- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Causes of myocardial infarction: causes and predisposing factors
The content of the article:
- Heart attack: causes and risk factors
- Risk groups: impact on the incidence of gender, age and place of residence
- Harbingers of myocardial infarction
- Signs of a heart attack
- The consequences of a postponed heart attack
- First aid
- Diagnostics
- Treatment tactics
- Video
The cause of myocardial infarction, an acute heart disease in which necrosis occurs, i.e. the death of a portion of the heart muscle, is the blockage of blood vessels by a thrombus or embolus, as a result of which blood flow in the coronary arteries is disturbed, which leads to insufficient blood supply to the heart.
Myocardial infarction is a clinical form of coronary heart disease (IHD) - a life-threatening condition, the risk of death is especially high in case of extensive infarction, untimely provision of medical care and the appearance of complications. According to statistics, 15-20% of the total number of all sudden deaths are myocardial infarction. Approximately 20% of patients die at the prehospital stage, and in another 15% of cases, death occurs in the hospital. The highest mortality rate is in the first few days from the onset of an attack, for this reason, timely seeking medical help and starting treatment as early as possible is important.
In the absence of blood flow to the heart muscle for more than 20 minutes, irreversible changes occur in it caused by cell death, which negatively affects the functioning of the organ. The focus of necrosis is subsequently replaced by connective tissue (post-infarction scar is formed), however, the connective tissue does not possess the properties inherent in the muscle tissue of the heart, and therefore complete recovery after a heart attack does not occur even with the most favorable development of events.

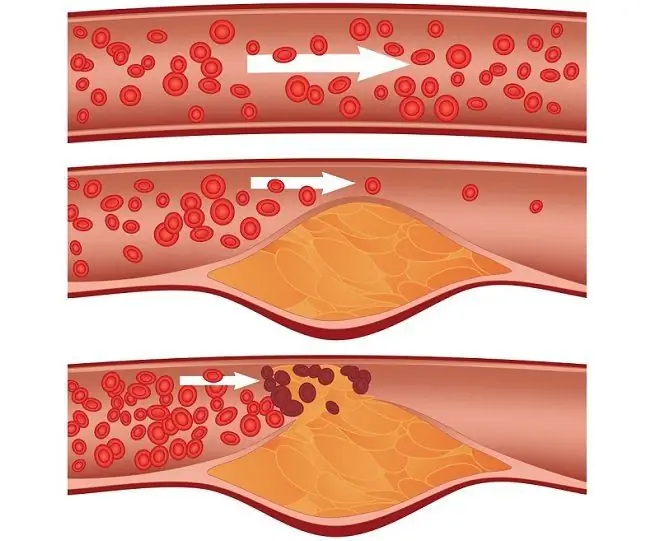
Atherosclerosis of the coronary arteries - a direct cause of heart attack
Heart attack: causes and risk factors
The main reasons for the development of myocardial infarction are:
- atherosclerosis - cholesterol plaques inside the blood vessels break off and enter the coronary arteries with blood flow, blocking blood flow in them;
- thrombosis - a thrombus, like a cholesterol plaque, is able to break off and enter the vessel supplying blood to the heart muscle with blood flow.
A foreign particle that has entered the bloodstream and blocked a vessel is called an embolus. Not only cholesterol plaques and blood clots can act as an embolus, but also adipose tissue, air bubbles, and other foreign particles that can enter the bloodstream during an injury, including the operating room. In addition, the cause of acute myocardial infarction can be a spasm of blood vessels (including against the background of uncontrolled use of drugs or drug use).
Factors that increase the risk of developing a heart attack include:
- genetic predisposition;
- hypercholesterolemia and hyperlipidemia caused by metabolic disorders due to malnutrition or diseases;
- arterial hypertension;
- diabetes;
- hypodynamia;
- obesity;
- stress;
- overwork (both physical and psycho-emotional).
Myocardial infarction can occur as a complication of other diseases:
- malformations of the coronary arteries;
- malignant tumors;
- aortic aneurysm;
- diseases affecting the endothelium of blood vessels (vasculitis, systemic diseases);
- syndrome of disseminated intravascular coagulation, developed against the background of infectious diseases, a decrease in the volume of circulating blood, malignant blood diseases, intoxication, etc.;
- mechanical and electrical injuries, extensive burns.
Risk groups: impact on the incidence of gender, age and place of residence
In recent years, more and more cases of myocardial infarction have been reported in young patients. The most vulnerable group of the population is men from 40 to 60 years old. In the age group of 40-50 years, a heart attack in men develops 3-5 times more often than in women, which is explained by the action of female sex hormones, one of the actions of which is to strengthen the vascular wall. After women enter the menopause (50 years and older), the incidence in them and in men becomes the same.

Most often, myocardial infarction occurs in men 40-60 years old.
In young patients, the cause of myocardial infarction is most often heart defects and coronary arteries, in the elderly - atherosclerotic changes in the coronary vessels.
Women more often than men develop an atypical form of myocardial infarction, which often leads to untimely detection of the disease and explains the more frequent development of adverse consequences in them, including death.
Residents of industrially developed countries and large cities are more susceptible to the occurrence of the disease, which is explained by their greater susceptibility to stress, frequent nutritional errors and less favorable environmental conditions.
Harbingers of myocardial infarction
In the clinical picture of the disease, five periods are distinguished: preinfarction, acute, acute, subacute and postinfarction (scarring).
The sudden development of a heart attack is noted only in 43% of cases, in other patients myocardial infarction is preceded by a period of unstable angina pectoris, manifested by pain in the chest at rest. This period can be of different duration - from several days to a month. At this time, the patient develops the so-called precursors - symptoms that indicate an impending cardiac catastrophe. As a rule, there is weakness, increased fatigue, sleep disorders (difficulty falling asleep, nocturnal awakening), shortness of breath after minor physical exertion, numbness of the limbs or feeling of goose bumps in them. There may be disturbances from the visual analyzer, headache, pallor of the skin, cold sweat, mood swings, anxiety, restlessness. Besides,patients may complain of nausea, vomiting, heartburn.
The listed signs can disappear on their own and appear again, which is the reason for the patient to ignore them.
Signs of a heart attack
The first and most striking sign of myocardial infarction is usually chest pain. It has a high intensity, patients describe it as dagger-like, unstoppable. The burning pain is pressing, bursting in nature (the so-called anginal pain). The pain syndrome is accompanied by dizziness, cold sweat, difficulty breathing, nausea. Blood pressure usually rises during an attack and then drops sharply or moderately. The patient may have arrhythmia, tachycardia. Often the attack is accompanied by a dry cough.
An attack of pain often has an undulating character, the pain then subsides, then it worsens again. The duration of an attack is usually 20-40 minutes, but it can last for several hours, and in some cases, days. A characteristic sign of a heart attack, which distinguishes it from angina pectoris, is that taking Nitroglycerin does not relieve this pain.
By the end of the acute period, the pain subsides. Its persistence in the acute period may indicate the development of ischemia of the peri-infarction zone or pericarditis. Against the background of necrosis and inflammatory changes in the lesion focus, the body temperature rises. Fever can last 10 days or more - the larger the area of damage to the heart muscle, the longer the fever lasts. In the same period, the patient usually has signs of arterial hypotension and heart failure. The outcome of the disease largely depends on the course of the acute period. If the patient survives at this stage, it is followed by a subacute period, during which the body temperature normalizes, the pain syndrome disappears, and the general condition improves. In the postinfarction stage, the relative normalization of the patient's condition continues.

Nitroglycerin with a heart attack is not able to relieve pain, however, taking it as part of the provision of first aid will not be superfluous
This, the most common form of heart attack, is called typical or anginal. There are also atypical forms that differ from each other and from the anginal clinical picture of the acute period. At all subsequent stages, similar symptoms are observed.
The asthmatic form is characterized by shortness of breath, up to choking, and tachycardia - symptoms that mimic an asthmatic attack. Pain in the region of the heart is mild or absent at all. This form of the disease is recorded in about 10% of cases and usually develops in patients who already have a history of myocardial infarction, and in elderly patients.
Cerebrovascular myocardial infarction has symptoms similar to those of a stroke. The patient has a headache, dizziness, disorientation in space, impaired consciousness up to its loss, sometimes the described manifestations are accompanied by vomiting. The cerebrovascular form accounts for about 5% of all cases of heart attack, the frequency of occurrence increases with age.
With the gastralgic form of a heart attack, pain is observed in the upper abdomen with radiation to the back. The pain is accompanied by hiccups, heartburn, bloating, belching, nausea, vomiting, and sometimes diarrhea. The attack mimics an exacerbation of pancreatitis or foodborne disease. This form of the disease is recorded in about 5% of cases.
In arrhythmic infarction, heart rhythm disturbances are the leading symptom. Chest pain is mild or absent. The attack is accompanied by shortness of breath, increasing weakness. This form of myocardial infarction is diagnosed in 1-5% of patients.
With an erased form, the transferred heart attack is often detected later, being an accidental find when conducting an electrocardiographic study for another reason. Pain with this type of heart attack is absent or weak, there is a deterioration in general health, increased fatigue, shortness of breath. This form of heart attack is usually found in patients with diabetes mellitus.
The consequences of a postponed heart attack
Complications of a heart attack can occur from the first hours after the onset of the disease, their appearance significantly worsens the prognosis.
In the first few days, heart rhythm disturbances often develop. Atrial fibrillation is one of the most serious complications of myocardial infarction, since it can turn into atrial and ventricular fibrillation, which in many cases is fatal. In the early postinfarction period, cardiac arrhythmias of varying degrees are recorded in all cases, in the late postinfarction period - in about 40% of patients.
The development of left ventricular heart failure in a patient who has had a heart attack is manifested by cardiac asthma, and in severe cases - pulmonary edema. Left ventricular heart failure can also cause cardiogenic shock, another complication that can be fatal. Cardiogenic shock is manifested by a drop in blood pressure below 80 mm Hg. Art., tachycardia, acrocyanosis, loss of consciousness.
The rupture of muscle fibers in the necrosis zone causes cardiac tamponade, in which blood flows into the pericardial cavity. With extensive myocardial damage, ventricular rupture is possible, the risk of which is highest in the first 10 days after an attack.

Ventricular fibrillation is a serious complication of heart attack that can lead to death
In 2-3% of patients, there is a blockage of the pulmonary artery by a thrombus, which is usually fatal.
Complication of myocardial infarction by thromboembolism is observed in 5-7% of patients.
Acute mental disorder complicates heart attack in about 8% of cases.
3-5% of patients with a heart attack develop ulcers of the stomach and intestines.
In 12-15% of cases, myocardial infarction is complicated by chronic heart failure.
A formidable late complication is postinfarction syndrome (Dressler's syndrome), caused by an abnormal response of the immune system to necrotic tissue. Autoimmune inflammation can affect both nearby and remote body tissues, such as joints. Postinfarction syndrome can manifest itself with joint pain, fever, pleurisy, pericarditis. This complication develops in 1-3% of patients.
First aid
If you suspect a heart attack, you should immediately call an ambulance. Before her arrival, the person needs to be given first aid. The patient should be tried to calm down, sit down, provide him with oxygen access, for which to loosen tight clothes and open the windows in the room. If you have Nitroglycerin on hand, you need to give a pill to the patient. The drug will not relieve pain, but it will still help improve coronary circulation. The patient should not be left alone until the ambulance arrives. If he loses consciousness, you should immediately start chest compressions.
Diagnostics
The main method for diagnosing a heart attack is ECG, electrocardiography. In addition to it, ultrasound of the heart (echocardiography) and a biochemical blood test are performed. One of the methods specific to infarction to confirm the diagnosis is the troponin test, which can detect even minor myocardial damage. An increase in troponin in the blood is noted for several weeks after an attack.

The main method for diagnosing a heart attack is ECG
Treatment tactics
First aid for a heart attack consists in improving the blood supply to the heart, preventing thrombosis, and maintaining the vital functions of the body. Further treatment aims at the fastest scarring of necrosis and the most complete rehabilitation.
The success of rehabilitation largely depends on how responsibly the patient treats the prescribed treatment and recommendations for changing lifestyle. In order to prevent relapse (repeated heart attack develops in more than a third of cases), it is necessary to abandon bad habits, follow a diet, ensure adequate physical activity, adjust body weight, control blood pressure and blood cholesterol levels, and also avoid overwork and psycho-emotional overstrain - then is to eliminate all factors contributing to the development of myocardial infarction.
Video
We offer for viewing a video on the topic of the article.

Anna Aksenova Medical journalist About the author
Education: 2004-2007 "First Kiev Medical College" specialty "Laboratory Diagnostics".
Found a mistake in the text? Select it and press Ctrl + Enter.