- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Lung abscess
The content of the article:
- Description and etiology of the disease
- Lung abscess symptoms
- Diagnostic methods
-
Lung abscess treatment
- Basic principles
- Conservative treatment
- Surgery
- Prevention
- Prognosis and complications
- Video
A lung abscess is a limited focus of purulent inflammation in the lung parenchyma. The disease develops when pyogenic bacteria enter the lung tissue through the bronchi, with blood or lymph flow. An abscess of the right or left lung can form in everyone, but most often middle-aged men with concomitant diseases (diabetes mellitus, alcoholism) are ill. It is necessary to treat the disease in a hospital setting, antibacterial agents, mucolytics and restorative drugs are prescribed.

Lung abscess is a potentially fatal disease, therefore requires an extremely serious approach
Description and etiology of the disease
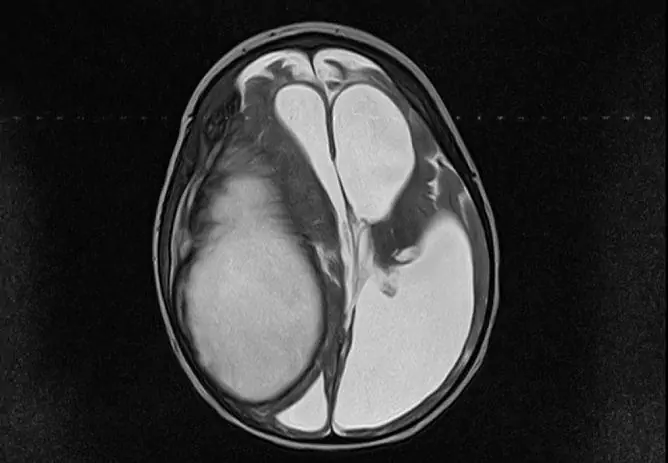
An abscess is a limited cavity that fills with pus (seen in the photo). The wall of the abscess has a protective function - it limits the spread of infection to the surrounding tissues.
The reason for its formation is the ingress of bacteria into the lung tissue, which leads to its purulent fusion.
In most cases, an acute abscess develops as a complication of pneumonia. The causative agents are non-specific microorganisms: streptococci, pneumococci, Staphylococcus aureus.
Several factors contribute to the development of infection:
- Complication of lung infarction (secondary infection).
- The presence of a patient with chronic diseases that reduce local and general immunity: diabetes mellitus, alcoholism, lung disease, bronchiectasis, HIV infection.
- Aspiration of infected contents of the nasal cavity, paranasal sinuses, tonsils.
- Aspiration of vomit.
- The penetration of bacteria into the lung tissue by the hematogenous route (with blood flow) from foci of osteomyelitis.
- The ingress of bacteria by the lymphogenous route (with lymph flow) with furunculosis, phlegmon in the face area.
Lung abscess symptoms
The disease begins acutely with the onset of symptoms of intoxication:
- an increase in body temperature up to 38-39 ° С;
- general weakness, lethargy, increased fatigue;
- chills;
- loss of appetite;
- headache;
- depression of consciousness, drowsiness.
Then local symptoms join: cough, chest pain. The cough at the beginning of the disease is dry, then sputum appears. Pain in the chest occurs localized, increases with deep breathing and coughing. Cough and chest pain are often accompanied by shortness of breath, which increases with exertion. The larger the abscess, the more severe the shortness of breath. These symptoms persist for 7-14 days before opening the abscess in the bronchus.
After opening the abscess, the clinical picture changes. The cough becomes moist, there is an abundant discharge of purulent sputum (yellow-green, unpleasant odor, up to 1 liter). The patient's well-being after this usually improves - the body temperature decreases, the severity of shortness of breath decreases, and the appetite normalizes. However, residual effects can persist for a long time (1-2 months).
Diagnostic methods
A preliminary diagnosis is made based on the clinic (acute course, fever, cough with discharge of pus, chest pain) and physical examination data. The doctor, during a physical examination, reveals the following signs of the disease:
- percussion is determined by the dullness of sound over the lesion;
- with auscultation, weakened breathing over the abscess cavity is heard;
- in the presence of a message of an abscess with a bronchus, bronchial respiration.
To confirm the diagnosis and carry out differential diagnostics, additional tests are prescribed - laboratory and instrumental.
| Diagnostic method | Indications, research results |
| Complete blood count (CBC) |
In the UAC, signs of an active inflammatory process are determined: · Increase in the level of leukocytes due to neutrophils; · Shift of the leukocyte formula to the left; · Increased ESR. |
| General sputum analysis |
In an acute abscess, the following changes are determined: Purulent sputum; · A lot of elastic fibers (indicates the breakdown of lung tissue); Leukocytes, columnar epithelium (signs of inflammation); Alveolar cells (a sign indicates the involvement of lung tissue in the necrotic process). To determine the pathogen, a bacterioscopic and bacteriological examination of sputum is prescribed. |
| Plain chest x-ray |
Plain radiography is one of the main methods for diagnosing the disease. At the initial stage, a homogeneous rounded darkening is determined, after the abscess breaks through, a rounded darkening with a liquid level (in the form of a basket). |
| Computed tomography (CT) | If plain x-ray is ineffective, computed tomography is prescribed. This is a more informative and specific research method, but at the same time, it is more expensive. It is possible to identify the size and exact localization of the formation, its connection with the bronchus. |
Lung abscess treatment
Treatment of the disease should be carried out in a hospital setting. The duration of therapy can be 6-8 weeks, it depends on the size of the cavity, the severity of the condition, the presence of concomitant diseases. Treatment can be conservative or surgical. Additionally, bed rest, diet, and abundant drinking are prescribed.
Basic principles
Adherence to the following recommendations will help speed up the healing process and reduce the likelihood of complications:
- During the day, drink 1.5 liters of clean water, warm tea, herbal teas, fruit drinks and diluted juices. A plentiful drinking regime reduces the severity of intoxication, dilutes phlegm.
- Observe bed rest in the acute period of the disease.
- Improve the drainage function of the bronchi, taking a position with the legs raised by 10-20 cm (drainage position). You need to be in this position several times a day for 30 minutes.
- Eat a high-calorie diet high in protein and vitamins. During the period of illness and recovery, it is recommended to eat more meat, fish, cottage cheese, vegetables and fruits.

Lung abscess is treated in a stationary setting
Conservative treatment
Conservative treatment consists in the use of medications - antibiotics, mucolytics, restorative agents. The duration of conservative treatment is 6-8 weeks, if it is ineffective, surgical methods are used.
| Group of medicines | Indications, mechanism of action |
| Antibacterial agents |
The use of antibiotics refers to etiotropic treatment (aimed at eliminating the cause). At the onset of the disease, antibacterial agents are prescribed empirically, after receiving the results of bacteriological research, the drug is changed if necessary. What groups of antibiotics are most often prescribed: 1. Protected penicillins: Amoxiclav, Sulbatsim. 2. Lincosamides in combination with aminoglycosides: Clindamycin and Streptomycin. 3. In severe cases, drugs from the carbapenem group may be prescribed. |
| Expectorants |
To improve drainage function, expectorant drugs are prescribed. They thin the phlegm, improve the functioning of the cilia of the mucous membrane, which facilitates the discharge of phlegm. Acetylcysteine, Bromhexine, Ambroxol may be prescribed. |
Surgery
If the use of medications is ineffective, they switch to surgical treatment. What surgical methods can be used:
- Bronchoalveolar lavage. The procedure consists in aspiration of the contents of the abscess, followed by the introduction of antiseptic solutions.
- Introduction of antibacterial agents into the abscess cavity.
- Transthoracic puncture - aspiration of purulent contents through a skin puncture is performed.
Prevention
Prevention consists in preventing the entry of microorganisms into the lung tissue and strengthening the immune system. What non-specific preventive measures are carried out:
- Restoration of the drainage function of the bronchi in pneumonia, bronchitis and other diseases of the respiratory system.
- Compensation for chronic diseases that reduce general and local immunity.
- An early visit to a doctor when symptoms of the disease appear.
- Remediation of foci of infection (chronic tonsillitis, rhinitis, sinusitis).
Prognosis and complications
In most cases, the prognosis is favorable - complete recovery, less often the acute process turns into a chronic one. The development of complications is possible, the most dangerous are pyopneumothorax (pus entering the pleural cavity), pleural empyema, pulmonary hemorrhage. Death occurs in 5-10% of cases. The risk of complications increases with late initiation of therapy, non-compliance with medical recommendations, and the presence of concomitant diseases.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!