- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Brain abscess
The content of the article:
- Features of the disease
- Development stages
-
Causes
Causative agents
- Brain abscess symptoms
-
Brain abscess treatment
- Conservative therapy
- Surgery
- Effects
- Video
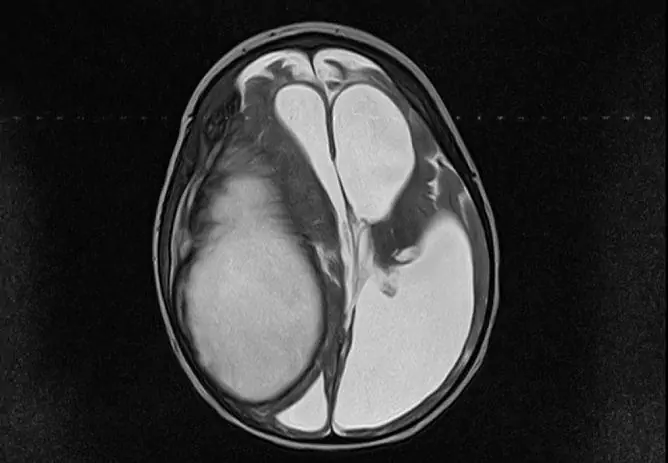
A brain abscess is a local formation of an infectious nature, which is an accumulation of pus isolated from healthy brain tissue by a hard connective tissue capsule. It makes up no more than 1-2% of all intracranial formations. It can occur at any age, but most often occurs in people over 40. Men are more often affected.

Brain abscess is of inflammatory or post-traumatic origin
Features of the disease
- The focus has a strictly infectious nature, depending on the specific pathogen, the variant of etiotropic therapy depends.
- An abscess is represented by a cavity filled with purulent contents, which may be localized in different parts of the skull (frontal, parietal, occipital, temporal), which will explain the variability of the clinical picture.
- It is often difficult to distinguish a purulent cavity from benign and malignant neoplasms from CT / MRI scans, therefore it is classified as a potentially life-threatening condition.
- Rarely are multiple purulent cysts (echinococcal, for example), more often it is a single formation with clear even contours.
- People with impaired immune response (HIV-infected) are at risk for developing brain abscesses.
- The prognosis depends on the duration and extent of the brain damage.
Development stages
|
Stage |
Characteristic |
| Early cerebritis (1-3 days) | The period is associated with a non-encapsulated focus of infection, that is, the inflammatory focus is not yet clearly limited to a healthy brain substance. With a histological examination at this stage, it is possible to detect the pathogen surrounded by a zone of perivascular infiltration (an accumulation of various cells like neutrophils and monocytes). |
| Late cerebritis (4-9 days) | The gradual spread of inflammation to neighboring areas and the appearance of necrosis in the center of the infectious focus (the beginning of the formation of a small purulent cavity in the center). At the edges of the inflammation, an accumulation of fibroblasts and macrophages begins. The lesion site loses the vascular network due to severe edema. |
| Stage of early formation of the capsule (10-13 days) |
Reduction of the inflammatory process and a significant increase in the number of fibroblasts at the border. A clear lack of vascularization in the affected area. Collagen maturation and formation of a fibrous capsule rudiment. |
| Stage of late formation of the capsule (14 days or more) | Final formation of the capsule and gradual regression of signs of inflammation. At this point, the abscess has a fully formed appearance (the layers are presented from the inside to the outside): the necrotic center, the peripheral zone of inflammatory cells and fibroblasts, a collagen capsule, a new vasculature, an area of reactive gliosis with edema. |
The severity of the manifestations of the disease has a clear dependence not only on the type of pathogen, but also on the state of the human immune system.
Causes
A brain abscess is an infectious disease, the main reasons for its occurrence include:
- Purulent processes in the nasal cavity (sinusitis, sinusitis). In this case, there is a direct contact between the purulent focus and the cranial cavity. Such abscesses are called rhinogenic.
- Inflammatory diseases of dental origin (tooth cysts, caries complications). There is also direct contact between the cranial cavity and the purulent focus, these are odontogenic formations.
- Infectious processes in the outer, middle or inner ear (otitis media, labyrinthitis). The abscess often breaks directly into the cranial cavity (otogenic abscesses).
- Purulent processes that are located at a considerable distance from the brain. In this case, by the hematogenous or lymphogenous route, the pathogen passes through the blood-brain barrier and enters the brain. The foci of infection can be located in different areas (intra-abdominal or pelvic infection, pneumonia, boils, osteomyelitis). In this case, there are a number of unique features in the formation that has arisen in the brain: localization at the border of the gray and white matter of the brain or in the basin of the middle cerebral artery; poorly expressed capsule; multiple foci. Such abscesses are called metastatic abscesses.
- Post-traumatic abscesses that occur as a complication of traumatic brain injury. By the time of occurrence, they can be divided into early (up to 3 months after TBI) and late (after 3 months). More often such abscesses are multi-chambered.
The contributing factors are:
- immunodeficiency states;
- long-term persistent untreated infections.
In all cases, the pathology under consideration acts as a complication of infectious processes in the body, i.e., secondary. In the case of the appearance of an abscess as an independent disease (idiopathic form), a course of diagnostic measures is shown to exclude oncological processes.
Causative agents
Not all pathogenic organisms are able to pass through the blood-brain barrier and enter the brain cavity. The main pathogens that can penetrate the blood-brain barrier and cause the formation of a focus in the brain are presented in the table.
| View | Representatives |
| Bacteria | Streptococcus aerobic and anaerobic, Staphylococcus aureus, Proteus, Klebsiella, Enterobacteriaceae, Listeria. |
| Mushrooms | Candida albicans, Histoplasma capsulatum, Aspergillus. |
| The simplest. | Toxoplasma gondii |
Brain abscess symptoms
Clinical manifestations depend on the specific affected area. Leading signs:
- With a small size of education (less than 1 cm), it has an asymptomatic course and is detected as an accidental finding.
- Severe headache is the most common symptom of the disease. It occurs due to compression of the nerve trunks.
- Nausea / vomiting of central origin due to increased intracranial pressure. Such vomiting does not bring relief to the patient, unlike vomiting with intestinal infections, for example.
- Intoxication (fever, lethargy, weakness) develops in only half of all cases.
- Convulsive syndrome occurs in 20-30% of cases. It is associated with the appearance of zones of increased excitability in the central nervous system and can manifest itself as both local and generalized seizures.
- Impaired visual acuity due to swelling of the optic nerve.
- Violation of the mental status (seizures, depression).
- Focal symptoms depend on the lobe involved (neurology is part of the classic triad of symptoms along with headache and nausea).
Symptoms depending on the level of damage:
| Localization | Leading signs |
| Brain stem | Paresis of the cranial nerves in combination with motor and sensory disorders of any genesis. |
| Cerebellum | Nystagmus, ataxia, pronounced nausea / vomiting, dysmetria, meningism. |
| Occipital lobe | Severe headache, hemianopsia (bilateral blindness in half of the visual fields). |
| Parietal lobes | Violation of orientation in space, recognition of objects by touch, loss of visual fields. |
| Temporal lobes | Impaired speech understanding, ipsilateral headache, sensory disorders. |
| Frontal lobe | Attention and memory disorders, mental personality disorders, movement disorders. |
| Paraventricular arrangement | When an abscess breaks out, the patient's condition worsens. |
A list of the most typical focal symptoms is given, but in each specific case, the manifestations vary somewhat (especially if several areas are involved).
Brain abscess treatment
Treatment requires an integrated approach, using conservative or surgical methods.
Conservative therapy
The tactics of drug therapy:
- Before prescribing drug therapy, obtain material from the focus of infection and send it for bacteriological examination to establish a specific pathogen.
- Until the main pathogen is identified, a course of empirical antibiotic therapy is prescribed, aimed at suppressing the maximum possible number of pathogens. This is done in order to stop the development of the infectious process until the analysis is ready.
Empiric therapy has features depending on the specific pathology that caused the abscess:
- otitis media - Metronidazole and 3rd generation cephalosporins;
- sinusitis - Metronidazole, 3rd generation cephalosporins, and Vancomycin;
- odontogenic infections - Penicillin and Metronidazole;
- penetrating TBI - Vancomycin, 3rd or 4th generation cephalosporins.
Treatment options for focal brain damage, depending on the pathogen, are presented in the table.
| Causative agent | Drugs |
| Streptococcus | Penicillin, Cefotaxime, Ceftriaxone, Vancomycin |
| Staphylococcus aureus | Oxacillin, Vancomycin |
| Enterobacteriaceae (Salmonella, Escherichia coli) | Cefotaxime, Cefepim, Meropenem, fluoroquinolones (Levofloxacin) |
| Haemophilus influenzae | Ceftriaxone, fluoroquinolones (Ciprofloxacin, Ofloxacin) |
| Mycobacteria | Isoniazid, Rifampicin, Pyrazinamide, Ethambutol (simultaneously) |
| Candida albicans | Fluconazole, Amphotericin B |
| Aspergillus | Voriconazole, Amphotericin B, Posaconazole |
In addition to the main therapy, a number of other drugs are shown:
- Corticosteroids - can somewhat reduce local edema in the tissues and reduce intracranial pressure (Prednisolone).
- Anticonvulsants - to remove pathological foci of arousal and thereby eliminate convulsive syndrome (Phenobarbital, Gabapentin).
- Analgesics and non-steroidal anti-inflammatory drugs - to reduce headaches (Analgin, Paracetamol).
Depending on the clinical manifestations, a number of other drugs (antiemetic, etc.) may be additionally prescribed. The duration of treatment is on average 6-8 weeks of high-dose antibiotic therapy.
Surgery
Surgical methods are considered only if the lesion is larger than 1.5-2 cm (before that, the patient is being treated using conservative methods).

Surgical intervention is used for large brain abscesses
It is characterized by complete or partial removal of the formation and is represented by two options for operations:
- Open removal with capsule. This type of operation is highly traumatic, since it involves wide access to the tissues of the skull (trepanation). It is produced only in cases where the formation lies superficially and has a hard capsule. If the lesion is located relatively deep and affects the base of the brain, such intervention is contraindicated due to the high risk of death.
- Puncture aspiration - refers to minimally invasive methods of treatment and is possible even in critically ill patients. It is performed under close visual control (CT / MRI). Allows not only to aspirate the contents of the cyst, but also to fenestrate the capsule.
Any option is possible only after a thorough diagnosis and exclusion of benign and malignant tumors. If it is impossible to differentiate, an open operation is required, since the puncture is fraught with total seeding of the brain with tumor cells.
Effects
With timely treatment, the pathology has a minimum of consequences, but taking into account the fact that the brain substance is involved, it does not pass completely without a trace.
Possible consequences:
- The development of zones of increased excitability in the brain with the formation of epileptic seizures (in severe cases - status).
- Irreversible impairment of some functions, depending on the location of the abscess (impaired speech, writing, attention, vision). Possible complete or partial loss of any kind of sensitivity and persistent disorders in the motor sphere.
- Development of sepsis with delayed treatment.
- Fatal outcome with a massive purulent process (relatively rare).
The development of possible complications is associated not only with the abscess itself, but also with the risks of its surgical treatment (thrombosis, for example).
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!