- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Warts on the penis
The content of the article:
- Causes of occurrence
- Ways and likelihood of infection
- Symptoms
- Diagnostics of the warts on the penis
-
How to treat genital warts
Methods for removing genital warts
- The possibility of relapse
- Video
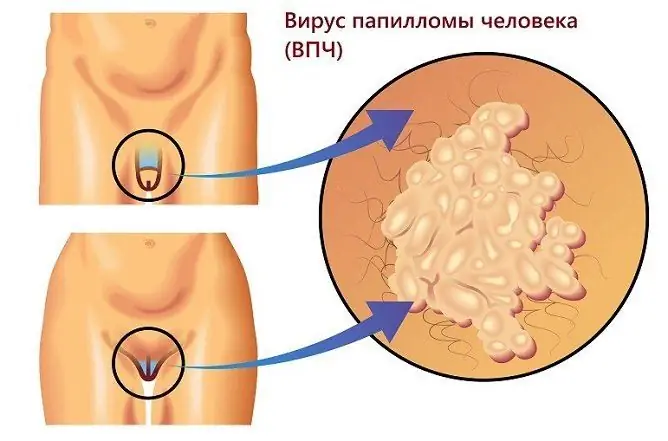
Warts on the penis, or genital warts, are benign neoplasms on the leg, flesh or pink, soft in consistency, of unequal size, prone to fusion. Their occurrence is associated with infection with the human papillomavirus (HPV) and decreased immunity in men. In more than half of cases, infection occurs through sexual contact. Treatment combines surgical methods and conservative therapy, which is symptomatic and restorative.
The photo gives an idea of genital warts.

Genital warts develop on the genitals as a result of papillomavirus infection
Causes of occurrence
Warts are caused by the human papillomavirus and are of several types:
- ordinary, or vulgar, often localized on the hands;
- flat, or youthful, are located on the skin of the face and hands;
- genital warts occur on the genitals, around the anus, in the groin folds.
There are also senile warts, or age-related keratomas, not associated with a viral infection, usually located on the neck, face, trunk. They look like dark growths covered with loose horny masses.
Warts on the penis are genital warts of viral origin. There are many strains of the virus, more than 40 of which cause the appearance of typical masses in the genital area in men. Most often these are 6 and 11 types of viruses.
Ways and likelihood of infection
The main route of infection is sexual. The likelihood of infection increases if the following predisposing factors are present:
- early sexual activity;
- a large number of sexual partners;
- unprotected sex.
The ingestion of HPV into the body does not always lead to clinical manifestations. Self-healing within 6-12 months or long-term asymptomatic carriage is possible. Warts on the genitals appear when the papillomavirus is activated, which occurs when immunity decreases, and this is facilitated by:
- prolonged hypothermia;
- excessive physical and emotional stress;
- alcohol abuse, tobacco smoking;
- viral, bacterial, fungal infections;
- trauma;
- oncological diseases;
- hormonal disorders;
- taking certain medications.
In more than half of patients, characteristic growths on the penis occur within 3 months from the moment of sexual contact with a partner infected with the human papillomavirus.
Symptoms
Genital warts can be single and multiple, small and significant in size. Usually, small pink nodules appear first, which, as the disease progresses, form growths in the form of papillae, resembling a rooster's comb or cauliflower in shape (see photo). They are soft to the touch and have a base or stem. Sometimes they reach several centimeters. Typical localization sites in men:
- coronal groove;
- the head of the penis;
- inner leaf of the foreskin;
- the mucous membrane of the urethra;
- scrotal skin;
- the area around the anus.
Often there are no complaints of itching or soreness. Bleeding and weeping are troubling with traumatization of neoplasms. Discomfort during urination is possible if condylomas are located in the urethra, and during bowel movements - if in the anal area.
Diagnostics of the warts on the penis
When warts appear on the penis, patients usually see a dermatologist. To make a diagnosis, the doctor:
- interviews the patient;
- finds out the history of the development of the disease;
- conducts an external examination;
- takes a scraping or smear-imprint for cytological examination;
- takes biopsy material for histological examination in case of suspicion of a malignant nature of the formation;
- prescribes blood sampling to determine the type of papillomavirus by polymerase chain reaction (PCR);
- examines for sexually transmitted infections.
For successful treatment, it is necessary to examine the sexual partner for the presence of HPV and diseases that are sexually transmitted. If genital warts are found, localized in the urethra, it may be necessary to consult a urologist and conduct ureteroscopy - examination of the canal using a special optical device.
How to treat genital warts
Therapy for genital warts is designed to solve the following main tasks:
- improve immunity;
- remove existing warts;
- prevent the appearance of new genital warts.
The virus exists in the human body in two forms: episomal, when it is outside the cell chromosome, and introsomal, when it is inserted into the cellular genome. The first is considered inactive and benign, the second is an aggressive form of parasitizing the virus, leading to the onset of clinical manifestations of the disease. The goal of treatment is to render the virus inactive.
| Therapeutic task | Characteristic |
| Boost immunity |
The activity of the virus in the human body, and hence the presence or absence of clinical manifestations, directly depends on the state of immunity. A decrease in the general resistance of the body is a prerequisite for the appearance of genital warts. It has been proven that natural immunity within two years is able to independently cope with the human papillomavirus that has entered the body in nine cases out of ten. In order to increase the effectiveness of the local immune response, antiviral and immunomodulating drugs are used: Allokin-alpha, Interferon, Groprinosin, Isoprinosine, Cycloferon, Viferon, Epigen Intim, Immunomax, Likopid, Aldara, etc. The form of their release is different: solution for injections, tablets, suppositories rectal, cream, spray. The dose of the drug, the frequency of use, the duration of treatment is determined by a specialist. To increase the effectiveness of therapy, several drugs are often prescribed simultaneously in different dosage forms. |
| Removal of genital warts |
There are various ways to remove existing formations: surgical, electrocoagulation, laser, cryodestruction with liquid nitrogen, using cauterization with chemicals. Treatment should not be limited only to the removal of existing condylomatous growths. It is necessary to treat complexly. Immunomodulatory, antiviral therapy often leads to regression of small warts and a reduction in the size of large warts. In addition, the destruction of warts without systemic treatment promotes the spread of infection to the adjacent skin and mucous membrane of the penis, increasing the possibility of recurrence of the disease. |
| Prevention | To prevent diseases caused by HPV, it is necessary to lead a healthy lifestyle, which contributes to an increase in non-specific immunity. The virus has a sexual route of transmission, so it is important to form the correct stereotype of sexual behavior: the choice of one sexual partner, the inadmissibility of casual relationships, the use of barrier contraception. For primary prevention, a four-component vaccine has been developed that is effective against oncogenic HPV strains - types 6, 11, 16 and 18 (Gardasil). In some countries, the vaccine is included in the mandatory vaccination schedule for girls aged 9 years and older as protection against cancer of the cervix, vagina and vulva. The World Health Organization recommends vaccinating not only girls, but also boys between the ages of 9 and 17. Vaccination is for prophylactic purposes only and is not used to treat a pre-existing disease. The greatest effect is achieved if the use of the vaccine is started before the onset of sexual activity. The course consists of 3 injections, injections are made into the deltoid muscle of the shoulder. The second and third vaccinations are given two months and six months after the first injection. Vaccination protects against infection with the most dangerous HPV strains: types 16 and 18 in men can cause anal and penile cancer, types 6 and 11 - genital warts and some potentially precancerous lesions. Until 2018, the introduction of the vaccine was recommended for people from 9 to 26 years old. In 2018, the use of a nine-valent vaccine (Gardasil 9), effective against 6, 11, 16, 18, 31, 33, 45, 52 and 58 strains of the virus, was allowed in patients aged 27-45 years. The vaccine does not contain mercury-containing compounds, live or dead viruses, but only virus-like particles that do not multiply in the human body. The number of side effects when using it is negligible. |

You cannot remove genital warts yourself, only a medical professional should do this.
Methods for removing genital warts
Methods of getting rid of genital warts are varied, each has its own advantages and disadvantages.
| Method | Feature, application |
| Surgical excision | Removal is performed with a scalpel under local or spinal anesthesia. The choice of pain relief depends on the size of the genital warts and their location. The use of an electrocoagulator or a Surgitron radio wave apparatus during surgical excision can reduce tissue trauma and promptly cauterize blood vessels: genital warts are well supplied with blood, and when removed, a bleeding wound surface is formed. |
| Electrocoagulation | Destruction of warts with alternating electric current. The basic principle of the method is to convert high-frequency current into thermal energy. The procedure is performed using an electrosurgical high-frequency apparatus. The impact on the vessels, the integrity of which is violated during the removal of neoplasms, leads to their wrinkling and stopping bleeding. |
| Radio wave exposure | Non-contact method of removing neoplasms using high frequency radio waves. The necessary effect occurs due to the heat generated in the tissue when it comes into contact with a special electrode that transmits high-frequency radio waves. Advantages of the method: sterility, bloodlessness, minimal trauma, good cosmetic effect during healing. |
| Cryodestruction | The method is based on the use of the destructive force of low temperature, forcing the liquid in living cells to freeze. The most common way to freeze genital warts is to use liquid nitrogen as a cooling solution. It is fed through a thin tube called a cryoprobe. The method provides the possibility of complete and accurate destruction of the formation, while the surrounding tissues are minimally damaged, bleeding does not develop. After the procedure, the lesions heal quickly, without the formation of rough scars. |
| Laser vaporization (evaporation) | To remove neoplasms, a carbon dioxide or neodymium laser is used: there is a very rapid evaporation of tissue and intracellular fluid, and then the complete combustion of the dry residue. The negative aspects of the procedure include the lack of material for histological examination. |
| Cauterization with chemicals | For destruction, special keratolytic preparations are used containing a mixture of organic and inorganic acids (Solkoderm, Kollomak, etc.). It is not recommended to remove genital warts on your own. The application of the agent on condylomas should be carried out by a dermatovenerologist in the treatment room of the polyclinic. This is done using an applicator or a glass capillary without affecting the healthy surrounding tissues. The presence of numerous or significant in size formations is not carried out simultaneously, but in several stages with a certain time interval (2-3 weeks). |
| Cytotoxic destruction | The drugs (Podophyllin, Kondilin, 5-fluorouracil) suppress DNA synthesis and cell proliferation. Condilin (the active substance is podophyllotoxin) can be used by the patient independently, but with all precautions: apply with a cotton or plastic swab strictly on the formation, without affecting the surrounding tissues. Development of local inflammatory reactions is possible. |
The choice of the method is carried out by a specialist. It takes into account the nature and localization of warts, the state of the patient's immune system, and the presence of concomitant pathology.
The possibility of relapse
There is a risk of recurrence after removal of genital warts by any method. To minimize it, you must:
- complex treatment;
- dispensary observation after removal of formations;
- examination and treatment of the sexual partner;
- compliance with preventive measures.
Only the fulfillment of all the requirements will make it possible to achieve a lasting positive result.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.