- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Alveolitis
The content of the article:
- Causes and risk factors
- Forms of the disease
- Disease stages
- Alveolitis symptoms
- Diagnostics
- Alveolitis treatment
- Possible complications of alveolitis and consequences
- Forecast
- Prevention
Alveolitis is a diffuse inflammatory lesion of the alveolar and interstitial lung tissue, which can occur in isolation or develop against the background of other diseases.
The pulmonary alveoli take part in the act of breathing, providing gas exchange with the pulmonary capillaries, and are the end part of the respiratory apparatus. The total number of alveoli reaches 600-700 million in both lungs.

Alveolitis is characterized by inflammation of the pulmonary alveoli
Causes and risk factors
Exogenous allergic alveolitis develops against the background of allergic reactions (plant and house dust, medicines, pet hair, components of microscopic fungi, industrial irritants, etc.) are often allergens. The ingestion of the allergen into the body causes the formation of IgG. Immune complexes (antigen-antibody) settle on the surface of the alveoli, which causes damage to the cell membrane, the release of a significant amount of biologically active substances with the development of an inflammatory process. In the development of this form of alveolitis, an important role is played by the repeated entry of the allergen into the body.

Dust allergy can lead to the development of allergic alveolitis
The causes of idiopathic fibrosing alveolitis have not been fully elucidated. It is assumed that the disease may be of an autoimmune nature, occur against the background of infection with certain viruses (hepatitis C virus, herpes virus, cytomegalovirus, adenoviruses). Risk factors for developing this form of the disease include work in the agricultural sector, woodworking, metallurgy, and smoking. In this case, the inflammatory process in the pulmonary alveoli leads to an irreversible thickening of their walls with a subsequent decrease in permeability for gas exchange.
The main reason for the development of toxic fibrosing alveolitis is the direct or indirect effect on the lungs of toxic substances that enter the pulmonary alveoli by hematogenous or aerogenic means (among others, such drugs as Azathioprine, Mercaptopurine, Methotrexate, Furadonin, Cyclophosphamide).
Secondary alveolitis occurs against the background of other pathological processes. Most often it is sarcoidosis, tuberculosis, diffuse connective tissue diseases.
Risk factors include:
- genetic predisposition;
- immunodeficiency states;
- collagen metabolism disorders.
Forms of the disease
Depending on the etiological factor, as well as the characteristics of the course of the disease, there are:
- idiopathic fibrosing alveolitis;
- toxic fibrosing alveolitis;
- exogenous allergic alveolitis.

Lungs with fibrosing alveolitis
Alveolitis can be primary and secondary, as well as acute, subacute and chronic.
Disease stages
Depending on the histological picture, there are five stages of idiopathic fibrosing alveolitis:
- Infiltration and thickening of the septa of the pulmonary alveoli.
- Filling the pulmonary alveoli with cellular composition and exudate.
- Destruction of the pulmonary alveoli.
- Changes in the structure of the lung tissue.
- Formation of cystic-altered cavities.
Alveolitis symptoms
The symptoms of alveolitis vary depending on the form of the disease, but there are a number of manifestations common to all forms of pulmonary alveolitis. The main symptom is shortness of breath, which at the initial stage of the disease occurs after physical exertion, but as the pathological process progresses, it begins to manifest itself at rest. In addition, patients complain of a dry, unproductive cough, rapid fatigue, soreness in muscles and joints. In the later stages of the disease, weight loss, cyanosis of the skin, as well as changes in the shape of fingers ("drum sticks") and nails ("watch glasses") are observed.

Shortness of breath is the first symptom of alveolitis
The first symptoms of acute exogenous allergic alveolitis may appear within a few hours after contact with the allergen. Moreover, the general signs of the disease resemble the clinical picture of influenza. In patients, the body temperature rises, chills, headache appear, then cough and shortness of breath, heaviness and pain in the chest occur. In children with some allergic diseases, in the initial stages of exogenous allergic alveolitis, asthmatic dyspnea occurs, and sometimes asthma attacks. On auscultation, finely bubbling moist rales are heard over almost the entire surface of the lungs. After excluding contact with the allergen that caused the development of the disease, the symptoms disappear within a few days, but return with subsequent contact with the causative allergen. At the same time, general weakness, as well as shortness of breath, which is aggravated by physical exertion, can persist in the patient for several more weeks.
The chronic form of exogenous allergic alveolitis can occur with repeated episodes of acute or subacute alveolitis or independently. This form of the disease is manifested by inspiratory dyspnea, persistent cough, weight loss, and deterioration in the patient's general condition.
Idiopathic fibrosing alveolitis develops gradually, while the patient has irreversible changes in the pulmonary alveoli, which is expressed in increasing shortness of breath. In addition to severe shortness of breath, patients complain of pain under the shoulder blades, which interfere with a deep breath, and fever. With the progression of the pathological process, hypoxemia (a decrease in the oxygen content in the blood), right ventricular failure, and pulmonary hypertension increase. The terminal stage of the disease is characterized by pronounced signs of respiratory failure, enlargement and expansion of the right heart (cor pulmonale).

In idiopathic fibrosing alveolitis, patients complain of pain under the scapula
The main signs of toxic fibrosing alveolitis are shortness of breath and dry cough. During auscultation of the lungs, patients have tender crepitus.
Diagnostics
The diagnosis is determined on the basis of data obtained during the collection of complaints and anamnesis, physical diagnostics, examination of the function of external respiration, and radiography of the lungs.
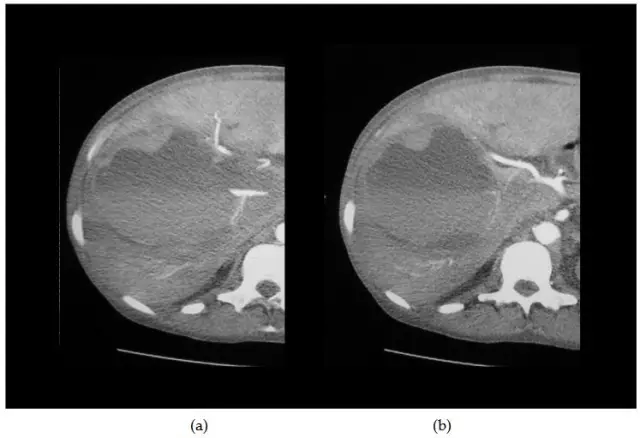
During an X-ray examination with exogenous allergic alveolitis, a decrease in the transparency of the lung tissue with the formation of a large number of small focal shadows is revealed. In order to confirm the diagnosis, laboratory immunological diagnostics, provocative inhalation tests, computed tomography of the lungs are carried out. In diagnostically difficult cases, they resort to a biopsy of the lung tissue followed by a histological examination of the material obtained.
Exogenous allergic alveolitis is differentiated from bronchial asthma, atypical pneumonia, tuberculosis, sarcoidosis, and other forms of pulmonary alveolitis.

Exogenous alveolitis of the lungs on x-ray
In the case of idiopathic fibrosing alveolitis, small-focal diffuse changes, more pronounced in the lower parts, are determined on the roentgenogram of the lungs on both sides. In the later stages of the disease, secondary cystic changes are detected in the lung tissue. The data of computed tomography of the lungs allow you to determine the area of altered lung tissue for subsequent biopsy. The results of the electrocardiogram indicate the presence of hypertrophy and overload of the right heart.
Differential diagnosis of this form of alveolitis is carried out with pneumonia, granulomatosis, pneumoconiosis, diffuse forms of amyloidosis and lung neoplasms.
Radiological changes in acute toxic fibrosing alveolitis may be absent. Further, deformation and diffuse enhancement of the pulmonary pattern, as well as diffuse fibrosis, are determined.
Alveolitis treatment
The tactics of treating alveolitis depends on the form of the disease. In some cases, the patient may need to be hospitalized.
The effectiveness of treatment of idiopathic fibrosing alveolitis decreases as the pathological process progresses, so it is important to start it at an early stage. Drug therapy for this form of the disease consists in the use of glucocorticoids, if this is not enough, immunosuppressants and bronchodilators are prescribed. With the progression of the disease, the therapeutic effect is provided by plasmapheresis. Surgical treatment of this form of the disease involves lung transplantation. Indications for it are dyspnea, severe hypoxemia, decreased diffusion capacity of the lungs.
In case of alveolitis of allergic and toxic etiology, in addition to the main treatment, it is necessary to eliminate or to limit as much as possible the effect on the patient's body of allergic or toxic agents, contact with which caused the development of the disease. In milder forms of alveolitis, this, as a rule, is sufficient for the disappearance of all clinical signs; the need for drug treatment may not arise.

Treatment of pulmonary alveolitis is mostly conservative, in severe cases, lung transplantation is required
In the treatment of severe forms of exogenous allergic alveolitis, glucocorticoids, inhaled bronchodilators, bronchodilators, and oxygen therapy are used.
In case of toxic fibrosing alveolitis, mucolytics and glucocorticoids (oral or inhalation) are prescribed.
In all forms of alveolitis, in addition to the main treatment, the intake of vitamin complexes, potassium preparations, as well as the performance of breathing exercises (therapeutic respiratory gymnastics) are indicated.
Possible complications of alveolitis and consequences
Complications of alveolitis can be chronic bronchitis, pulmonary hypertension, cor pulmonale, right ventricular heart failure, interstitial fibrosis, pulmonary emphysema, respiratory failure, pulmonary edema.
Forecast
With timely adequate treatment of acute exogenous allergic, as well as toxic fibrosing alveolitis, the prognosis is usually favorable. With the transition of the disease into a chronic form, the prognosis worsens.
Idiopathic fibrosing alveolitis is prone to gradual progression with the development of complications. Due to the growing irreversible changes in the alveolar-capillary system of the lungs, the risk of death is high. The five-year survival rate after surgical treatment reaches 50-60%.
Prevention
In order to prevent the development of alveolitis, it is recommended to timely and adequately treat infectious diseases, limit contact with potentially dangerous allergens, exclude household and professional factors that can cause the development of a pathological process, observe occupational hygiene rules, and also give up bad habits.
Persons at risk of alveolitis should regularly undergo preventive medical examinations.
YouTube video related to the article:

Anna Aksenova Medical journalist About the author
Education: 2004-2007 "First Kiev Medical College" specialty "Laboratory Diagnostics".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!