- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Deforming arthrosis
The content of the article:
- Causes and risk factors
- Forms of the disease
- Stages
- Symptoms
- Diagnostics
- Treatment of deforming arthrosis
- Possible complications and consequences
- Forecast
- Prevention
Deforming arthrosis is a chronic slowly progressive degenerative disease, which is characterized by damage to the articular cartilage and bone surfaces with subsequent involvement of the periarticular soft tissues in the pathological process.
The disease is widespread. It affects about 20% of adults. The first symptoms usually begin between the ages of 40 and 60. Women get sick twice as often as men.

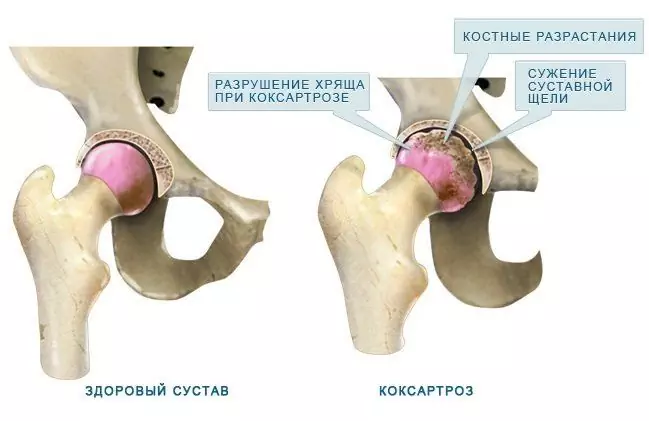
With deforming arthrosis, articular cartilage and bone surfaces are affected
The development of deforming arthrosis is based on the natural aging process of the articular cartilage. X-ray examination reveals signs of damage to the articular apparatus in every second person over 55 years old.
Most often, the pathological process affects the knee joints (75%) and small joints of the hand (60%). Other joints are less commonly affected: the lumbar and cervical spine (30%), the hip (25%), the ankle joint (20%), and the shoulder joint (15%). Deforming arthrosis of the hip joint is called coxarthrosis, and the knee joint is called gonarthrosis.
Causes and risk factors
The internal structures of the joint are covered with hyaline cartilage to allow movement and reduce friction. When the regenerative processes are disturbed, the articular cartilage begins to wear out and become thinner. Its surface becomes rough, cracks and abrasions appear on it. Over time, in some areas, there is an almost complete loss of cartilage. In order to compensate for friction, the exposed areas of the surface of the bones involved in the formation of the joint begin to thicken. In them, characteristic osteosclerotic changes occur, leading to the growth of bone tissue (osteophytes) and the formation of bone pseudocysts. In turn, bone growths create even more obstacles in friction of the articular surfaces, intensifying degenerative processes.
Factors that increase the risk of developing deforming arthrosis are:
- elderly age;
- female;
- congenital joint pathology (violation of the mutual arrangement and shape of the articular surfaces, hypermobility);
- structural defects associated with diseases of the musculoskeletal system that begin in childhood (hip dysplasia, Perthes disease);
- injuries and mechanical damage to joints (recurrent dislocations, meniscectomy, intra-articular fractures);
- obesity;
- occupational hazards (for example, deforming arthrosis of the finger joints of typists);
- microcrystalline arthropathy (gout, pyrophosphate arthropathy);
- metabolic (alkaptonuria) and endocrine (acromegaly) diseases;
- avascular necrosis;
- diseases accompanied by the destruction of articular cartilage (hemarthrosis, septic arthritis).

Deforming arthrosis of the hand is a fairly common disease in typists
Forms of the disease
Deforming arthrosis is primary and secondary. The primary form of the disease develops in an initially healthy joint and is usually caused by natural aging processes. Secondary deforming arthrosis affects joints that already have any defects in hyaline cartilage caused by metabolic and hormonal disorders, aseptic bone necrosis, inflammation of the bone-articular tissues, or trauma.
Stages
In the development of deforming arthrosis, in accordance with the characteristics of the clinical and radiological picture, several stages are distinguished:
- A slight limitation of mobility in the affected joint is characteristic. On the roentgenogram, the presence of initial osteophytes located along the edge of the articular surfaces and an indistinct narrowing of the joint space are determined.
- The mobility of the affected joint is reduced. When moving, a characteristic crunch is often heard. The muscles are moderately atrophied. The radiograph clearly shows subchondral osteosclerosis, narrowing of the joint space and the presence of many osteophytes.
- Visible deformity of the joint. The range of motion is sharply limited. The radiograph reveals the presence of "articular mice" (a fragment of bone tissue, freely located in the joint cavity), subchondral cysts, extensive osteophytes, almost complete absence of the joint space.

Stages of deforming arthrosis
Some authors also distinguish an additional 0 stage of the disease, in which degenerative changes in the joint have already begun at the cellular level, but radiological and clinical symptoms are still absent.
Symptoms
The main symptoms of deforming arthrosis are:
- pain (increases during physical exertion and subsides at rest);
- morning stiffness (difficulty in mobility in the joint after a night's sleep lasting 25-30 minutes);
- the phenomenon of the gel (swelling of the articular region after prolonged immobilization of the limb);
- crepitus (heard when performing passive movements in the joint in full and is due to the incongruence of the articular surfaces);
- limitation of mobility in the joint (due to pain and / or blockage by "articular mouse");
- subluxation of the joint, valgus or varus deformity (occur in the later stages of the disease);
- swelling and effusion into the articular cavity (most often observed with deforming arthrosis of the knee joint);
- zones of myofibrosis (the appearance of small painful nodules in the regional muscles).

With deforming arthrosis, pain and swelling of the articular region is observed
Deforming arthrosis of the hip joints is very difficult. Patients complain of pain in the groin area, which can radiate to the knee. Often there is a "jamming" of the affected joint. Over time, hypotrophy of the muscles of the buttock and thigh gradually develops, which leads to the formation of flexion-adduction contracture, shortening of the limb and lameness. In severe cases, complete immobility of the limb develops on the side of the lesion.
Deforming arthrosis of the knee joints is manifested by the occurrence of pain when performing flexion and extension movements, climbing stairs, and long walking. A symptom of deforming arthrosis of the small joints of the hands is the appearance of dense small nodules along the edges of the distal and proximal interphalangeal joints (Bouchard's nodules, Heberden's nodules), as well as stiffness and soreness of the affected joints.
The generalized form of deforming arthrosis (polyarthrosis, Kellgren's disease) is manifested by multiple lesions of the intervertebral and peripheral joints. This form of the disease is often combined with another pathology of the articular apparatus (tendovaginitis, periarthritis, spondylosis of the lumbar and cervical spine, osteochondrosis).
Diagnostics
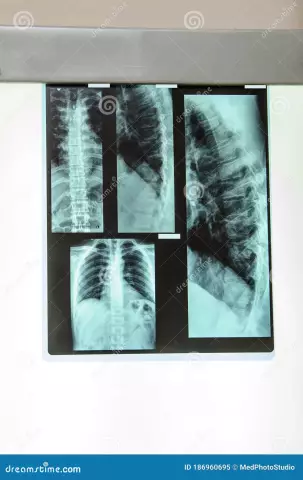
The main method for diagnosing deforming arthrosis is radiography. Revealing on radiographs of joint space narrowing, osteosclerosis, marginal osteophytes, subarticular cysts, spotted calcification of cartilage confirms the diagnosis of deforming arthrosis.
Magnetic resonance imaging and computed tomography, ultrasound scanning of joints are used as additional methods of instrumental diagnostics.
If indicated, puncture of the affected joint is performed, followed by laboratory examination of the resulting synovial fluid (increased viscosity is detected, leukocytes are less than 2,000 in 1 μl, neutrophils are less than 25%).

The main method for diagnosing deforming arthrosis is radiography.
In diagnostically difficult cases, there are indications for performing arthroscopy - an invasive study that allows you to examine the joint from the inside using an endoscopic apparatus equipped with a microcamera. During this procedure, the doctor makes a targeted sampling of a small area of the synovial membrane, cartilaginous tissue, synovial fluid, followed by a morphological study of the obtained biopsies.
Differential diagnosis of deforming arthrosis is carried out with mono- and polar arthritis, rheumatic diseases.
Treatment of deforming arthrosis
Complex therapy of deforming arthrosis is carried out taking into account the stage of the disease, the cause that caused it, the general condition of the patient. First of all, it is recommended to reduce the load on the affected joint (using a cane while walking, avoiding prolonged forced poses, refusing to lift weights).
To relieve pain and reduce the activity of the inflammatory process, patients are prescribed non-steroidal anti-inflammatory drugs. If their intake does not lead to the elimination of pain, intra-articular administration of corticosteroid drugs is performed. Gels and ointments with analgesic and anti-inflammatory effects are applied locally.

In order to prevent further destruction of the joint in deforming arthrosis, chondroprotectors may be prescribed
In the initial stages of deforming arthrosis, in order to stop further destruction of the articular cartilage, some experts recommend chondroitin sulfate and glucosamine hydrochloride, which have a chondroprotective effect. It should be noted that the effectiveness of this group of drugs has not been confirmed in clinical trials.
In the treatment of deforming arthrosis, physiotherapeutic techniques are widely used: laser therapy, magnetotherapy, electrophoresis with novocaine or analgin, high-frequency electrotherapy, ozokeritotherapy, paraffin applications.
To improve the function of the affected joints and strengthen the musculo-ligamentous apparatus, patients are recommended to regularly engage in physiotherapy exercises, kinesiotherapy. Balneotherapy plays an important role in the rehabilitation treatment of deforming arthrosis.
With the complete destruction of the hip or knee joint, the ability to work is lost, disability occurs. Conservative treatment at this stage of the disease is ineffective. In order to restore mobility and improve the quality of life of patients, they are shown endoprosthetics, that is, the replacement of the affected joint with an artificial one.
At the terminal stage of deforming arthrosis, in order to eliminate the pain syndrome, it is shown that arthrodesis is performed, an operation during which the joint is completely immobilized.
Currently, a new method is being developed for the treatment of deforming arthrosis, which consists in the use of stem cells that have the ability to replace the cells of the articular cartilage and activate the course of regenerative processes.
Possible complications and consequences
Long-term deforming arthrosis can be complicated by:
- habitual dislocation;
- spontaneous hemarthrosis;
- reactive secondary synovitis;
- ankylosis.
Forecast
The rate of destruction of the joint in deforming arthrosis is determined by the age of the patient and his initial state of health, localization and form of the pathological process. In most cases, with timely initiated and actively pursued treatment of deforming arthrosis, it is possible to improve the mobility of the affected joint, relieve pain. However, complete restoration of the lost cartilage tissue is impossible.
Deforming arthrosis of the hip joint (coxarthrosis) often leads to a significant decrease in working capacity. In the terminal stage of the disease, patients almost completely lose the ability to move independently, the ability to self-care and need constant care.
Prevention
Prevention of the development of deforming arthrosis includes the following measures:
- maintaining a normal body weight;
- regular gymnastics (however, excessive physical activity, during which the joints are constantly exposed to increased stress, is contraindicated);
- timely detection and treatment of diseases (scoliosis, flat feet, dysplasia) and injuries (bruises, sprains, dislocations) of the musculoskeletal system;
- rational nutrition, balanced in the composition of macro- and micronutrients.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!