- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Decoding a general blood test in children
The content of the article:
- Erythrocytes
-
Leukocytes
- Neutrophils
- Lymphocytes
- Monocytes
- Eosinophils
- Basophils
- Platelets
Deciphering a blood test in children is a difficult task that a specialist must deal with. Our article provides only general information for reference, not sufficient for a diagnosis.
A general blood test is the most common laboratory test, which allows you to narrow the search results for suspected diseases, recognize pathology in time, conduct a preliminary diagnosis of the state of organs and systems, and draw the first conclusions about the state of the patient's body.
The results of general analysis play a special role in pediatrics, because children often cannot express their complaints. There are a number of indicators by which it is possible to identify possible disturbances in the activity of the body using a general blood test.
The norms of a general blood test in children depend on age, since in connection with the growth of the child and the formation of the body, the composition of the blood changes. To interpret the obtained indicators, you can consult the tables for decoding the general blood test in a child, in which several age groups are distinguished, however, it should be borne in mind that only a specialist can correctly evaluate the results obtained. The norms for blood counts differ depending on the method and units of measurement, and therefore may differ from laboratory to laboratory.

For a general analysis, blood from children is taken from a finger
For a general analysis, take blood from a finger. It is recommended to donate blood in the morning, on an empty stomach, 8 hours after the last meal (acceptable in the afternoon, but not earlier than four hours after a meal).
A general blood test in a child includes determining the composition and concentration of blood cellular elements - erythrocytes, leukocytes and platelets, as well as calculating a number of indices. Deciphering the blood test in children allows you to determine the content of each type of blood elements, estimate the volume ratio of cellular elements and the liquid part of the blood, and get an idea of the concentration of hemoglobin in the child's body.
Erythrocytes
Erythrocytes (from the Greek erythros - red and kytos - vessel, cell) are red blood cells containing hemoglobin. The place of their formation and growth is the bone marrow. The main function of erythrocytes is to transport oxygen and carbon dioxide between the lungs and tissues of other organs. Deciphering a blood test in children allows you to assess the indicators of the number of red blood cells relative to the generally accepted norm:
- newborns (up to 2 weeks) - 3.9-5.9 million / μl;
- up to a month - 3.3-5.3 million / μl;
- up to 3 months - 3.5-5.1 million / μl;
- up to 6 months - 3.9-5.5 million / μl;
- up to 9 months - 4-5.3 million / μl;
- up to 1 year - 4.1-5.3 million / μl;
- up to 2 years - 3.8-4.8 million / μl;
- up to 5 years - 3.7-4.9 million / μl;
- up to 6 years - 3.8-4.9 million / μl;
- up to 10 years -3.9-5.1 million / μl;
- up to 15 years: girls - 3.8-5, boys - 4.1-5.2 million / μl;
- up to 18 years old: girls - 3.9-5.1, boys - 4.2-5.6 million / μl.

The number of red blood cells in the blood of a child rises with dehydration
A decrease in the number of red blood cells (erythropenia) is observed in conditions accompanied by a decrease in their formation or increased destruction, and may be a sign of anemia. An increase in the concentration of erythrocytes in a child (erythrocytosis) most often indicates dehydration of the child's body, which can develop with vomiting, diarrhea, high temperature. A persistent increase in the number of erythrocytes accompanies diseases of the lungs, heart, liver, kidneys.
The general (clinical) blood test includes erythrocyte indicators:
- the absolute content of erythrocytes - according to the number of erythrocytes, a preliminary assessment of the activity of the hematopoietic system can be made. In clinical practice, the total number of erythrocytes in 1 microliter or cubic millimeter of blood is determined;
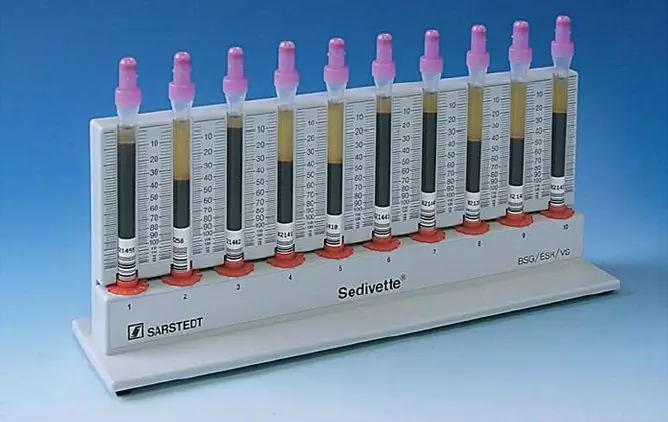
- ESR (erythrocyte sedimentation rate) - erythrocytes have the ability to stick together and settle under the influence of gravity while keeping the blood uncoiled. The erythrocyte sedimentation rate depends on many factors: blood viscosity, physical and chemical properties of erythrocytes, the content of bile pigments and acids in the blood, acid-base balance, cholesterol and lecithin balance. Acceleration of erythrocyte sedimentation accompanies infectious diseases, inflammatory processes, the development of malignant neoplasms. Slowdown is observed with hyperhidrosis, gastroenteritis, tetanus, jaundice, encephalomyelitis, overwork. Increased ESR in newborns is a physiological phenomenon;
- study of the level of reticulocytes - precursors of erythrocytes, young immature cells, the number of which reflects the rate of erythrocyte formation. Deciphering the blood test in children allows you to assess the saturation of the body with oxygen and determine the speed at which the blood composition is renewed;
- physiological hemoglobin (Hb) level- the composition of erythrocytes includes the respiratory blood pigment hemoglobin, which consists of protein and iron atoms. With a deficiency of hemoglobin in the blood, metabolism is disturbed, oxygen transport is impeded. A high level of hemoglobin in the blood of a child can be a symptom of cardiopulmonary insufficiency, heart disease, intestinal obstruction, liver cancer, blood clots, erythrocytosis, polycystic kidney disease. An increase in hemoglobin in the blood occurs as a result of burns, with excessive physical exertion. An increase in the level of glycated hemoglobin is observed in diabetes mellitus and iron deficiency states. Low hemoglobin may indicate the presence of chronic diseases, anemia, blood diseases, accompanied by the destruction of erythrocytes, internal bleeding. Deciphering a blood test in children allows you to track metabolic processes in the body,determine the content of hemoglobin in the red blood system, assess the risks of complications of diabetes.
- color index - characterizes the content of hemoglobin in one erythrocyte. A decrease in the color index accompanies different types of anemias, and can be observed with blood loss. An increase in the color index occurs with hyperchromic anemia, which develops with a deficiency of vitamin B1.
Leukocytes
Leukocytes (from the Greek. Leuko's - white and kytos - vessel, cell) - white blood cells that perform immune function. White blood cells are produced in the lymph nodes and bone marrow. With a number of pathologies, the decoding of a blood test in children shows characteristic changes in the level of leukocytes.
A decrease in the number of leukocytes can be a symptom of hepatitis, rubella, rheumatism, lupus erythematosus, often observed with hypovitaminosis, general depletion of the body.
An increase in the level of leukocytes accompanies inflammatory and purulent diseases. In infants, leukocytosis is a normal stage in the formation and development of the immune system.

Leukocytes, or white blood cells, perform a protective function in the body
The leukocyte formula indicates the relative percentage of different types of leukocytes in a blood test. The ratio of leukocytes in infants can fluctuate during the day; to obtain an accurate result, the results are assessed according to absolute values. Leukocyte indicators should be assessed together with other indicators of the blood system and the general condition of the child, therefore, only a doctor can correctly decipher the leukocyte formula.
The number of leukocytes in the blood of a child, depending on age:
- up to a year - 6-17.5 thousand / μl;
- up to 3 years - 6-17 thousand / μl;
- up to 8 years old - 5-14.5 thousand / μl;
- up to 10 years - 4.5-13.5 thousand / μl;
- over 10 years old - 4.5-11 thousand / mcl.
There are five subgroups of leukocytes, each of which has a specific function in the body.
Neutrophils
Neutrophils surround microbial agents, absorb and break them down within themselves, protecting the body from bacteria, fungi and protozoa. Depending on the stage of maturation, neutrophils are divided into subgroups (stab, segmented, myelocytes, metamyelocytes). The ratio of subgroups of neutrophils to each other is called the neutrophilic formula, its shift to the left with an increase in the number of neutrophils is a sign of an inflammatory process. A sharp deviation of the level of neutrophils from normal values causes a weakening of immunity, leads to the development of bacterial and viral diseases.
Lymphocytes
Lymphocytes are responsible for the immune response and immune memory. They destroy sick cells infected with viruses, tumor cells, and fight chronic infections. Lymphocytes differentiate into subgroups with different functions: T cells, B cells, NK cells (natural killer cells).
Monocytes
Monocytes absorb particles of foreign physical agents and foreign cells in the blood, and are responsible for purifying the blood from foreign microorganisms. A decrease in the level of monocytes in a child may be due to the development of anemia, purulent lesions, leukemia. The decrease in monocytes can be influenced by surgical operations, taking steroid drugs.
Eosinophils
These cells are responsible for the fight against particles that carry allergens in the focus of inflammation, activate cell receptors responsible for antiparasitic immunity, accumulate and release inflammatory mediators, and participate in the utilization of histamine. Eosinophilia in a child can be a symptom of an allergic process (hay fever, allergic diathesis, bronchial asthma), helminthic and protozoal invasion. A decrease in the level of eosinophils is due to the development of inflammatory and purulent processes, intoxication of the body with heavy metals.
Basophils
The smallest group of leukocytes. They help to detect and destroy foreign particles in the body, regulate blood coagulation and vascular permeability. Despite the fact that the leukocyte formula in children changes with age, the rate of basophils remains unchanged. An increase in the level of basophils can occur for various reasons: chickenpox, myeloid leukemia, nephrosis, Hodgkin's disease, hypothyroidism, tuberculosis, ulcerative colitis, hemolytic anemia, rheumatoid arthritis. The cause of increased basophils can also be a condition after removal of the spleen, allergic reactions, taking hormonal drugs.
Platelets
Platelets (Greek thrombos - clot and kytos - vessel, cell) are platelets that support the work of blood vessels, are responsible for blood clotting and provide regeneration of damaged vessels. They are secreted in the red bone marrow from the plasma of its cells (megakaryocytes). The platelet count characterizes the body's ability to stop bleeding. An increased number of platelets creates a risk of thrombus formation, it is observed in acute and chronic inflammatory processes, tuberculosis, oncological diseases, lymphogranulomatosis, after undergoing surgical interventions. High blood platelet counts can also be caused by certain medications. A decrease in the number of platelets leads to fragility of blood vessels and increased bleeding.

A lowered number of platelets in the child's blood causes bleeding
Thrombocritis is the proportion of blood volume occupied by platelets in the total volume of circulating blood. Thrombocritis determines the percentage of platelet mass in the volume of whole blood. This indicator, when decoding a blood test in children, allows you to assess the degree of risk of thrombosis or bleeding.
The normal platelet count depends on the age and sex of the child:
- newborns (up to 2 weeks): boys - 218-419 thousand / mcl, girls - 144-449 thousand / mcl;
- 2 weeks - 2 months: boys - 248-586 thousand / mcl, girls - 279-571 thousand / mcl;
- 2 months-six months: boys - 229-562 thousand / mcl, girls - 331-597 thousand / mcl;
- half a year - 2 years: boys - 206-445 thousand / μl, girls - 214-459 thousand / μl;
- 4 years - 6 years: boys - 202-403 thousand / μl, girls -189-394 thousand / μl;
- over 7 years old - 150-400 thousand / μl in girls and boys.
YouTube video related to the article:

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.