- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Early and late complications of myocardial infarction
The content of the article:
- Early complications
- Late complications
- Early signs of a heart attack
- Near signs of a heart attack
- How to prevent the development of complications after myocardial infarction
- Video
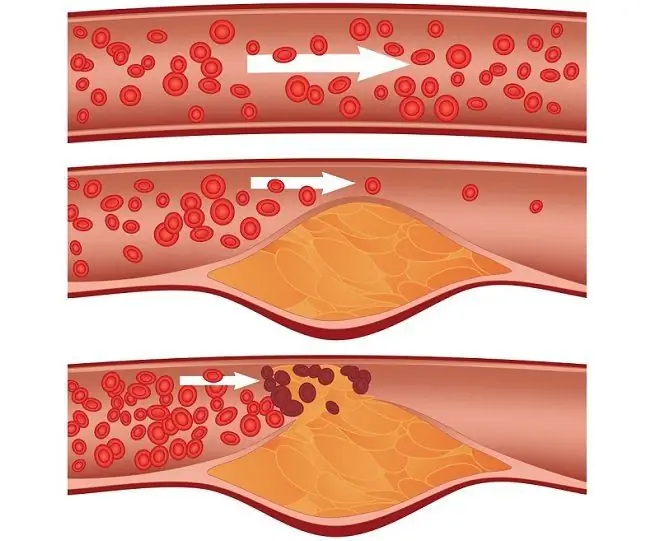
Complications of myocardial infarction - a serious cardiac disease, which is accompanied by necrosis of heart muscle cells due to a sharp cessation of blood circulation in it, caused by blockage of a coronary vessel, directly depend on the timeliness and adequacy of the medical care provided.
Myocardial infarction refers to conditions requiring resuscitation measures, since it poses an immediate threat to life. A heart attack can be uncomplicated and complicated, and can have early complications and long-term consequences. If diagnostics and medical care are carried out in a timely manner, the patient's chances of survival are quite high. The longer it takes from the onset of a heart attack to medical care, the higher the risk of severe complications.

To reduce the risk of complications from a heart attack, it is necessary to provide the patient with medical care as soon as possible.
Mortality from myocardial infarction in women is 9%, while in men it is only 4%. The probability of death in the short term (the first few hours) after a massive heart attack in women of young (under 30 years old) and middle (over 35 years old) age is 68% higher than in men of the same age. Clinicians attribute this to a higher risk of postinfarction complications in women.
Early complications
Early complications of a heart attack include:
- rhythm disturbances;
- conduction disturbances;
- cardiogenic shock;
- acute heart failure.
Sometimes they are the first and only manifestations of a heart attack, especially with repeated attacks.
Violations of the heart rhythm and conduction are recorded in the vast majority of patients in the first hours of the disease and in more than half of the patients in the following days. Some patients develop atrial fibrillation, less often - nodal atrioventricular tachycardia. The most severe rhythm disturbances are flutter and fibrillation (flickering) of the atria and ventricles, a consequence of excluding large muscle mass from the function. This is a formidable complication that carries an immediate threat to life.
Another serious and common complication of heart attack is cardiac conduction abnormalities due to damage to the heart muscle. The most dangerous of these are atrioventricular block and asystole.
One of the most severe complications of myocardial infarction is cardiogenic shock, which is caused by a severe hemodynamic disorder. Cardiogenic shock is manifested by acute chest pain, arterial hypotension, severe microcirculation disorders, impaired consciousness.
The clinical picture of cardiogenic shock:
- severe and prolonged arterial hypotension (however, cardiogenic shock sometimes occurs with normal blood pressure);
- pallor of the skin, cyanosis of the nasolabial triangle and fingers;
- cold sweat;
- frequent pulse of weak filling (small).
In severe cardiogenic shock, renal function suffers, which is manifested by oliguria up to anuria. There are cardiac arrhythmias: tachy- or bradycardia, extrasystole, atrioventricular blockade, atrial fibrillation and flutter, paroxysmal tachycardia. From the side of the central and peripheral nervous system - psychomotor agitation or weakness, confusion, temporary loss of consciousness, change in tendon reflexes.
Acute heart failure is the inability of the heart to cope with its function. If it cannot be compensated in time, it leads to pulmonary edema and death of the patient.
Late complications
Late complications that develop 2-3 weeks after the onset of the disease (in the subacute period and at the stage of scarring) and later include postinfarction syndrome, chronic heart failure, thromboembolism, aneurysm and heart rupture.
Chronic heart failure is a slowly progressive circulatory disorder characterized by congestion in the large and small circle and tissue starvation of almost all organs and systems. The condition is manifested by the following symptoms:
- dyspnea;
- reduced tolerance to normal stress;
- cough;
- peripheral edema.
One or another degree of chronic heart failure is diagnosed in all patients who have had myocardial infarction, since the functions of the heart muscle are irreversibly impaired even in the case of a favorable development of events. This is why patients often require lifelong therapy to maintain heart function and normal circulation.

Atrial fibrillation is one of the most formidable early complications of a heart attack
Postinfarction syndrome, also called Dressler's disease (Dressler's syndrome), develops 2-6 weeks after an attack. It is based on autoimmune reactions that cause an inflammatory process not only in the myocardium, but also in other tissues, which can lead to pericarditis, pleurisy, pneumonitis, and polyarthritis.
The connective tissue that replaces the dead part of the heart muscle does not have sufficient elasticity, so its stretching caused by high blood pressure in the heart can lead to protrusion of the connective tissue area (aneurysm) or expansion of the whole heart. Such a state with stress (physical or psychoemotional) is fraught with heart rupture.
Early signs of a heart attack
There are signs that allow you to identify the development of a heart attack even before it appears. These early signs include precursors of the disease, which appear in patients several weeks before the attack:
- increased fatigue, lack of energy, which is not removed even by prolonged rest;
- shallow or intermittent sleep, insomnia;
- snoring during sleep, apnea;
- swelling of the legs, feet and hands caused by impaired blood flow and poor heart function. Numbness or tingling sensation in the extremities;
- disorders of the gastrointestinal tract for no apparent reason in women. This symptom is explained by the fact that the diaphragm of the stomach and the digestive organs in the female body are close to the heart muscle. Thus, with ischemia of the lower parts of the posterior wall of the ventricle of the heart, this part of the body suffers;
- attacks of unexplained anxiety;
- frequent headaches, episodes of visual impairment;
- bleeding of the gums caused by impaired blood supply to peripheral vessels;
- Difficulty trying to take a deep breath or shortness of breath with little exercise
- heart palpitations, arrhythmia - the consequences of coronary artery disease;
- increased urge to urinate at night;
- discomfort in the chest, in the region of the heart.
These signs are nonspecific, that is, they are not characteristic of a heart attack, but the simultaneous presence of several of them is the reason for a cardiological examination.
Near signs of a heart attack
The sooner help is provided for a heart attack, the lower the risk of complications. The main sign of an approaching heart attack is chest pain, which is characterized by pressing and squeezing sensations that cause severe discomfort. The pain is most often localized in the center of the chest or on the left side of it. It is characterized by irradiation - recoil to other parts of the body, for example, to the upper abdomen, stomach, left shoulder, left shoulder blade, lower jaw, left arm, neck.
The pain can be of different intensity and nature, but most often patients describe it as acute, pressing, bursting, burning. A distinctive feature of the pain syndrome with a heart attack is the inability to relieve it when changing posture, as well as with the help of drugs. If, with angina pectoris, the painful sensations disappear after the resorption of the Nitroglycerin tablet, when a heart attack begins, this remedy has no effect, so that the Nitroglycerin test is often used to recognize a heart attack.
Other symptoms that characterize the approaching heart attack:
- shortness of breath, feeling short of breath;
- strong heartbeat;
- weakness;
- dizziness;
- loss of coordination;
- profuse sweating (sweat during a heart attack is cold and sticky, its increased separation is associated with the release of adrenaline secreted by the adrenal glands into the bloodstream);
- nausea, vomiting;
- numbness of the left side of the body (arms, legs, neck);
- dry, painful cough;
- violation of visual function;
- nervous excitement;
- growing pallor.
How to prevent the development of complications after myocardial infarction
The course of a heart attack and its consequences directly depends on how timely and competent the emergency care will be. Timely treatment started significantly reduces the risk of complications and minimizes long-term consequences.
First of all, you need to call an ambulance. This should be done at the first suspicion of a heart attack, without waiting for the diagnosis to become clear (accurate diagnosis is impossible without an ECG).
Help to be provided to a person with a heart attack before the arrival of doctors:
- to sit the patient in a comfortable position, in case of loss of consciousness, lay on the right side, raise the head above the level of the body;
- unbutton, loosen or take off tight clothing (belt, collar, tie, belt), open windows in the room;
- as an emergency treatment, you can use a drug that the patient usually uses to lower blood pressure. You can also give him a Nitroglycerin pill - despite the fact that he cannot relieve the attack, it will help reduce ischemia;
- constantly be near the patient. If breathing stops and the heart stops, immediately start chest compressions.
The period when medical care is especially important and most effective is the first two hours after the attack. It is highly desirable that during this time the patient is taken to the clinic.
In the hospital, therapy is prescribed, aimed at preventing thrombus formation and cardiogenic shock, improving trophism of the heart muscle, and maintaining vital functions.

The need to restore blood supply to the heart muscle may require surgical intervention
In some cases, heart attack is treated surgically. Thus, the blockage of the vessel is eliminated and blood circulation in the heart muscle is restored. This reduces the risk of possible recurrence by 70%.
Rehabilitation of the patient plays an important role in preventing late complications. Rehabilitation measures are aimed at stabilizing blood pressure, respiration, heart rate, restoring normal vital functions, muscle tone of motor activity. Psychological rehabilitation and adaptation are of no less importance. The success of recovery and recovery depends on how carefully the patient will follow the clinical guidelines given to him.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.