Endometrial glandular polyp: causes of formation, treatment, complications
The content of the article:
-
What is an endometrial polyp
- Uterine membranes
- How does the build-up form
- Types of polyps
- Features of the glandular polyp
-
The reasons for the development of pathology
- Functional form
- Basal form
- Symptoms
-
Diagnostics
- Laboratory research methods
- Instrumental research methods
-
Therapy
Treatment of the endometrial glandular polyp after removal
- Complications
- Video
The glandular polyp of the endometrium is one of the most common types of pathology, along with the glandular-fibrous form. This type of neoplasm is typical for women of reproductive age and, on average, accounts for 30–40% of all cases.
Attention! Photo of shocking content.
Click on the link to view.
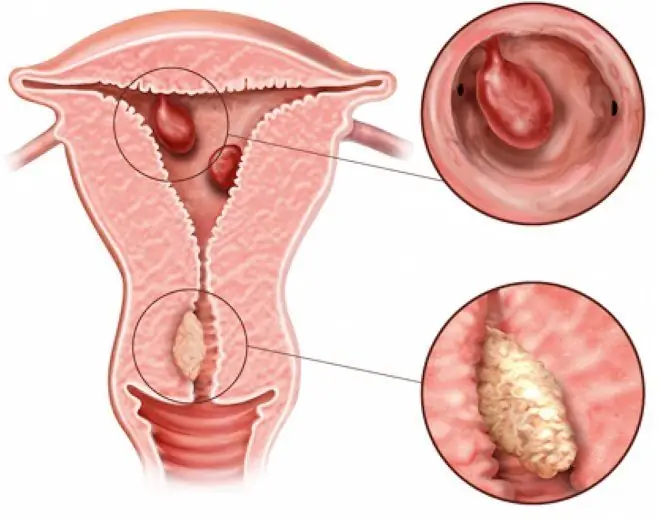
Endometrial polyp is a common pathology in women of the reproductive and climacteric period and is a type of glandular cystic or atypical endometrial hyperplasia. It has the appearance of a towering formation (growth) and may consist of adenomatous (glandular) cells and connective tissue cells.
Clinically, a neoplasm is able to remain unnoticed for a long time, without causing any symptoms. This poses a great danger, since there are cases of malignancy - the degeneration of a benign polyp into a malignant form.
What is an endometrial polyp
Uterine membranes
The endometrium is one of the three lining of the uterus. The outer membrane is called perimetry (or serous membrane). The middle, largest membrane of the uterus - the myometrium, consists of smooth muscle cells (myocytes).

The lining of the uterus consists of three layers
The inner shell is the endometrium. It is represented by two layers of cells: basal and functional. The cells of the basal layer have a small number of receptors for hormonal substances, due to which they are practically not subject to hormonal influences. The basal layer is the basis for the overlying functional layer.
The most superficial layer is functional, the cells of which are maximally sensitive to any hormonal changes in a woman's body. It is rejected along with menstrual blood during menstruation, and after it is over, it is completely restored using the basal layer.
How does the build-up form
The polyp is formed only from the mucous membrane of the uterus - the endometrium, as a result of hyperplastic processes. Due to the intensive growth, the endometrium grows in height, forming a nodular neoplasm, consisting of a leg and a body.
As the growth progresses, vessels begin to grow, providing blood supply. Thus, its size can reach from a few millimeters to 5-6 centimeters or more.
Types of polyps
Since the endometrium contains several types of cells, a neoplasm is formed with a predominance of one of them. Allocate polyps:
- adenomatous (glandular): growth with a predominance of glandular cells;
- fibrous: the formation is formed by the cells of the connective tissue;
- glandular fibrous: the composition includes equally both connective tissue cells and glandular cells.
Features of the glandular polyp
The glandular polyp of the endometrium is more represented by glandular cells, to a lesser extent by stromal cells.
Depending on the layer from which it was formed, there are two types:
| Polyp type | Description |
| Basal (true) | It is formed from the endometrial layer of the same name. Unlike the second type, it is practically immune to sex hormones and does not change its structure |
| Functional (pseudopolyp) | It is formed from the most superficial - functional layer, which must be rejected during menstruation. However, if the area of unseparated endometrium for some reason remains, a growth is formed on it |
A functional growth is highly sensitive to any hormonal changes, so its shape and structure can change along with a healthy endometrium throughout the entire menstrual cycle.
By histological type, pseudopolyps are divided into the following types:
- proliferative;
- hyperplastic;
- secretory.
Glandular neoplasms are extremely rare and are considered the most dangerous, since they are prone to malignant transformation, especially in postmenopausal women, against the background of neuroendocrine and metabolic disorders.
The number of polyps in the uterus can also indirectly indicate the risk of transformation. So, single neoplasms rarely malignant (1-2%), multiple - more often (20%), diffuse (familial) malignant very often (80-100%).
The reasons for the development of pathology
The reasons for the formation of a functional and basal polyp are somewhat different.

The development of a functional and basal endometrial polyp has different reasons.
Functional form
Since the functional layer is most susceptible to hormonal changes, the formations of the functional type increase against the background of hormonal disorders, namely with hyperestrogenism.
Dyshormonal conditions can be caused by:
- frequent stress;
- obesity, hypertension;
- diabetes mellitus, thyroid disease and other neuroendocrine pathologies;
- hyperestrogenism, which has arisen against the background of inadequate therapy with estrogen-containing drugs;
- trauma and inflammation of the uterine lining (endometritis);
- some other gynecological diseases.
Basal form
The basal layer is practically not subject to hormonal influences, therefore, dyshormonal states do not play a key role in the development of a basal endometrial polyp.
A common cause of occurrence is trauma to this layer and some other pathologies:
- abortion;
- fractional diagnostic curettage;
- long-term presence of the intrauterine device in the uterine cavity, its incorrect installation;
- biopsy of the inner walls of the uterus without high-quality sterilization of instrumentation, its inaccurate conduct;
- diseases of the immune system: allergies, autoimmune pathologies, especially involving the vascular wall, immunodeficiency states;
- inflammatory processes in the uterus caused by sexually transmitted infections and some other pathogens;
- complicated obstetric anamnesis (miscarriages, termination of pregnancy, complicated labor).
Symptoms
The onset of neoplasm formation almost always goes unnoticed, since during this period the woman does not observe any symptoms, and ultrasound research methods cannot visualize it.

One of the symptoms of pathology is pulling pain in the lower abdomen
Reaching a certain size, a polyp can provoke the following symptoms:
- intense soreness before and during menstruation;
- the appearance of a bloody discharge long before the onset of menstruation (intermenstrual bleeding). A woman can detect spotting on her underwear on any of the days of the menstrual cycle: at the beginning, in the middle or just before the menstruation itself;
- delayed menstruation followed by profuse menstrual flow;
- pulling pain in the lower abdomen;
- dyspareunia (pain during intercourse);
- spotting after intercourse, exercise, stress;
- lack of a regular menstrual cycle.
In menopausal women, bloody discharge from the genital tract may be observed. At this age, this is a formidable sign, which often indicates oncological processes in the gynecological sphere.
Diagnostics
If at least one of the symptoms appears, you should immediately contact your gynecologist. Based on complaints, anamnesis, the results of a bimanual gynecological examination and examination in mirrors, the doctor will be able to suspect this pathology.
Laboratory research methods
To make a diagnosis, the doctor prescribes a study of the hormonal background: determining the amount of estrogen, progesterone, follicle-stimulating hormone, luteinizing hormone, thyroid hormones, adrenal glands and others. The material is taken on different days of the cycle.
Additionally, a study of tumor markers can be carried out, especially in menopausal and postmenopausal women.
Instrumental research methods
Instrumental research methods are mandatory, they allow visualizing the neoplasm, conducting a biopsy with further examination of the tissue for benignity or malignancy.

Pathology is often detected during ultrasound
The following types of instrumental studies are used:
- ultrasound examination of the pelvic organs (ultrasound). The method allows you to assess the state of the endometrium, the presence of hyperplastic processes and neoplasms in it;
- endoscopic examination using a hysteroscope (hysteroscopy). A hysteroscope is a special optical device that is inserted into the uterine cavity and allows a detailed examination of its mucous membrane.
During hysteroscopy, it is possible to conduct a targeted biopsy of the neoplasm for its subsequent cytological and histological examination.
Another option is fractional diagnostic curettage. Fragments of tissue isolated during the procedure are also sent to the laboratory for assessment of cellular and tissue composition.
Therapy
Most often, a glandular polyp is treated surgically.
During the operation, the gynecologist inserts a hysteroscope into the uterine cavity, after the outgrowth is visualized in the field against the background of a pathologically unchanged endometrium, it is targeted mechanically or using laser ablation, electrocoagulation, etc.

Removal of the polyp is usually done during a hysteroscopy
If at the diagnostic stage, fractional diagnostic curettage was performed and the polyp turned out to be functional, further surgical intervention is not required.
Treatment of the endometrial glandular polyp after removal
This is an important step in therapy. In order to restore hormonal levels, the following are used:
- gestagens (preparations containing progesterone in their composition): Micronor, Levonorgestrel, Dyufaston, Utrozhestan;
- gestagen-estrogen drugs or combined oral contraceptives: Yarina, Zhanin, Diane-35.

For treatment, drugs containing progesterone are prescribed, in particular Utrozhestan
The scheme and duration of therapy is determined by the gynecologist individually for each patient.
If the results of the cytological examination of the material taken during the biopsy testify in favor of malignancy and there are signs of an oncological process, the treatment differs from the usual and must be carried out by an oncologist-gynecologist.
Complications
Timely and adequately untreated glandular polyp can cause the following complications:
- infertility, miscarriage, placental abruption, fetal hypoxia during pregnancy;
- metrorrhagia (uterine bleeding) with the development of anemia;
- accession of infection or impaired blood supply with the development of necrosis;
- malignancy, adenomatous transformation.
For the early detection of hyperplastic processes of the endometrium and other pathologies of the gynecological sphere, it is necessary to visit a gynecologist regularly (at least once a year), try to eliminate risk factors, and treat gynecological diseases in a timely manner.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.