Types of myocardial infarction: anginal, atypical and other forms
The content of the article:
- 5 types of infarction according to the classification of the World Heart Federation
- Classification of myocardial infarction by stages of development
- Anginal and atypical forms of myocardial infarction
- Anatomical classifications
- Diagnosis of the disease
- Video
Types of myocardial infarction - what are the types and what is the basis for the classification of the disease? A heart attack is called the softening of tissues due to necrosis, that is, their death due to the lack of oxygen supply to them.
A heart attack can occur in various internal organs, but the most common is myocardial infarction. What is it and why is it happening? Due to the functional importance of the heart and the high demand for oxygen in the heart muscle, myocardial infarction develops very quickly and is accompanied by irreversible consequences. Several types of classifications of myocardial infarction have been created, each of which is important in the clinic.

The type of heart attack can be determined only after examination
5 types of infarction according to the classification of the World Heart Federation
The main classification of myocardial infarction is currently a classification prepared by a joint group of scientists from the World Cardiology Federation, which is based on the principle of an integrated approach to the cause, pathogenesis and clinical manifestations of pathology. Thus, myocardial infarction is divided into 5 types:
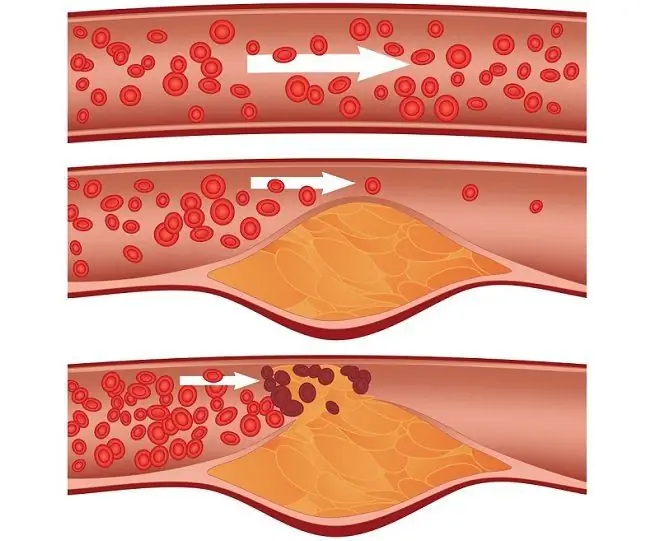
- type 1 - spontaneous myocardial infarction, the cause of which is a primary violation of the coronary circulation, for example, destruction of the wall of the coronary artery, erosion of an atherosclerotic plaque in its lumen, dissection of the vessel, i.e., the directly feeding vessel is damaged, which leads to insufficient trophism;
- type 2 - secondary myocardial infarction, which is caused by insufficient blood circulation due to coronary spasm or coronary artery thromboembolism. In addition, the possible causes of the second type are anemia, impaired blood perfusion (pumping), arterial pressure disorders, arrhythmias;
- type 3, or sudden coronary death caused by acute ischemia in combination with disturbances in the conduction system of the heart - left bundle branch block with characteristic signs on the ECG;
- type 4 is divided into 4a - complication of percutaneous coronary intervention (balloon angioplasty, stenting) and 4b - complication of coronary intervention associated with stent thrombosis;
- type 5 - myocardial infarction associated with coronary artery bypass grafting. It can occur both during surgery and as a late complication.
4 and 5 types indicate iatrogenic, that is, a violation of the heart circulation provoked by the actions of doctors.
Classification of myocardial infarction by stages of development
Most of all organic changes in the heart muscle during a heart attack occur in the first few hours after the onset of the attack. In the course of myocardial infarction, several periods are distinguished.
- The most acute period is the first six hours from the onset of the attack. At this time, maximum ischemia is noted, cell death begins, and compensatory mechanisms are activated. An important point in the treatment of a heart attack is assistance in this period - by expanding the vessels and giving the myocardium more oxygen, massive cell death can be prevented.
- Acute period - begins six hours after an attack and lasts up to two weeks. During this period, close monitoring of the patient's vital signs is necessary, since the risk of a second heart attack is high. In addition, against the background of therapy with fibrinolytics, a dangerous complication can develop - reperfusion syndrome. It is characterized by even greater damage to the heart muscle and its necrosis after a sharp resumption of blood circulation in the damaged area. It follows that blood flow should be resumed slowly to avoid tissue damage by free radicals in fresh blood.
- The subacute period is from two weeks to two months. At this time, heart failure is formed, since the pumping function is sharply reduced due to the loss of the area of necrosis from work. In 35% of patients during this period, Dressler's syndrome develops - an autoimmune reaction of the body in relation to necrotic tissues, leading to a sharp deterioration in the patient's condition. This condition is stopped by drugs that suppress the production of antibodies specific to the myocardium.
- Scarring period - begins with the end of the subacute period and lasts until the formation of a scar at the site of the necrosis focus. The properties of scar tissue are not at all similar to the properties of the heart muscle, the heart will no longer be able to perform its function in full - the result will be the formation of persistent heart failure, which will persist for life. There is a likelihood of thinning of the heart wall in the area of the scar, rupture of the heart with significant physical exertion.
Anginal and atypical forms of myocardial infarction
The division into forms occurs according to the main symptoms of the disease. The characteristic signs of a typical form of myocardial infarction are intense burning chest pain (medical definition - anginal), which radiates between the shoulder blades, in the arm, ribs or jaw and is not relieved by analgesic drugs. This condition is accompanied by arrhythmia, weakness, tachycardia, nausea, and excessive sweating. A heart attack with such typical manifestations is called an anginal form - after the name of the pain syndrome.

Anginal infarction is manifested by acute heart pain of high intensity
There are other forms in which the clinical manifestations do not at all coincide with the classic book picture of the disease. These include:
- the abdominal form of myocardial infarction - the symptom complex resembles acute pancreatitis. The patient complains of abdominal pain, bloating, nausea, hiccups, vomiting. Severe pain in this case, as in a typical heart attack, is not relieved by antispasmodics and analgesics;
- asthmatic - due to rapidly progressing heart failure, symptoms similar to bronchial asthma develop, the main of which is shortness of breath;
- the painless form is typical for patients with diabetes mellitus - due to the high blood glucose, pain sensitivity is muffled. This is one of the most dangerous forms, since the asymptomatic course contributes to late seeking medical help;
- cerebral, or brain form - it is characterized by loss of consciousness, dizziness, cognitive disorders, and perception disorders. In this case, myocardial infarction can easily be mistaken for a stroke;
- collaptoid form - as a result of cardiogenic shock and a sharp drop in blood pressure, a collapse occurs, the patient feels dizziness, darkening in the eyes, severe weakness, may lose consciousness;
- peripheral - characterized by a special irradiation of pain to the throat, limbs or fingers, the spine, while the pain in the heart is weak or absent;
- arrhythmic - the main symptom is a pronounced arrhythmia;
- edematous - the rapid development of heart failure leads to the appearance of extracardiac manifestations: swelling in the legs and arms, shortness of breath, ascites (fluid in the abdominal cavity).
Atypical forms can be combined with each other, as well as with anginal infarction.
Anatomical classifications
Since different parts of the heart have different blood supply, their lesion will have different manifestations and prognosis. According to the anatomy of the lesion, the following types of heart attacks are distinguished:
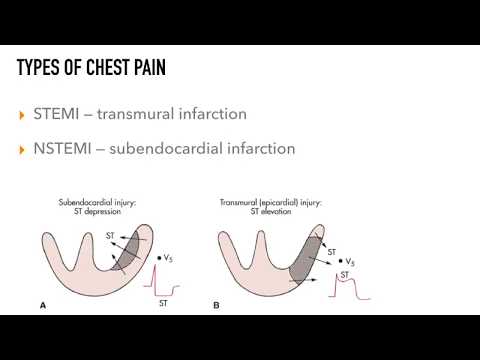
- transmural - the entire thickness of the heart muscle is affected by necrosis;
- intramural - the focus is located in the thickness of the wall, most often the left ventricle, while the endocardium and epicardium are not affected;
- subendocardial - the focus of necrosis is located in a narrow strip under the endocardium, often on the anterior wall of the left ventricle;
- subepicardial - does not affect the deep layers of the heart, it develops immediately under its outer shell - the epicardium.
Based on the anatomical location and size of the necrosis focus, large-focal myocardial infarction is isolated, it is also transmural, also called Q-infarction. The name comes from the specific ECG signs of this type of myocardial infarction - with it, the Q wave is preserved.

If the Q wave is detected on the ECG, they talk about transmural, or Q-infarction
The other three options refer to small focal lesions, do not have a Q wave on the cardiogram, and therefore are called non-Q infarctions.
Another classification takes into account the localization of the necrosis focus in the anatomical parts of the heart:
- left ventricular myocardial infarction is the most common. Depending on the affected wall, anterior, lateral, lower and posterior location is distinguished;
- isolated apex infarction;
- septal infarction - the affected area is the interventricular septum;
- myocardial infarction of the right ventricle is extremely rare, as well as damage to the posterior wall of the heart.
Mixed localizations are possible.
Diagnosis of the disease
Arbitration methods for making a diagnosis are ECG (electrocardiography), echocardiography (ultrasound examination of the heart), as well as the determination of specific markers of inflammation in the blood.
According to the ECG data, it is possible to determine the degree of myocardial necrosis, its type and the approximate depth of the formed defect, to assess the preserved conductivity, excitability and other properties of the heart muscle.
Echocardiography combines the classical ECG with ultrasound examination of the heart and the use of the Doppler effect to visualize the movement of blood flows within the heart. This mode allows you to see the hemodynamics, valvular insufficiency, and regurgitation of blood masses necessary for assessing the consequences of a heart attack. Echocardiography also allows you to determine the exact localization of the necrosis focus.
A biochemical blood test serves as the final confirmation of the diagnosis. After the destruction of myocardial cells, proteins and enzymes are released (troponin, CPK-MB, etc.). They testify to the high specificity of necrosis, i.e., the location of the focus in the myocardium.
All the listed classifications help to accurately determine the type of myocardial infarction, develop principles of approach to each of them, assess the required amount of treatment and subsequent rehabilitation, and sometimes give a prognosis with a high degree of reliability.
Video
We offer for viewing a video on the topic of the article.

Nikita Gaidukov About the author
Education: 4th year student of the Faculty of Medicine No. 1, specializing in General Medicine, Vinnitsa National Medical University. N. I. Pirogov.
Work experience: Nurse of the cardiology department of the Tyachiv Regional Hospital No. 1, geneticist / molecular biologist in the Polymerase Chain Reaction Laboratory at VNMU named after N. I. Pirogov.
Found a mistake in the text? Select it and press Ctrl + Enter.