- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Glandular fibrous polyp of the endometrium: causes of formation, symptoms, treatment
The content of the article:
-
Kinds
Features of glandular fibrous polyps
- Reasons for education
- Symptoms
- Diagnostics
-
Treatment
- First stage
- Second phase
- Stage three
- Stage four
- Prevention
- Video
The glandular fibrous polyp of the endometrium is one of the types of pathology that is quite rare. The most common localization is the fundus and uterine corners.

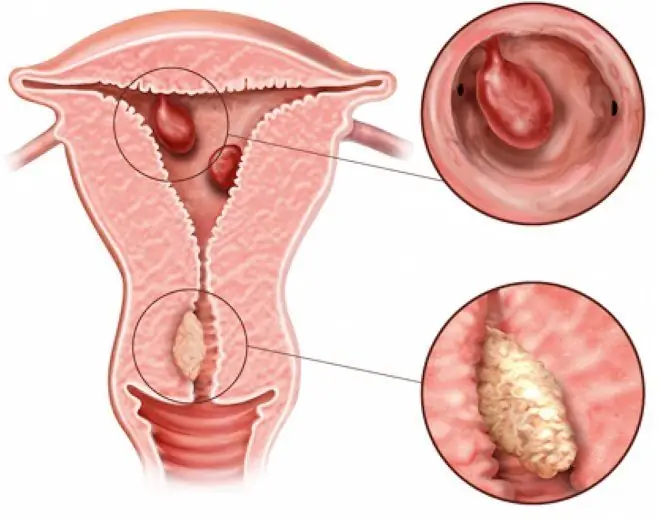
Endometrial polyp - a pathological neoplasm that occurs due to the proliferation of its cells
Endometrial polyp is called a pathological specific neoplasm, the cause of which is the proliferation of endometrial cells (the inner layer of the uterus together with the underlying stroma) as a result of changes in the endometrial receptor apparatus, in which the number of estrogen receptors increases, or due to vascular pathology.
The polyp looks like an oval or round formation, often located on a thin leg, less often on a wide base. Sizes can vary from a few millimeters to 1-6 centimeters, sometimes more.
The glandular fibrous polyp of the endometrium consists of glandular and connective tissue epithelial cells. Its danger lies in frequent inflammation, impaired blood supply, the development of infertility, etc., which leads to intense pain syndrome, sometimes to life-threatening conditions.
Kinds
Endometrial polyps can be single or multiple.

Glandular fibrous polyps are composed of glandular cells and connective tissue cells
According to histological characteristics, they are divided into the following types:
- Fibrous: fibrosis is an overgrowth of connective tissue, which means that the growths are composed primarily of cells of fibrous, or fibrous tissue.
- Glandular fibrous: in their composition, there are glandular cells and connective tissue cells in equal proportions.
- Adenomatous: the rare and most dangerous type of pathology. The growths are formed mainly from glandular tissues; later, under the influence of a number of factors, they can degenerate into malignant tumors. They originate from the basal layer and can acquire a glandular-cystic form. It is rare in its pure form, more often - as tumors with focal adenomatosis.
Depending on the type, these formations can react to cyclic hormonal changes, with them the same functional changes can occur as with the inner mucous membrane of the uterine body.
Features of glandular fibrous polyps
Usually this type is characterized by a benign course. The most common localization is the fundus of the uterus.

The glandular fibrous polyp of the endometrium is most often localized at the fundus of the uterus
The polyp consists of two parts: the body and the legs. Attaching the leg to the bottom of the body of the uterus, it grows into its cavity. Reaching a large size, sometimes partially or completely blocks the cervical canal.
This feature leads to the inability to become pregnant, and if fertilization still succeeds, a miscarriage often occurs in the early stages.
Reasons for education
There are two clinical variants of endometrial hyperplastic processes:
| Process type | Frequency of occurrence | Description |
| Estrogen dependent | 60-70% of cases | This species is characterized by pronounced metabolic dysfunctions, increased production of estrogens or an increased number of receptors for them in the inner lining of the uterus. |
| Non-hormonal (autonomous) | 30-50% of cases | In this case, no disturbances from the endocrine system are observed, and the growth is formed against the background of atrophic phenomena of the mucous layer of the uterus (more typical for the postmenopausal period) |
It is believed that the following factors can provoke the appearance of excessive growth of cells of the uterine mucosa:
- hyperestrogenism: a condition in which estrogen production increases along with a decrease in progesterone biosynthesis (dyshormonal states);
- an increase in the number of estrogen receptors in the uterine lining;
- adrenal dysfunction: some of the sex hormones are synthesized and produced by one of the layers of the adrenal cortex. Therefore, dysfunction of the adrenal glands can also lead to hormonal imbalance;
- inflammatory diseases of the uterus and appendages.
Miscarriages, a history of abortion, smoking, alcoholism, psychoemotional stress can increase the risk of endometrial pathologies.
Symptoms
Usually the disease remains asymptomatic for a long time.
As the progression progresses, the following complaints may occur:
- intermenstrual bleeding (bleeding from the genital tract, which occurs not on the days of menstruation, but for example, in the middle of the menstrual cycle or on other days);
- dyspareunia (painful sensations during intercourse);
- bloody discharge that occurs after intercourse;
- profuse menstrual flow (menorrhagia), which the patient has not previously noted. Menorrhagia can be talked about when a woman often changes hygiene products due to their complete saturation with menstrual blood. This can lead to anemia;
- spotting after exertion or as a result of stress during menopause;
- profuse mucous white discharge.
Another common symptom is infertility.
If the polyp is located near the isthmic part of the fallopian tube (in the wall of the corner of the uterus), it can block the lumen, which leads to the inability of sperm to move into the uterus, which, accordingly, prevents the fertilization of the egg. Also, a growing mass can interfere with the attachment of a fertilized egg to the wall of the uterus.
Diagnostics
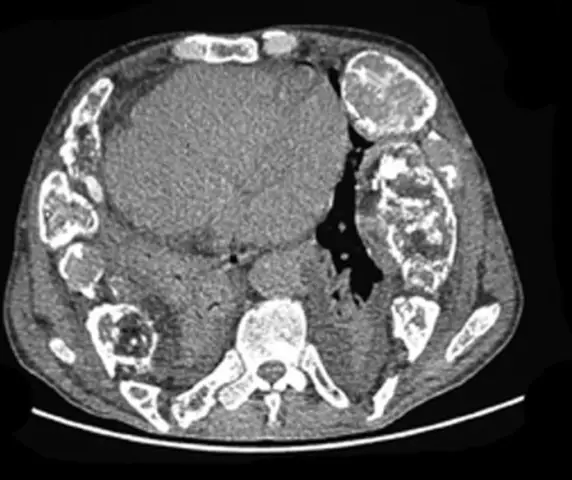
Since a polyp can exist for a long time without manifesting itself in any way (asymptomatic), it is recommended to conduct screening studies aimed at early detection and timely treatment of endometrial hyperplastic processes.

To confirm the diagnosis, the necessary examinations are carried out
The characteristic symptoms and anamnesis help to suspect a growing polyp.
Various methods are used to confirm the diagnosis:
| Method | Description |
| Ultrasound examination (ultrasound) of the pelvic organs | Allows you to visualize a neoplasm or reveal a discrepancy between the thickness of the endometrium and the menstrual cycle or a discrepancy with the menopausal, pre- and postmenopausal periods |
| Endoscopic research method (hysteroscopy) | The method consists in the introduction into the uterine cavity of a hysteroscope - a special optical instrument with which you can visualize the endometrium with its hypertrophied areas |
| Cytological and histological diagnostics | Allows you to investigate the cellular composition of a fragment of the taken tissue, to determine the type of neoplasm, its good quality |
Tissue sampling for cytological and histological examination can be performed during hysteroscopy with targeted biopsy of the hypertrophied area. Also, the fence is possible during the operation of fractional diagnostic curettage of the walls of the uterine cavity and cervical canal.
Scraping is usually carried out on the eve of the expected period or in the early days of its onset.
Often, the appearance of hyperplasia of the uterine mucosa and, as a result, polyps, occurs against the background of hormone-active ovarian tumors, especially in postmenopausal women. This means that in addition to such women, it is necessary to examine in detail the ovaries and hormones.
Treatment
The therapy is carried out in several stages aimed at achieving the following goals:
- Stop bleeding (if any).
- Restoration of reproductive function in women of reproductive age. Normalization of the endometrial structure in patients of reproductive age, during menopause and postmenopause.
- Anti-relapse therapy.
First stage
It consists in the complete removal of the endometrium together with the polyp by fractional diagnostic curettage. The removed material is subjected to careful morphological diagnostics in order to determine the further tactics of patient management.
Second phase
This period consists in treatment after removal of the glandular fibrous polyp of the endometrium. Hormone therapy is shown, which is aimed at suppressing proliferation (reducing proliferation) of the inner lining of the uterus.
For this purpose, gestagens (progesterone) and gonadotropin-releasing hormone agonists are used. The duration of this stage should be at least 6 months.
Stage three
The menstrual cycle is normalized with the appointment of minimum doses of combined oral contraceptives (COCs, contraceptives).
COCs are not prescribed during perimenopause.
Stage four
Dispensary observation for five years after effective hormone therapy is shown.
Prevention
Screening gynecological examinations are an important part of the early detection and timely treatment of various pathological processes. To screen for hypertrophic changes in the uterus, a non-invasive research method is used - ultrasound of the pelvic organs using a transvaginal sensor.

In order to identify and timely treat pathology, it is important to regularly conduct ultrasound of the pelvic organs
Also, an important screening study is the regular (once a year) delivery of smears for cytological and bacterioscopic studies. The collection of smears should be carried out by an obstetrician-gynecologist.
Endometrial polyps pose a danger not only by the possibility of malignancy (which is extremely rare), but also by anemic syndrome, infertility and even septic conditions. Screening, timely and complete treatment minimize the risks of these complications.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.