Brain hematoma: types, symptoms, treatment, prognosis
The content of the article:
- The structure of the brain
- The reasons
- Types of hematomas
-
Epidural hematoma
-
Symptoms
- Blurred light gap
- Lack of light period
-
-
Subdural hematoma
Symptoms
-
Intracerebral hematoma
Symptoms
- Diagnostics
- Treatment
- Consequences of a brain hematoma
- Video
A hematoma of the brain is most often the result of a head injury, in most cases, a shock and a traffic accident. In old age, any, even minor, traumatic effect can lead to rupture of blood vessels and the formation of a hematoma.

Most often, cerebral hemorrhage occurs due to trauma
The human brain (hereinafter referred to as GM) is represented by neurons (parts of which form the gray and white matter of the brain) and three of its membranes - hard, soft and arachnoid. Each of them performs vital functions.
The structure of the brain
The hard shell is the most superficial, its outer part, facing the inner surface of the bones of the skull, and the inner one - towards the arachnoid membrane. It is rich in nerve endings and forms the cavernous sinuses and vaginas for the nerves leaving the cranial cavity.

The brain is surrounded by three membranes
The median membrane is arachnoid, represented mainly by vessels. It provides adequate blood supply, lymph drainage and CSF dynamics.
The closest to the GM is the soft shell. It also participates in the blood supply to the brain, penetrates into all furrows and crevices and provides a kind of fixation of the integument of the GM.
Between each of the membranes there are spaces partially filled with serous fluid, which, if injured or for other reasons, can fill with blood coming from damaged blood vessels, forming a hematoma.
The reasons
In addition to trauma, other causes of hemorrhage include:
- Deformation, changes in the structure of the vessels of the brain, which occurs due to chronic or other diseases, including autoimmune (aneurysm, arteriovenous malformation, cerebral amyloid angiopathy).
- Uncontrolled arterial hypertension, hypertensive crisis.
- Primary or metastatic tumor processes of GM.
- Long-term uncontrolled intake of anticoagulants (Warfarin, Acetylsalicylic acid, etc.).
- Hematological diseases (hemophilia, oncohematology, sickle cell anemia).
Types of hematomas
Depending on the localization, the following forms of GM hemorrhage are distinguished:
| Kinds | Description |
| Epidural | Formed in the space bounded by the outer surface of the hard shell and the inner surface of the skull |
| Subdural | Spilled blood accumulates between the hard and arachnoid membranes |
| Intracerebral | Formed as a result of hemorrhage in the brain tissue, sometimes with a breakthrough into the ventricles and the formation of ventricular hemorrhage |
| Subarachnoid | Accumulation of blood in the subarachnoid space |
From a damaged vessel, blood can soak the very substance of the brain, in which case they speak of intracerebral hemorrhage.
Types of subdural hematomas according to the clinical course:
| Kinds | Description |
| Sharp | Typical symptoms develop immediately after injury or exposure to a damaging factor |
| Subacute | In this case, the clinical picture is not obvious immediately, but manifests itself within a few hours. |
| Chronic | A person with chronic subdural hematoma can walk for months, and in rare cases - for years, unaware of their disease, due to the absence of characteristic clinical signs |
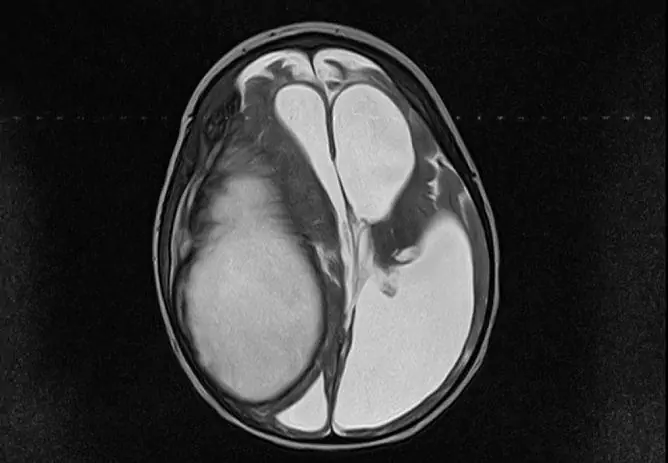
Epidural hematoma
It forms above the dura mater and can reach up to 8 cm in diameter, accumulating an average of 80-120 ml of blood (sometimes up to 250 ml). Due to the detachment of the dura mater from the bones of the skull, it has a characteristic biconvex lens appearance, in which there is a decrease in size from the center to the periphery.

Epidural hematoma forms over the dura mater; in the subdural form, blood accumulates between the dura mater and arachnoid
An interesting fact is that subdural hemorrhages almost never occur in children under two years old and in people over 60 years old due to the tight attachment of the hard shell to the bones of the skull.
Most often, they are formed in men aged 16–25 years, in patients of the opposite sex, they are less common (more than 2 times).
Symptoms
A characteristic clinical picture is the presence of a light period, in which the patient loses consciousness for a short time, and after recovery complains of moderate cephalalgia, dizziness, and weakness. Objectively, amnesia, anisoreflexia, nystagmus, and mild meningeal symptoms can be observed.

Pathology is accompanied by headache and weakness
This condition is regarded as a head injury of mild to moderate severity. However, after the light period (on average - from half an hour to several hours), symptoms sharply increase, headache intensifies, and vomiting is observed.
Consciousness suddenly deteriorates, up to sopor (subcoma) and coma. Objectively, there is a decrease in heart rate, an increase in blood pressure, unilateral mydriasis (on the side of hemorrhage), paresis of the facial nerve and other focal signs indicating compression of the GM.
Blurred light gap
The process can proceed with an erased light gap. In this case, the absence of consciousness, coma is immediately noted. Then, after some time (several hours), consciousness begins to recover to stupor, sometimes verbal interaction with the patient is possible, in which he can indicate a severe headache.
In this state, the patient can be from several minutes to 24 hours, after which the symptomatology, as in the first case, progressively and sharply worsens, the stupor turns into excitement, and then into a coma. Objectively, severe vestibular, neurological and other disorders are observed, indicating damage to the brain stem. Vital functions progressively deteriorate.
Lack of light period
The absence of a light period is a rather rare occurrence in which immediately after an injury the patient is in a coma, without changing his consciousness. This is a poor prognostic sign observed in severe traumatic brain injury in combination with other brain damage.
Subdural hematoma
In this case, blood from damaged vessels accumulates between the hard and arachnoid meninges. In terms of frequency, it is about 40% of all intracranial hematomas.
Symptoms
Signs of impairment of consciousness, psyche, headaches and vomiting come to the fore.
Classically, the symptoms of hemorrhage are three-stage, in which at first there is a lack of consciousness, then a short-term bright interval follows (partial restoration of consciousness), which is replaced by a lack of consciousness, the onset of coma. However, such staging is rarely observed, often the light gap is either erased or completely absent.
Other clinical symptoms:
- amnesia;
- delirious, oneiroid syndrome;
- euphoria, ridiculous behavior, agitation;
- epileptic seizures;
- headache, dizziness, increased sensitivity to light;
- dilation of the pupil from the side of hemorrhage;
- other symptoms indicating brain compression;
- focal symptoms.
Intracerebral hematoma
It is represented by a limited accumulation of liquid or clotted blood (1–100 ml) in the GM substance.

With an intracerebral hematoma, blood accumulates in the substance of the brain
The accumulated liquid in the GM substance is characterized by the following clinical signs:
- Compresses the surrounding neurons, which inevitably leads to their necrosis.
- It leads to an increase in intracranial pressure and the development of GM edema.
- It provokes the formation of a dislocation syndrome (in which a large amount of accumulated blood leads to a displacement of the median structures of the brain).
The forming spasm of the vessels located near the hematoma aggravates the process, increasing the area of necrosis. In 15% of cases, blood breaks through into the ventricles of the GM (ventricular hemorrhage).
Pathology is classified depending on location and size. The size of the hematoma is distinguished:
- small: up to 20 ml, up to 3 cm in diameter;
- medium: up to 50 ml, up to 4.5 cm in diameter;
- large: more than 50 ml, more than 4.5 cm in diameter.
Symptoms
Intracerebral hemorrhage may be accompanied by three-phase (with the presence of a light gap) or the absence of a light gap. Consciousness in such patients is impaired (stupor or coma), which may be preceded by psychomotor agitation.
The severity and presence of focal symptoms will depend on the size and location of the hematoma. Most often, it is accompanied by unilateral muscle paresis, aphasia, epileptic seizures, a violation of the symmetry of tendon reflexes, and different pupil diameters. Also characterized by a lack of criticism, amnesia, behavior disorder.
Diagnostics
The diagnosis is made by a neurologist or neurosurgeon, often in consultation with a traumatologist.

To make a diagnosis, you need to contact a neurologist or neurosurgeon
To determine the localization of hemorrhage, the severity of the patient's condition and further management tactics, the following clinical and laboratory methods are used:
- Anamnesis collection, assessment of symptoms, complaints, objective condition.
- General clinical blood and urine tests.
- X-ray diagnostic methods: allow to identify the localization of the fracture (in 90% of cases, it coincides with the location of the hematoma).
- Magnetic resonance imaging.
- Cerebral angiography or magnetic resonance angiography (may indicate the site of rupture of blood vessels or other vascular disorders).
Treatment
Therapy can be conservative and operative.
Conservative treatment is carried out with the following hematoma sizes:
- epidural: up to 40-50 ml;
- subdural: thickness no more than 1 cm, displacement of cerebral structures up to 3 mm, volume up to 40 ml;
- intracerebral: the diameter does not exceed 3 cm.
Additional indications for conservative therapy:
- satisfactory state of consciousness of the patient and the absence of severe symptoms with a tendency to progression;
- absence of signs of compression of GM, dislocation syndrome.
Drugs used in treatment:
- to eliminate vasospasm: Aminocaproic acid, Vikasol, Aprotinin, Nifedipine;
- to prevent cerebral edema: Mannitol and other symptomatic drugs.
Often an urgent surgical intervention is performed, aimed at aspiration of the outflowing blood, removal of hematoma and crush foci, if any, elimination of brain compression, ligation of a bleeding vessel.

In some cases, surgery is required
Surgical intervention should always be accompanied by fluid therapy, including hemostatic, decongestant and other drugs.
Consequences of a brain hematoma
The consequences of a brain hematoma depend on its location and size, the patient's age, concomitant diseases, combination with other damage to the brain tissue and its membranes, the duration and degree of impairment of consciousness, the timeliness and usefulness of the provision of qualified assistance.
Mortality in subdural hematomas is 50–90%. A predictively favorable outcome is observed during the operation in the first 6 hours after injury. Mild hematoma often responds well to conservative treatment and resolves within 30-40 days. There are known cases of its chronicity.
With intracerebral hemorrhage, the most unfavorable outcome is in the case of blood breakthrough into the ventricles. 70% of patients after treatment have persistent disabling neurological deficit.
Brain hematoma is a dangerous condition that threatens the patient's life. The promptness and adequacy of treatment, resuscitation and rehabilitation measures are the most important steps in reducing the risk of death or disability.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.