Cervical osteochondrosis
The content of the article:
- Causes and risk factors
- Stages
- Symptoms of cervical osteochondrosis
- Diagnostics
- Treatment of cervical osteochondrosis
- Possible complications and consequences
- Forecast
- Prevention
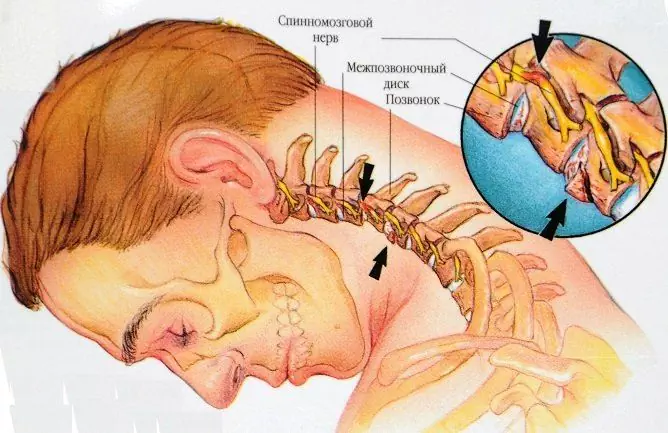
Cervical osteochondrosis is a degenerative-dystrophic process in the intervertebral discs of the cervical spine, accompanied by the replacement of cartilage with bone tissue and immobilization of the vertebrae. According to statistics, one or another degenerative-dystrophic changes in the cervical spine are present in about half of people of working age - from 25 to 45 years.

Source: bubnovsky-ua.com
Causes and risk factors
The anatomical features of the cervical spine create the prerequisites for the early development of degenerative-dystrophic changes. The vertebrae of the cervical segment are characterized by maximum mobility, perform all types of movements in full and are therefore subject to early wear.
A sedentary lifestyle contributes to the development of cervical osteochondrosis, in particular the habit of sitting with the neck stretched forward, which increases the pressure on the intervertebral discs, leading to deformation and dehydration of the pulp nuclei. Degeneration of cartilage tissue is aggravated by trophic disorders due to compression of blood vessels by spasmodic muscles. The following factors contribute to the progressive course of cervical osteochondrosis:
- congenital anomalies of the structure of the vertebrae;
- endocrine disorders;
- autoimmune collagen diseases (rheumatism and systemic lupus erythematosus);
- torticollis of newborns;
- dysplasia of the head of the hip joint;
- flat feet;
- posture disorders and curvature of the spine;
- trauma and microtrauma of the cervical vertebrae;
- smoking and alcohol abuse;
- prolonged emotional distress;
- hereditary predisposition.
The development of cervical osteochondrosis is also facilitated by prolonged intoxication of the body when living in an ecologically unfavorable area, regular contact with harmful substances and the presence of chronic foci of infection in the body.
Stages
Progressive cervical osteochondrosis goes through four stages of development.
- Moderate dehydration of the central part of the intervertebral disc - the nucleus pulposus. The gradual loss of the shock-absorbing and supporting function of the intervertebral discs is compensated by reflex tension of the neck muscles. The patient may be disturbed by aching pains and a feeling of stiffness in the neck, arising from sudden movements and hypothermia.
- Exhaustion of the compensatory capabilities of the muscles. It is manifested by myositis, spasms and congestion. Spasmodic muscles squeeze capillaries and blood vessels, preventing the normal blood supply to the intervertebral disc. As dystrophic changes develop, the framework of the intervertebral disc, or the annulus fibrosus, becomes thinner; a dehydrated nucleus pulposus flattens out and forms a protrusion - a slight protrusion forward or backward within the annulus fibrosus. Under the influence of excessive loads on the articular processes and bodies of the cervical vertebrae, bone growths are formed - osteophytes, which partially compensate for the pressure on the vertebra. Painful sensations in the neck area become habitual and acquire a clear localization; there is instability of the cervical vertebrae, cases of subluxation and dislocation become more frequent with sharp turns and tilts of the head.
- Flattening and thinning of the intervertebral discs results in extrusions. The edge of the deformed nucleus pulposus breaks the annulus fibrosus in the weakest area and extends beyond the edges of the vertebral body. As a result of compression of muscles, nerve and vascular formations by extrusions and osteophytes, compression complications arise.
- The intervertebral discs, ligaments and cartilage of the intervertebral joints are completely calcified; osteophytes of adjacent vertebrae form ankylosis - they are connected to each other, immobilizing the affected segment; the pain in the neck stops.

Source: f.doctor.kz
Symptoms of cervical osteochondrosis
In the early stages of the degenerative-dystrophic process, the disease is almost asymptomatic. Unpleasant sensations in the neck arise only with sudden movements, after prolonged maintenance of a tense sitting posture and head tilt, or in response to excessive physical exertion. The development of myositis is accompanied by a feeling of stiffness, and a clear localization of pain indicates spasms in the muscles of the neck.
Decompensated cervical osteochondrosis is characterized by persistent discomfort in the neck, habitual muscle tension and limited mobility of the cervical segment; the forced position of the head partly smooths out the unpleasant sensations. When turning and tilting the head, the crunch of the vertebrae is often heard. Subluxations of the intervertebral joints are accompanied by acute burning pain, which is popularly called lumbago, and autonomic disorders: aching headache, dizziness, darkening of the eyes, palpitations, etc. Spontaneous reduction of the subluxation brings quick relief.
In the case of the formation of osteophytes and extrusions on the posterior surface of the vertebrae, radicular symptoms are later added to the general manifestations of cervical osteochondrosis:
- headaches localized in the back of the head and parietal region;
- decreased sensitivity of the skin on one side of the neck;
- speech disorders and numbness of the tongue;
- discomfort in the outer surface of the shoulder;
- respiratory disorders.
With the defeat of osteochondrosis of the third cervical vertebra, reflex cardialgic syndrome is sometimes observed - severe pains behind the sternum radiating to the scapula and shoulder, causing associations with a heart attack, especially if the painful sensations are accompanied by a rapid heartbeat. In the case of damage to the three lower vertebrae, painful sensations and paresthesias spread from the neck to the scapula, forearm, hand and fingers. Patients may complain of numbness in the upper extremities, a burning sensation, tingling sensation, or "creeping" along the nerves.
Osteophytes located on the lateral surfaces of the vertebrae squeeze the vertebral artery, causing a complex of cerebrovascular accidents called vertebral artery syndrome. This pathology is manifested by frequent attacks of pressing headache, which spreads from the back of the head to the crown and temples, giving it to the eyeballs. In some cases, instead of a headache, there is a constant feeling of heaviness in the head. At the same time, vegetative symptoms are observed:
- drops in blood pressure;
- heart attacks and arrhythmias;
- migraine-like unilateral throbbing headaches accompanied by photophobia, nausea and vomiting;
- violations of thermoregulation (chills, sweating, cold extremities);
- attacks of dizziness, fainting and drop attacks;
- violations of coordination of movements;
- noise and congestion in the ears;
- decreased visual acuity and visual disturbances: darkening and double vision, blurred vision, flashes and multi-colored flies before the eyes;
- sleep disorders;
- increased fatigue and emotional lability.
Diagnostics
Due to the low specificity of symptoms and a wide variety of manifestations, the diagnosis of cervical osteochondrosis is carried out in several stages. You should start with the consultation of a specialist - a surgeon, orthopedist, neuropathologist or vertebrologist. A presumptive diagnosis is made based on the patient's complaints, medical history and the results of a physical examination. During the examination of the patient, the doctor pays attention to the mobility of the neck, the sensitivity of the skin and painful areas in the cervical segment and shoulder girdle, muscle strength and tone, the severity of tendon reflexes.
To determine the stage of the pathological process and identify complications, the patient is sent for an MRI of the cervical spine. Thanks to high-quality visualization of hard and soft tissues on tomograms, all signs of cervical osteochondrosis are clearly visible - a decrease in the height of intervertebral discs, osteophytes, protrusion, extrusion, damage to nerves and blood vessels, calcification of ligaments, foci of bone tissue resorption, myositis and congestion in muscles.
If MRI is unavailable, radiography or CT of the cervical segment is performed to detect osteophytes, osteoarthritis and a decrease in bone density. Changes in soft tissues are visualized using ultrasound; to study hemodynamics and assess the degree of damage to blood vessels with advanced cervical osteochondrosis, dopplerography of the neck vessels is prescribed, and if there is suspicion of spinal cord infringement, contrast myelography.
Cardiac syndrome with osteochondrosis of the cervical spine is differentiated from angina pectoris and coronary heart disease. In doubtful cases, it may be necessary to consult a cardiologist and functional examinations of the heart - ECG and echocardiography of the heart, stress tests.

Source: dota2on.ru
Treatment of cervical osteochondrosis
Osteochondrosis of the cervical spine requires complex treatment. During exacerbations, the main task of therapy is to relieve pain, stop the inflammatory process and restore capillary blood circulation in the affected areas. Patients are prescribed analgesics or non-steroidal anti-inflammatory drugs, of which cyclooxygenase-1 inhibitors based on diclofenac and nimesulide are preferred. A new group of NSAIDs - selective COX-2 inhibitors - have a lesser effect on the gastrointestinal tract than previous generations, and its anti-inflammatory and analgesic effect is equal to or even higher than that of older generations. It is for this reason that Amelotex is chosen for long-term therapy. A wide range of various forms of release allows for step therapy - quickly relieve pain with injections,continuing treatment in a human-friendly tablet form. Amelotex has a high anti-inflammatory and analgesic efficacy, a low incidence of gastrointestinal and cardiovascular adverse events. With severe muscle spasms, it is recommended to wear an orthopedic collar; if necessary, prescribe antispasmodics and muscle relaxants.
In radicular syndromes with a weak response to drug treatment, they resort to X-ray-controlled blockades of the restrained roots and steroid injections. To improve metabolism in the intervertebral discs and damaged nerve structures, a course intake of vitamins of group B is shown. Complicated extrusions, spinal cord infringement and intractable pain syndrome are indications for surgical intervention.
As the acute symptoms subside, a course of physiotherapy begins, aimed at activating the blood supply in the damaged areas and utilizing the products of inflammation. Electrophoresis and phonophoresis, magnetotherapy, amplipulse therapy, shock wave therapy, UHF and diadynamic therapy have proven themselves well.
The rapid restoration of mobility of the cervical spine is facilitated by classes in exercise therapy groups, swimming and aqua gymnastics. You can also do it at home: the most effective exercises for cervical osteochondrosis do not require special equipment and simulators. The daily rehabilitation program is designed for 15-20 minutes and includes five simple exercises. Each exercise is repeated 5 times at a slow, smooth pace, gradually increasing the number of repetitions up to 10-12 times.
- Turns and rotations of the head to the right and left with a constant position of the head and shoulders.
- Alternate pressure with the forehead and the back of the head on the palm with slight tension in the neck muscles.
- Tilt of the head thrown back to the jugular fossa and to the side. When bending to the right, touch the right ear to the right shoulder, and the left ear to the left shoulder.
- Pressing with the left temple on the palm of the left hand, then with the right temple on the right palm.
- Tilting the chin to the neck with the head turning first to the right, then to the left.

Source: lechimsustavy.ru
The means of traditional and alternative medicine should be treated with great caution and their use should be coordinated with the attending physician. In the absence of contraindications, you can take a course of reflexology, osteopathy and hirudotherapy; manual therapy is strictly contraindicated. Ordinary therapeutic massage for cervical osteochondrosis gives more encouraging results without exposing the patient to unnecessary risk.
Possible complications and consequences
The neck area contains a large number of autonomic nerve plexuses and blood vessels, including the vertebral artery and vertebral nerve. The joints that connect the protruding anterior edges of the vertebrae are prone to dislocation and subluxation, and the triangular shape of the intervertebral foramen in the lower three cervical vertebrae increases the likelihood of nerve root entrapment by bony growths and spasmodic muscles. As a result, the risk of joining compression syndromes in cervical osteochondrosis is higher than in other parts of the spine.
In the early stages of the disease, complications are mainly associated with myositis and muscle spasms. The anterior scalene muscle syndrome develops with prolonged compression of the brachial plexus and the subclavian artery by the spasmodic scalene anterior muscle. Reflex irritation of autonomic nerve fibers and insufficient blood supply to muscle tissue is manifested by soreness of the forearm and hand, which increases with a tilted head position and abduction of the arm. When large vessels are squeezed, a cold snap and swelling of the limb are noted.
The defeat of the muscles and tendons of the shoulder girdle provokes degenerative-dystrophic changes in the shoulder joint, causing humeroscapular periarthrosis and unilateral atrophy of the muscles of the shoulder and scapula. Pain with progressive humeroscapular periarthrosis radiates from the neck to the scapula and intensifies when lying on the sore side.
The appearance of extrusions and osteophytes is accompanied by radicular syndromes, which, in turn, can be complicated by an infringement of the spinal cord. Spinal cord compression often causes paralysis of the upper limbs and, in the most severe cases, is fatal due to a sharp depression of respiratory function. Severe vertebral artery syndrome, occurring against the background of severe ataxia and decompensated neurocirculatory dysfunction, threatens to turn into disability and increases the risk of ischemic stroke and spinal cord ischemia.
Forecast
Full restoration of intervertebral discs in osteochondrosis is unlikely, but with the help of timely and adequate therapeutic measures, it is possible to stop or slow down the progression of the degenerative-dystrophic process, prevent complications and achieve maximum preservation of the cervical spine mobility. With advanced osteochondrosis of the cervical spine, complicated by multiple extrusions and compression syndromes, the prognosis is more cautious.
Prevention
One should think about the prevention of cervical osteochondrosis even in childhood. Formation of correct posture, consistent strengthening of the muscular corset of the back and good nutrition will help maintain the health of the spine in adulthood. If a child detects postural disorders, flat feet and the consequences of birth injuries, such as torticollis or dysplasia of the head of the hip joint, rehabilitation programs should not be neglected: many pathologies of the musculoskeletal system accompanying osteochondrosis are successfully cured before the skeleton is ossified.
If the patient's profession involves a sedentary lifestyle, you need to find an ergonomic office chair with neck support, and include an orthopedic mattress and a low firm pillow in the bedding set. It is not recommended to sleep on soft sofas and beds with shell mesh; it is better to choose a model with a moderately hard, flat surface. During work, every 45-60 minutes, it is advisable to do exercises for the neck, and at leisure to exercise and walk more often on foot. Swimming and water aerobics, yoga, qigong and Pilates give a good effect; power and traumatic sports are best excluded. During exercise, you should avoid sudden movements and keep your back straight. When doing household chores, you cannot stand on tiptoe for a long time or keep your hands raised above your head;it is better to use a stepladder or stand on a stool. Two or three times a year it will not hurt to undergo a course of therapeutic and prophylactic massage of the cervical-collar zone.
The diet should contain a sufficient amount of protein, vitamins and minerals; if possible, jelly, jellied fish and seafood should be included in the menu - sources of natural collagen. Avoiding bad habits helps maintain active blood circulation in the intervertebral discs.
YouTube video related to the article:

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!