of damaging agents provides patients at this stage with hope for a favorable outcome.
Sometimes the phases drop out or pass one into the other so that it is impossible to separate a particular stage of a heart attack. To find out which stage is taking place, and then adjust the treatment, instrumental diagnostics will allow.
The mechanism of development of a heart attack
Myocardial infarction is one of the most common and at the same time the most dangerous diseases of the cardiovascular system. It is characterized by high mortality, most of which occurs in the first hours of an attack of oxygen starvation (ischemia) of the heart muscle. Necrotic changes are irreversible, but occur within a few hours.

Stress is one of the triggers of myocardial infarction
Many factors affect the cardiovascular system, increasing the risk of heart attack. This is smoking, an unbalanced diet with a lot of trans fats and carbohydrates, physical inactivity, diabetes mellitus, an unhealthy lifestyle, night work, exposure to stress and many others. There are only a few reasons that directly lead to ischemia - a spasm of the coronary vessels supplying the heart (acute vascular insufficiency), their blockage by an atherosclerotic plaque or thrombus, a critical increase in myocardial nutritional requirements (for example, during heavy physical exertion, stress), damage to the vessel wall with its subsequent rupture.
The heart is able to compensate for ischemia for some time due to the nutrients accumulated inside cardiomyocytes (heart muscle cells), but the reserves are depleted after a few minutes, after which the cells die. The zone of necrosis cannot take a functional part in the work of the muscular organ, aseptic inflammation arises around it, and the systemic immune response to damage joins. If assistance is not provided at the right time, the heart attack zone will continue to expand.
Symptoms
Symptoms of the disease vary, but there are several signs that are highly likely to have a heart attack. First of all, it is cardiac pain, which radiates to the hand, fingers, jaw, between the shoulder blades.
The diagnostic criterion is a violation of the contractile, conductive, rhythm-forming work of the heart due to damage to the conducting system - the patient feels strong tremors of the heart, its stoppage (interruptions in work), irregular beats at different intervals. Systemic effects are also observed - sweating, dizziness, weakness, tremors. If the disease progresses rapidly, shortness of breath is added due to heart failure. Mental manifestations of a heart attack may be observed - fear of death, anxiety, sleep disturbances, suspiciousness and others.
Sometimes the classic symptoms are not pronounced, and sometimes atypical signs appear. Then they talk about atypical forms of myocardial infarction:
- abdominal - in its manifestations it resembles peritonitis with acute abdominal syndrome (intense pain in the epigastric region, burning sensation, nausea);
- cerebral - occurs in the form of dizziness, clouding of consciousness, development of neurological signs;
- peripheral - pain is distant from the source and is localized in the tips of the fingers, neck, pelvis, legs;
- painless, or oligosymptomatic form - usually occurs in patients with diabetes mellitus.
Anatomically, several types of heart attacks are distinguished, each of which damages different membranes of the heart. Transmural infarction affects all layers - a large area of damage is formed, cardiac function suffers to a large extent. Unfortunately, this species also accounts for most of all cases of myocardial infarction.
Intramural infarction has limited localization and a more favorable course. The damage zone is located in the thickness of the heart wall, but does not reach the outside epicardium and the inside endocardium. With subendocardial infarction, the lesion is localized immediately under the inner shell of the heart, and with subepicardial infarction - under the outer one.
Depending on the extent of the lesion and the characteristics of the necrotic process, large-focal and small-focal infarction is also distinguished. Large-focal one has characteristic signs on the electrocardiogram, namely, a pathological Q wave, therefore, a large-focal one is called a Q-infarction, and a small-focal one is a non-Q-infarction. The size of the damaged area depends on the caliber of the artery that has dropped out of the circulation. If the blood flow in the large coronary artery is blocked, a large-focal infarction occurs, and if the terminal branch is a small-focal one. Small focal infarction may almost not manifest itself clinically, in this case, patients transfer it on their legs, and the scar after alteration is discovered quite by accident. However, heart function suffers significantly in this case as well.
Diagnosis of a heart attack
The most important method for diagnosing a heart attack is an ECG (electrocardiogram), which is readily available and can be performed in an ambulance to identify the type and location of damage. By changes in the electrical activity of the heart, one can judge about all the parameters of a heart attack - from the size of the focus to the duration.

Small focal lesions of the heart muscle are called non-Q-infarction
The first stage is characterized by elevation (elevation) of the ST segment, which indicates severe ischemia. The segment rises so much that it merges with the T wave, an increase in which indicates myocardial damage.
In the second, acute stage of myocardial infarction, a pathological deep Q wave appears, which can turn into a barely noticeable R (it has decreased due to deterioration of conduction in the ventricles of the heart), or can skip it and go directly to ST. It is by the depth of pathological Q that Q-infarction and non-Q-infarction are distinguished.
In the next two stages, deep T appears and then disappears - its normalization, as well as the return of high ST to the isoline, indicates fibrosis, replacement of the lesion with connective tissue. All changes in the ECG are gradually leveled, only R will still gain the necessary potential for a long time, but in most cases it never returns to its pre-infarction indicator - the contractility of the heart muscle is difficult to return after acute ischemia.
An important diagnostic indicator is a blood test, general and biochemical. General (clinical) analysis allows you to see the changes characteristic of a systemic inflammatory response - an increase in the number of leukocytes, an increase in ESR. Biochemical analysis measures the level of enzymes specific to heart tissue. The indicators characteristic of a heart attack include an increase in the level of CPK (creatine phosphokinase) of the MV fraction, LDH (lactate dehydrogenase) 1 and 5, a change in the level of transaminases.
Echocardiography is the decisive examination to clarify the changes in hemodynamics in the heart after injury. It allows you to visualize blood flow, necrosis or fibrosis.

Ultrasound of the heart, or echocardiography, allows you to study in detail the coronary blood flow and the affected area
Treatment at different stages of a heart attack
In the initial stages, treatment is aimed at reducing the damage that the heart muscle receives. For this, drugs are introduced that dissolve the thrombus and prevent the aggregation, that is, sticking, of platelets. Also used are drugs that increase the endurance of the myocardium under conditions of hypoxia, and vasodilators to increase the lumen of the coronary arteries. The pain syndrome is stopped by narcotic analgesics.
In the later stages, it is necessary to control the patient's diuresis; in addition, vasoprotectors and various kinds of membrane stabilizers are used. Heart failure is to some extent compensated by cardiotonic drugs.
In the future, cardiac rehabilitation and supportive therapy are carried out.
Video
We offer for viewing a video on the topic of the article.

Nikita Gaidukov About the author
Education: 4th year student of the Faculty of Medicine No. 1, specializing in General Medicine, Vinnitsa National Medical University. N. I. Pirogov.
Work experience: Nurse of the cardiology department of the Tyachiv Regional Hospital No. 1, geneticist / molecular biologist in the Polymerase Chain Reaction Laboratory at VNMU named after N. I. Pirogov.
Found a mistake in the text? Select it and press Ctrl + Enter.