- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Endometrial hyperplasia
The content of the article:
- Causes and risk factors
- Forms of the disease
- Endometrial hyperplasia symptoms
- Features of sexual function in endometrial hyperplasia
- Diagnostics
- Treatment of uterine hyperplasia
-
Diet food for endometrial hyperplasia
Sample menu for patients with endometrial hyperplasia:
- Traditional methods of treatment of endometrial hyperplasia
- Potential consequences and complications
- Forecast
- Prevention
Endometrial hyperplasia - excessive growth of the endometrium (the inner layer of the uterus), accompanied by an increase in its volume and thickness.
Pathology is an urgent problem of modern gynecology, since hyperplastic processes in the endometrium tend to progress and are capable of undergoing malignant transformation.

Causes and risk factors
The pathological mechanism of the development of endometrial hyperplasia is based on a violation of the hormonal balance in a woman's body, namely, a decrease in the level of progesterone with an increased level of estrogen. At the same time, ovulation can be preserved, or it can be absent.
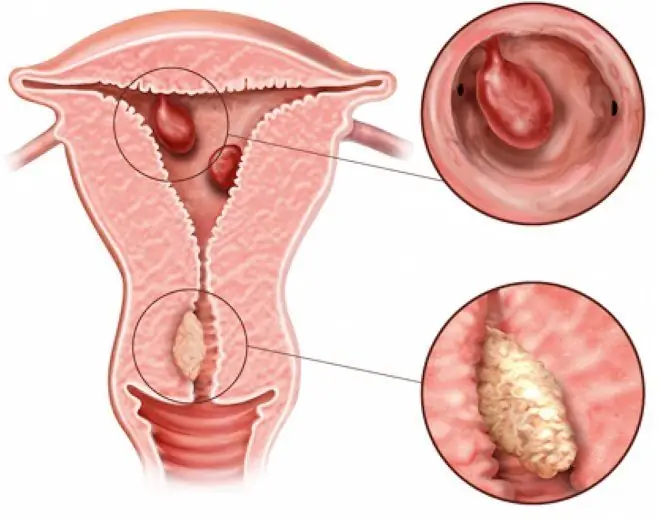
The endometrium, lining the uterine cavity from the inside, consists of the basal and superficial layers. During menstrual bleeding, the surface layer is rejected, and then during the next cycle it is again formed from the cells of the basal layer.
During each menstrual cycle, there are three phases of the state of the endometrium:
- Proliferation phase. Under the influence of estradiol, the cells of the basal layer begin to actively divide. This leads to the formation of a new loose surface layer. It quickly thickens, and the elongated tubular glands located in it lengthen.
- Secretion phase. After ovulation, a gland of temporary secretion is formed at the site of the bursting follicle - the corpus luteum, which secretes progesterone. Under the influence of progesterone, there is an increase in the tortuosity of the glands, as well as a gradual expansion of their lumen. Due to the increase in volume, stromal cells approach each other. The secretory activity of the glandular tissue is enhanced.
- Menstruation. If pregnancy has not occurred, then the corpus luteum undergoes regression. This process is accompanied by a sharp decrease in the concentration of estradiol and progesterone, which becomes the reason for the rejection of the surface layer of the endometrium and the occurrence of menstrual bleeding.
Thus, the regulation of cyclical changes in the endometrium in the first phase of the menstrual cycle is regulated by estrogens (responsible for cell proliferation), and in the second - by progesterone (inhibits proliferation activity and activates secretion).
Against the background of an increased level of estrogen in the blood, the secretory phase is not expressed clearly enough or is completely absent. Therefore, in the second phase of the menstrual cycle, the endometrial cells continue their active division, which normally should not be. This process leads to endometrial hyperplasia.
Endometrial hyperplasia can occur in women at any age when exposed to risk factors, but it is most often observed during the transition periods of life, accompanied by significant changes in hormonal levels (the period of the formation of menstrual function, premenopausal period), i.e., during periods of hormonal changes.
The emergence of hyperplastic processes in the endometrium can be triggered by the following factors, which are called genital:
- early onset of menstruation;
- late onset of menopause;
- abortion;
- lack of childbirth;
- refusal of hormonal contraception;
- gynecological operations, including curettage of the uterine cavity;
- polycystic ovary syndrome (multifollicular ovarian syndrome);
- uterine fibroids;
- endometritis;
- endometriosis;
- hormone-producing ovarian tumors;
- inflammatory diseases of the urogenital tract, especially those of a chronic nature;
- congenital anomalies of the organs of the reproductive system;
- therapy with tamoxifen or estrogen-containing drugs.
In addition, there are extragenital factors that increase the risk of developing endometrial hyperplasia. These include: mastopathy, diseases of the liver, adrenal glands, thyroid gland, obesity, diabetes mellitus, arterial hypertension.
Forms of the disease
Depending on the characteristics of histological changes in the inner layer of the uterus, the following forms of pathology are distinguished:
- glandular hyperplasia of the endometrium - proliferation of glands prevails; their shape is not the same, and the location is uneven. The division of the endometrium into basal and functional layers disappears, the border between the muscle and the inner layer of the uterus becomes indistinct;
- glandular cystic hyperplasia of the endometrium (adenomatosis) - some of the enlarged glands become cystic enlarged;
- atypical endometrial hyperplasia - there is a decrease in the number of stromal elements, polymorphism of the nuclei is observed, more intense proliferation processes.
- endometrial polyps - a focal form of hyperplasia, in which the integumentary and glandular epithelium grows in a certain area of the endometrium.
In turn, endometrial polyps, depending on the structural features, are divided into several types:
- glandular - come from the cells of the basal layer of the endometrium;
- glandular fibrous - characterized by the presence of a connective tissue stroma;
- fibrous - are a connective tissue formation in which there are no glands or are present in a very limited number.
Polyps and atypical endometrial hyperplasia are precancerous conditions. According to statistics, in the absence of timely and adequate treatment, 10-14% of them degenerate into endometrial cancer. Glandular cystic and glandular hyperplasia of the endometrium are malignant much less frequently. The risk of malignancy increases with inadequate hormone therapy, recurrent course of the disease and repeated curettage of the uterine cavity.
Endometrial hyperplasia symptoms
The main symptom of endometrial hyperplasia is dysfunctional uterine bleeding, which in most cases occurs after a delay in menstruation for a period of 1 to 3 months. By nature, these bleeding can be profuse, profuse or moderate, short-term or prolonged.
In patients with no obvious endocrine pathology and with normal body weight with endometrial hyperplasia, the regularity of menstrual cycles can be maintained, and the pathology at the same time manifests itself in abundant and prolonged, over 7 days, menstrual bleeding (hypermenorrhea, menorrhagia).
Approximately 25% of patients with endometrial hyperplasia have anovulatory uterine bleeding, and 5-10% have metrorrhagias - irregular uterine bleeding not associated with menstruation.
Another common symptom of endometrial hyperplasia is intermenstrual bleeding.
In 50% of cases, endometrial hyperplasia is combined with obesity, 75% of them show signs of virilization:
- coarsening of the voice;
- male pattern hair growth;
- enlargement of the clitoris.
In patients with normal body weight, endometrial hyperplasia is combined with manifestations of virilization in no more than 30% of cases.
Almost all patients with endometrial hyperplasia suffer from secondary infertility, recurrent miscarriage, mastopathy, chronic inflammatory diseases of the reproductive system, endometriosis.
Features of sexual function in endometrial hyperplasia
With endometrial hyperplasia, sexual life outside of periods of bleeding is not contraindicated. However, many women avoid it, as their coitus is accompanied by soreness in the lower abdomen. The selection of the most optimal position, the accuracy of the sexual partner and a long foreplay allow you to improve your sex life.
After intercourse, about every second patient has slight (so-called smearing) bleeding, accompanied by paroxysmal aching pain in the lower abdomen.
Diagnostics
Diagnosis of endometrial hyperplasia is carried out on the basis of the patient's complaints, anamnesis data, general and gynecological examinations, the results of laboratory and instrumental studies.
Interrogating the patient, the doctor specifies the age of the onset of menarche, the peculiarities of the menstrual cycle (after what time it was established, its duration, regularity, profusion and duration of menstrual bleeding, the presence of bloody discharge outside of menstruation). After collecting the history, a gynecological examination (bimanual and with the use of mirrors) is performed.
To assess the uniformity, thickness and structure of the endometrium, ultrasound of the pelvic organs is performed. This study allows not only to assess the state of the inner layer of the uterus, but also to identify other possible gynecological pathology (myomatous node, multifollicular ovarian syndrome, ovarian cysts, tumor processes).
If you suspect endometrial hyperplasia, ultrasound is recommended to be performed on the 5-7th day of the menstrual cycle (for uterine bleeding, the study is carried out on any day). Normally, in women of childbearing age, the thickness of the endometrium in the first phase of the menstrual cycle does not exceed 7 mm. After the onset of menopause, the thickness of the inner layer of the uterus should not be more than 4-5 mm.
Ultrasound can detect hyperplastic processes in the uterine cavity in about 70-80% of cases based on the following signs:
- an increase in the thickness of the endometrial layer;
- heterogeneity of its structure;
- the presence of echogenic inclusions in it.
In some cases, an aspiration biopsy of the endometrium with subsequent cytological examination of the resulting tissue is indicated. However, this study does not provide high diagnostic accuracy, so most gynecologists recommend diagnostic curettage and hysteroscopy instead. These methods are considered the gold standard in the diagnosis of uterine hyperplasia and allow a correct diagnosis in more than 95% of cases.
Hysteroscopy is an endoscopic diagnostic method that makes it possible to examine the internal cavity of the uterus using a special optical system, which is introduced into the uterus through the cervical canal. The advantages of hysteroscopy are:
- the ability to visually assess the state of the endometrium and identify any intrauterine pathology;
- low invasiveness of the procedure, due to which it is easily tolerated by patients;
- the ability to perform curettage of the uterine cavity under visual control, which minimizes the risk of complications (uterine perforation, damage to the basal layer of the endometrium).
During the curettage of the uterus, sections of endometrial tissue are taken for subsequent histological analysis. Curettage of the uterine cavity is not only a diagnostic, but also a therapeutic procedure, as it helps to stop uterine bleeding.
If you suspect the presence of metabolic syndrome or multifollicular ovary syndrome, blood tests are prescribed to determine the concentration of hormones (thyroid, adrenal glands, follicle-stimulating hormone, luteinizing hormone, estradiol, testosterone, progesterone).
Considering that hyperplastic processes in the uterus are often combined with mastopathy, mammography and ultrasound of the mammary glands are performed. If indicated, the patient is consulted by a mammologist.
Differential diagnosis of uterine hyperplasia is carried out with the following diseases:
- malignant tumors of the uterus (cancer of the body of the uterus, adenocarcinoma);
- submucosal fibroma of the uterus;
- polyposis;
- adenomyosis.
Treatment of uterine hyperplasia
The tactics of treating uterine hyperplasia is determined by many factors (the age of the patient, the desire to have children, the nature of the disease).
Girls under 20 years old with endometrial hyperplasia are prescribed cyclic hormone therapy with estrogens and progesterone for at least six months. As a rule, biphasic oral contraceptives are selected for this purpose. Such therapy stabilizes the endometrium and prevents uterine bleeding.
For women of childbearing age, endometrial hyperplasia is treated with three to four courses of cyclic administration of estrogens and progestins, after which a second endometrial biopsy is performed.
When the patient is planning a pregnancy and there is no ovulation, her medication is stimulated. If pregnancy is undesirable, cyclic hormone therapy is continued.
During the periods of perimenopause and postmenopause, the treatment of endometrial hyperplasia is carried out with progesterone preparations for 3-6 months.
Persistence of endometrial hyperplasia after 3-6 months of conservative treatment significantly increases the risk of developing uterine cancer. Therefore, in such cases, surgical treatment is recommended - amputation of the uterus (hysterectomy).
In case of glandular hyperplasia of the endometrium, the installation of an intrauterine progestogen-containing spiral "Mirena" has a good therapeutic effect.
In women over 35, antagonists of gonadotropin-releasing hormone (GnRH) can be used, which cause an artificial temporary menopause and amenorrhea in patients.
With prolonged or profuse uterine bleeding, treatment of endometrial hyperplasia begins with hemostasis (for this purpose, curettage of the uterine cavity is undertaken, uterotonics are prescribed), blood loss replenishment (infusion of electrolyte solutions, glucose, dextran is performed, according to indications of blood transfusion) and correction of post-hemorrhagic anemia).
Along with hormone therapy, patients are prescribed vitamin preparations, physiotherapy procedures (electrophoresis, acupuncture), and correction of iron deficiency anemia.
Diet food for endometrial hyperplasia
Properly organized medical nutrition plays an important role in the treatment of endometrial hyperplasia. To reduce cell proliferation, foods rich in antioxidants (tocopherols, ascorbic acid, bioflavonoids) should be included in the diet. These products include: carrots, broccoli, beets, zucchini, Brussels sprouts, legumes, figs, dried apricots, dried pears, apples, citrus fruits; nuts, strawberries, sea buckthorn, blackberries, black currants, rosehip broth.
The diet should include foods that help suppress excess estrogen. These are all types of cabbage, celery, pumpkin, garlic.
At least three times a week, it is recommended to eat fatty fish (mackerel, beluga, salmon, herring, salmon), rich in omega-3-polyunsaturated fatty acids, which have a pronounced oncoprotective effect. Other sources of omega-3-polyunsaturated fatty acids in the body are flaxseed and sesame oil, walnuts, and flax seeds.
Undesirable for endometrial hyperplasia are: red meat, eggs, fried foods, animal fats, margarine, flour products, yeast, sweets, carbonated sweet drinks, coffee, hot spices.
Food should be taken in small portions 4-5 times a day. The calorie content of the diet depends on the weight, height, age and lifestyle of the patient; in the presence of obesity, the daily caloric content of the diet should be reduced by 250-300 kcal until body weight normalizes.
Sample menu for patients with endometrial hyperplasia:
- Breakfast: protein omelet with green onions or green peas, a slice of rye bread, tea with honey and lemon.
- Second breakfast: a few slices of fresh pineapple or any seasonal fruit.
- Lunch: beetroot with kefir, fresh vegetable salad, steamed fish, rice, a slice of bread with bran, dried fruit compote or rosehip broth.
- Afternoon snack: a pear, a handful of walnuts, or a few dried apricots.
- Dinner: curd-rice casserole or carrot salad with prunes, herbal tea.
- Late dinner: A glass of natural yogurt without additives or kefir.
Traditional methods of treatment of endometrial hyperplasia
There are many recipes for traditional medicine for the treatment of endometrial hyperplasia. Some of them are quite effective, but there are also those that can worsen the state of health, including promoting tumor activity, therefore, traditional medicine can be used only in agreement with the attending physician and under his supervision.
The following tools are most commonly used:
- alcohol tincture or decoction of boron uterus;
- a mixture of juice from the roots of a golden mustache and burdock;
- a mixture of carrot and beet juice combined with linseed oil;
- alcohol tincture of nettle;
- decoction of cucumber wattle;
- plantain infusion;
- peony extract.
One of the methods of traditional medicine recommended for endometrial hyperplasia is hirudotherapy. It improves blood circulation and metabolic processes in the pelvic organs, reduces the severity of side effects of synthetic hormone therapy, and helps to normalize hormonal levels. However, there are a number of contraindications to hirudotherapy:
- atypical form of endometrial hyperplasia;
- the presence of benign or malignant tumors;
- low blood pressure;
- blood diseases, accompanied by a clotting disorder;
- different types of anemia;
- a tendency to allergies.
Potential consequences and complications
Possible complications and consequences of endometrial hyperplasia are:
- infertility - due to changes in the inner lining of the uterus, the ovum cannot be implanted;
- transformation into a malignant tumor - observed in 1-15% of cases; more often occurs in women with atypical adenomatous hyperplasia and / or in the postmenopausal period.
Forecast
The prognosis depends on the stage and form of the disease, the patient's age, and the timeliness of the initiation of therapy. In young women with an uncomplicated history, the prognosis is generally favorable. After the end of the course of treatment of endometrial hyperplasia, their menstrual, sexual and reproductive function is restored.
The prognosis worsens with age, as well as in the presence of metabolic diseases (diabetes mellitus, metabolic syndrome, obesity), arterial hypertension, cardiovascular pathology. In this case, endometrial hyperplasia, as a rule, is accompanied by frequent relapses and has an increased risk of malignant degeneration, to reduce which removal of the uterus is indicated.
The most serious prognosis is when diagnosing endometrial hyperplasia in elderly women, with atypical and complex forms of hyperplasia. The risk of malignancy in this case is the highest, and the presence of concomitant pathology is often an obstacle to surgical treatment.
Prevention
Prevention of endometrial hyperplasia is based on the timely detection and active treatment of diseases of the female reproductive system, endocrine pathology. Particular attention should be paid to the absence of ovulation.
All women are advised to regularly, at least once a year, visit a gynecologist in order to conduct a preventive examination. If painful sensations occur during intercourse, menstrual irregularities, smearing discharge in the middle of the cycle, you must immediately visit the gynecologist and undergo the necessary examination to identify the cause of these symptoms (they are nonspecific for endometrial hyperplasia, and are characteristic of most uterine pathologies).
Other measures to prevent endometrial hyperplasia include:
- hormonal contraception;
- planning pregnancy to prevent induced abortion;
- regular sex life with a regular partner;
- maintaining a normal body weight;
- balanced diet;
- regular, but not exhausting physical activity;
- rejection of bad habits (smoking, alcohol abuse).
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!