Numbness of the leg from hip to knee on the outside
The content of the article:
-
The reasons for the development of paresthesia
- Transient sensitivity disorders
- Prolonged sensitivity disorders
-
Neuropathy of the external cutaneous nerve of the thigh
- Development mechanism
- Provoking factors
- Roth syndrome and pregnancy
- Diseases causing numbness of the thigh
- Diagnostics
- Treatment
- Video
Numbness of the leg from the hip to the knee on the outside is a sensory disorder called paresthesia. Localization of paresthesia in the thigh area occurs quite often and is a consequence of various pathological processes in the human body that affect the nervous structures: tumors, infectious, neurodegenerative, autoimmune lesions. Since loss of sensitivity is not an independent disease, the elimination of this symptom depends on the effectiveness of the treatment of the underlying pathology.

Most often, numbness of the leg from the hip to the knee from the outside is not associated with pathologies and is transient
The reasons for the development of paresthesia
Paresthesias in the lower extremities are accompanied not only by numbness, but also by tingling, burning, pain of varying intensity. These sensations are short-lived, and can bother the patient for a long time or occur in the form of seizures. Accordingly, the first were called passing, and the second - chronic paresthesias.
Transient sensitivity disorders
If, after excessive physical exertion, a long stay in an uncomfortable position, the outer surface of the right leg is not felt, or the thigh of the left leg grows numb from the outside, the reasons for the loss of sensations are obvious. In this case, temporary numbness is provoked by:
- violation of local blood circulation;
- mechanical compression of the superficial nerve;
- irritation of nerve endings with acidic products of cellular metabolism.
Such violation of sensitivity does not require special therapeutic measures and goes away on its own. For this, it is enough to rest, change the position of the body, and light massage.
Prolonged sensitivity disorders
When the outer side of the thigh is not felt for a long time, then pathological changes are more serious than with passing paresthesia. They can be the result of a primary lesion of the nervous system or be a consequence of a long-term illness. Chronic paresthesia of the anterior, lateral parts of the lower limb from the hip to the knee leads to:
- neuropathy of the external cutaneous nerve of the thigh;
- osteochondrosis of the lumbar spine;
- intervertebral hernia of the lumbosacral region;
- arthritis of the hip joint;
- deforming arthrosis of the hip joint;
- multiple sclerosis;
- diabetic neuropathy;
- atherosclerosis of the vessels of the lower extremities;
- alcoholic polyneuropathy;
- injury to the hip joint;
- tumor process.
The various mechanisms of action of these negative factors are ultimately reduced to a change in metabolic processes in the nervous tissue and to a violation of the conduction of nerve impulses.
Neuropathy of the external cutaneous nerve of the thigh
Neuropathy of the external cutaneous nerve of the thigh refers to the tunnel syndromes of peripheral nerve damage. In the medical literature, you can find several synonyms for the name of this ailment: paresthetic meralgia, lateral cutaneous nerve syndrome of the thigh, Roth syndrome, Roth-Bernhardt disease.
Development mechanism
The nerve and its branches reaching the knee joint innervate the outer and partly the anterior femoral surfaces. The most vulnerable part of the nerve is the place of its exit from the pelvic cavity: above the anterior superior iliac spine or below the inguinal ligament. It is there or in the tunnel formed by the connective tissue membrane of the thigh muscles, and its compression occurs, which causes the development of the syndrome.
Neuropathy is manifested by numbness, tingling, pain in the antero-lateral surface of the thigh, with increased stress and intense pain syndrome - a violation of walking. Roth - Bernhardt disease occurs mainly in middle-aged and elderly people, and the incidence of men is three times higher than that of women.
Why does paresthetic meralgia develop more often after 50 years? This is due to age-related degenerative changes in the nervous tissue due to:
- obstructed venous outflow;
- inferiority of the capillary network;
- metabolic disorders.
Provoking factors
Complaints begin to appear when the compression effect of the provoking factor becomes critical. Compression in the groin or at the level of the iliac muscle can result from:
- wearing a corset, tight belt, overly tight underwear;
- excessive deposition of fat in the lower part of the anterior abdominal wall and thighs (lyes);
- retroperitoneal hemorrhage;
- tumor process;
- inflammatory infiltration of the abdominal cavity;
- surgical intervention on the abdominal organs.
Roth syndrome and pregnancy
Compression of nerve fibers at the level of the inguinal ligament is a common cause of neuropathy during gestation. During pregnancy, the bending of the spine in the lumbar spine, the angle of inclination of the pelvis and extension in the hip joint increase. All this leads to tension on the ligament and compression of the nerve.
Roth syndrome is one of the common, but not the only, causes of numbness in the leg from the hip joint to the knee.
Diseases causing numbness of the thigh
Loss of sensitivity of the lower extremities is possible with impaired nerve conduction accompanying various diseases.
| Disease | Manifestations | Pathological changes |
| Osteochondrosis of the lumbosacral spine | Pain and paresthesias spread from the lower back to the buttock along the outer edge of the thigh, the lateral surface of the lower leg to the back of the foot and the big toe. | Degenerative-dystrophic lesion of the intervertebral discs located between the vertebral bodies: wear under the influence of stress, high and long-term traumatic effects. |
| Intervertebral hernia in the lumbosacral spine | Numbness, tingling, weakness in the lower limb. Pain of varying intensity, radiating to the buttock, along the posterior outer surface of the thigh and lower leg on the affected side. Possible dysfunction of the pelvic organs. | Protrusion of the intervertebral disc between the vertebral bodies associated with displacement of the nucleus pulposus of the disc and rupture of the annulus fibrosus. Leads to compression of the nerve roots and blood vessels. |
| Arthritis of the hip joint | Pain, sensory disturbances in the groin, lateral thigh, buttock, limitation of range of motion, difficulty walking. | Inflammatory process of various etiologies (rheumatoid, reactive, infectious, psoriatic), affecting the connective tissue in the area of the joint of the pelvic and femur bones. |
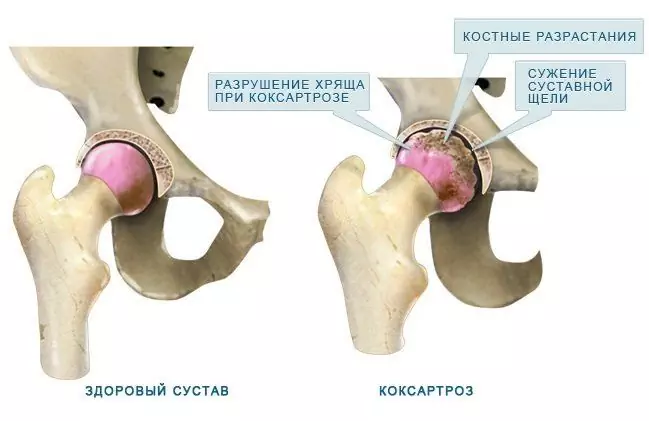
| Coxarthrosis (deforming arthrosis, osteoarthritis of the hip joint) | Joint pain, from the groin to the knee, stiffness of movement, paresthesia, gait disturbance, lameness, atrophy of the thigh muscles, shortening of the limb on the affected side. | Degenerative-dystrophic changes in the hyaline cartilage of the articular surfaces. |
| Multiple sclerosis | Paresthesias, violation of deep and superficial sensitivity: a decrease in vibrational, tactile sensations, a feeling of pressure in one or more limbs. | Damage to the myelin sheath of nerve fibers in the brain and spinal cord: the formation of foci of sclerosis (plaques) with the replacement of normal nerve tissue with connective tissue. |
| Peripheral diabetic neuropathy | Numbness, burning sensation, tingling, decrease or loss of temperature, pain sensitivity, first in the feet, then in the proximal extremities. | Metabolic disorders, damage to small blood vessels. The pathological process affects all nerve fibers: sensory, motor and vegetative. |
| Obliterating atherosclerosis of the vessels of the lower extremities | Chilliness, numbness of the limbs, intermittent claudication; trophic disorders: skin discoloration, atrophy of subcutaneous tissue, ulcers, dry gangrene. | Violation of lipid and protein metabolism in the arteries of the elastic and muscular-elastic type, accompanied by the deposition of cholesterol and some lipoprotein fractions in the lumen of the vessels, leading to circulatory failure. |
| Alcoholic polyneuropathy | Sensory disturbances, manifested by a feeling of numbness, crawling creeps; edema of the distal extremities, changes in color and temperature; soreness in the calf muscles, weakness, paralysis. | The toxic effect of alcohol and its metabolites on metabolic processes in nerve fibers: axonopathy (damage to the long processes of nerve cells) with secondary damage to the myelin sheath. |
Diagnostics
Diagnosis of the disease that led to the development of numbness of the leg from the hip to the knee on the outside is usually carried out by a neurologist. Medical history and neurological examination data may be supplemented by:
- X-ray of the spine, hip joint;
- magnetic resonance imaging of the spine, hip joint, brain;
- ultrasound examination of the abdominal organs, small pelvis, hip joint;
- ultrasound dopplerography of the vessels of the lower extremities;
- laboratory examination (detailed clinical, biochemical blood tests).

If an accurate diagnosis is necessary, MRI of the affected limb is performed
You may need to consult specialists: vascular surgeon, neurosurgeon, orthopedist, therapist, endocrinologist, rheumatologist, etc.
Treatment
A prerequisite for achieving a positive effect of therapy for chronic paresthesia is the elimination of the immediate cause that led to its development. It is necessary to treat in a complex way, using medication, physiotherapy and reflexology methods. The result is achieved by:
- balanced diet;
- normalization of body weight;
- to give up smoking;
- elimination of alcohol;
- therapeutic exercise, especially swimming and walking.
The sooner the patient seeks qualified medical care, the more successful and cheaper the treatment will be.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.