- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Subdural hematoma of the brain: causes, symptoms, treatment, prognosis
The content of the article:
- The reasons
- Classification
-
Symptoms
- Classic version
- Subdural hematoma with or without a blurred "light" gap
-
Diagnostics and treatment
- Drug therapy
- Surgical intervention
- Forecast
- Video
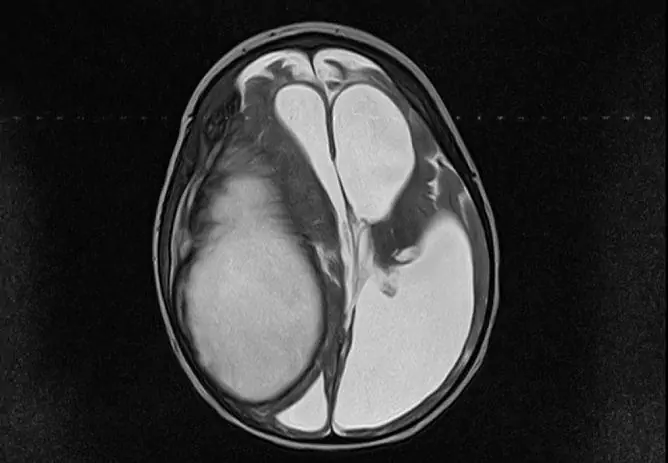
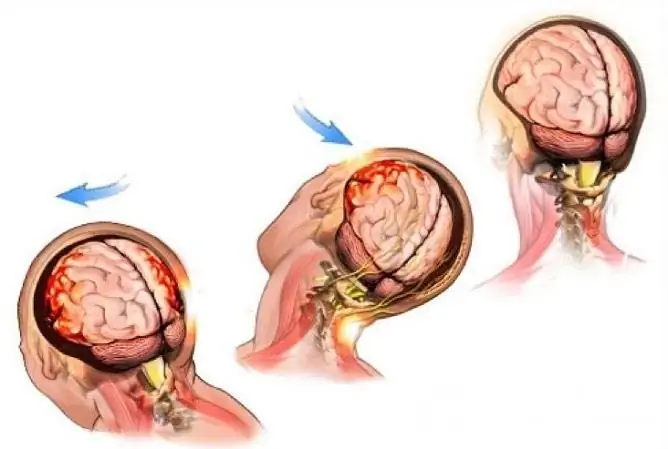
Subdural hematoma is an intracranial accumulation of blood between the meninges (arachnoid and hard). Most often, it occurs after trauma and manifests itself in the form of mental and consciousness disorders. In men, this pathology occurs three times more often than in women. In most cases, it occurs in people over forty.
Subdural hematoma occurs as a result of traumatic brain injury
Almost 22% of severe TBIs (traumatic brain injuries) are accompanied by the appearance of subdural hematoma. Unlike epidural, subdural hemorrhage can form not only on the injured part of the head, but also on the opposite side.
The reasons
The reason for the appearance of a subdural hematoma of the brain can be:
- rupture of pial or cortical vessels that pass in the subdural space, resulting from traumatic brain injury. In this case, the head should be inactive, and the object with which the blow is struck should be small in area;
- a change in direction of movement or an abrupt stop when falling on your legs or on the buttocks. In this case, a sharp shaking of the head leads to a displacement of the brain inside the cranium, as a result of which the intracranial veins rupture;
- hitting the head on a massive, sedentary object. Hemorrhage is the result of the rupture of the veins flowing into the sagittal venous sinus. The most common cause of this type of injury is falling from a great height or supine, collision of motorcycles or cars;
- impact on the motionless head of an object with a volumetric contact area. Often, injuries of this type occur when heavy objects, logs, snow blocks, and the sides of cars fall on the head. In this case, there is also a rupture of the pontine veins that flow into the superior sagittal sinus;
- vascular-cerebral pathologies caused by systemic vasculitis, arterial hypertension or cerebral aneurysm;
- violation of blood clotting as a result of coagulopathy or uncontrolled intake of anticoagulants.
The shape and severity of the hemorrhage depends on many factors, including the direction of the blow
If several mechanisms of injury occur at the same time, the patient develops bilateral subdural hematomas.
Classification
Depending on the causes of subdural hematoma, determine:
- non-traumatic hemorrhage;
- traumatic hemorrhage (with the absence or presence of a penetrating wound).
Also, subdural hematomas are classified as follows:
| The form | Description |
| Acute subdural hematoma | Occurs in the first three days after TBI |
| Subacute subdural hematoma | From the moment of TBI, it takes from 3 to 14 days |
| Chronic subdural hematoma | Occurs later than two weeks after injury, while it is limited to a capsule formed due to the activation of fibroblasts of the dura mater |
For an acute subdural form to form, the traumatic brain injury must be severe. For the appearance of an acute and subacute form, a slight injury is enough.
A lamellar subdural hematoma is a hemorrhage of a small volume (up to 50 ml), which, when conducting a CT scan, does not displace the ventricular system of the brain.
Depending on the mechanism of hemorrhage formation, they are classified as follows:
- homolateral: in this case, the area of the traumatic agent is small, and it is applied to a motionless or inactive head;
- contralateral: occur when the head is in motion, on a motionless or massive object, or as a result of injury to the agent by a wide object of the motionless head.
Symptoms
With subdural hematoma, the patient has local, cerebral and secondary stem symptoms. It is caused by compression of the brain and increased intracranial pressure. Particular attention is paid to the "light" interval (the period after the injury, during which there are no symptoms indicating the presence of hemorrhage).
In severe TBI, it can be several minutes, while in subacute or chronic form, it stretches for several weeks or even months.
In some cases, the appearance of signs of pathology causes additional trauma or a sharp jump in blood pressure. Most often, the change in the state of consciousness occurs gradually. In rare cases, the patient suddenly falls into a coma (as with an epidural hemorrhage).
The most important role among the focal signs of trauma is played by unilateral dilation of the pupil, in which its reaction to light decreases:
- acute form of the disease: the pupil is maximally dilated and practically does not react to light;
- subacute and chronic form of the disease: moderate mydriasis occurs (while the pupil's reaction to light persists).

Headache is one of the symptoms of pathology
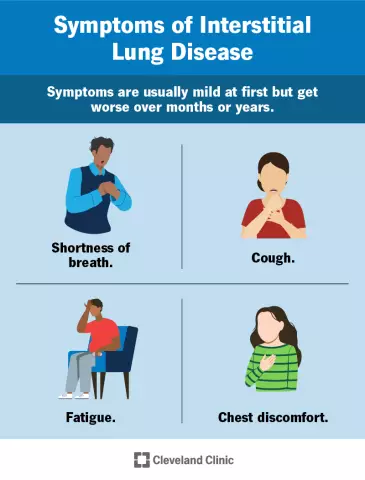
Another persistent symptom of subdural hematoma is a bursting headache. It accompanies the patient almost constantly, radiates to the eye area or the back of the head and intensifies with the movement of the eyeballs. Cephalalgia is aggravated by tapping on the skull and may be accompanied by nausea, vomiting, and photophobia.
The patient often has a disintegration of consciousness in the form of the following manifestations:
- mental disorders occurring with impaired attention, thinking, confusion;
- confusion, incoherence of speech and thinking, chaotic movements;
- "Frontal" psyche, a decrease in criticism of one's condition;
- violation of behavior;
- a state of euphoria.
Pathology can be accompanied by a change in muscle tone, a person begins to move too slowly, and the grasping reflex is disturbed.
Classic version
This variant of subdural hematoma is quite rare. It is characterized by the following clinical picture:
- short-term loss of consciousness at the time of traumatic brain injury;
- the duration of the light interval is from 10 minutes to 2 days.
The patient has headache, dizziness, and nausea. At the next stage, drowsiness appears, the headache increases sharply, the person becomes inadequate. Homolateral mydriasis is clearly manifested. Along with the loss of consciousness, the breathing rhythm changes, blood pressure rises, and tonic convulsions occur.
Subdural hematoma with or without a blurred "light" gap
This variant is typical for severe brain injuries. Initial loss of consciousness can easily develop into a coma. In the future, it is possible to restore consciousness, while psychomotor agitation is noted, headache and nausea occur. After a while, the patient again loses consciousness.
Diagnostics and treatment
In order to diagnose pathology after severe craniocerebral trauma, such examinations as: X-ray of the skull, Echo-EG, ophthalmoscopy, CT or MRI of the brain are carried out.

The diagnosis is confirmed by computed tomography
Drug therapy
Conservative treatment is carried out in the following cases:
- the victim is in a clear consciousness, has a hematoma less than 1 cm thick, with a displacement of cerebral structures up to 3 mm;
- no signs of brain compression;
- intracranial pressure does not exceed 25 mm Hg. Art.;
- stable neurological status.
Antifibrinolytic drugs (Vikasol, Aminocaproic acid) are used in complex therapy. Other medicines, depending on the goals of treatment:
- prevention of vasospasm: Nimodipine or Nifedipine;
- elimination of cerebral edema: Mannitol or Mannitol;
- relief of symptoms: antiemetic, anti-inflammatory, analgesic and sedative drugs.
With proper and timely treatment started, the bruising occurs within a month.
The patient is shown bed rest and long-term use of drugs that accelerate the resorption of hemorrhage. Traditional medicine methods for such injuries do not have the necessary effect. This approach to treatment contributes to the deterioration of the patient's health and the chronicity of the process.
Surgical intervention
For acute and subacute subdural hematomas, causing compression and displacement of the brain, immediate surgical intervention is indicated. The sooner the hemorrhage is eliminated, the greater the patient's chances of recovery.

The need for surgical intervention is determined by the doctor after conducting diagnostic tests.
Also, the operation is indicated in the subacute form, if the patient develops signs of intracranial hypertension or focal symptoms increase.
The operation can also be performed for chronic hematoma: surgical intervention may be necessary if the patient's condition worsens, congestion occurs in the fundus and headaches increase. In this case, closed external drainage is performed.
Forecast
With this type of injury, death occurs in 50-60% of cases. Elderly patients die more often. The most favorable prognosis for patients who underwent surgery within the first six hours after traumatic brain injury.
Mild forms of hemorrhage respond to conservative treatment and resolve within a month. In some cases, there is a transformation into a chronic form.
The threat of death persists even after removal of the hemorrhage by surgical intervention, since an increase in cerebral edema is possible in the postoperative period.

Wear protective equipment when engaging in traumatic sports.
In order to avoid the occurrence of injuries and hemorrhages, you must follow the safety rules. When riding motorcycles, roller skating, extreme sports, or on construction sites, a safety helmet must be worn.
Specialists such as a neurosurgeon, traumatologist and neurologist are involved in eliminating the consequences of TBI. For any traumatic brain injury, you should consult a doctor.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.