Epidural hematoma of the brain: symptoms, treatment, prognosis and consequences
The content of the article:
-
Symptoms
- Blurred light period flow
- Hematoma without light period
- Diagnostics
-
Therapy
- Conservative treatment
- Surgical intervention
- Closed external drainage
- Forecast and possible consequences
- Video
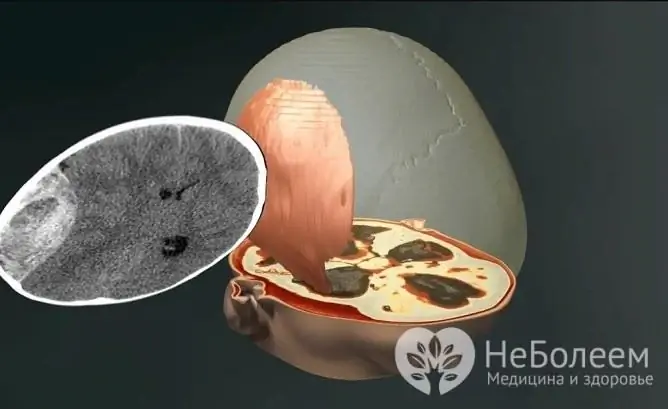
Epidural hematoma is caused by traumatic brain injury (TBI) and is a collection of blood that fills the space between the hard cerebral membrane and the bones of the skull.

Epidural hematoma formation occurs as a result of traumatic brain injury
Epidural hematomas are characterized by a traumatic origin. The most common cause of its formation is the following mechanisms of action:
- blow with a medium-sized object on the head: a stone, a hammer, etc.;
- hitting your head on a stationary object: falling from a small height, hitting a step, table corner, etc.
The zone of contact in these cases is usually the inferior parietal or temporal region of the skull, and the source of bleeding is the diploic and meningeal veins, venous sinuses, the middle meningeal artery and its branches.
Symptoms
In most cases, there are characteristic clinical manifestations of epidural hemorrhage. It is characterized by a pronounced light interval - the victim loses consciousness for a short time, which is then restored, but some stunnedness remains.

Pathology is manifested by a moderate headache
The main complaints are: mild headache, weakness and dizziness. Initially, this condition is regarded as mild to moderate TBI.
When the light period passes, the patient's well-being sharply worsens, the following symptoms appear:
- nausea and vomiting;
- acute growing headache;
- psychomotor agitation;
- rapidly progressive disorder of consciousness - from stunnedness to deep depression of consciousness and coma.
In some cases, the rapid extinction of consciousness immediately turns into a coma, which can cause concomitant arterial hypertension, bradycardia, increasing brachiocephalic paresis of contralateral hematoma of the extremities and side of the face.
The pupil of the eye on the side corresponding to the site of injury dilates with a consequent lack of response to light. Sometimes, focal symptoms (anisocoria and paresis) are prioritized, which outpace the appearance of symptoms of brain compression.
Blurred light period flow
Perhaps the course of pathology with an erased light period. This sign indicates profound impairment of consciousness and severe TBI. After several hours, the coma changes to an intermediate state - stupor, at which time the possibility of verbal contact with the victim is provided. The doctor, by his behavior, determines whether there is hemiparesis and how intense the headache is.
The severity of symptoms depends on the severity of the injury.
A light interval of this type can last from a couple of minutes to several days, and after it a sharp deterioration in the patient's well-being occurs - the growing excitement flows into a coma, and paresis is aggravated to a complete plegia of the extremities opposite to the side on which the hematoma was formed.
As a result, it is possible to develop disorders of vital functions and damage to the brain stem, which can manifest itself as severe oculomotor and vestibular disorders, hormone, etc.
Hematoma without light period
An epidural hematoma that occurs without a light period indicates multiple brain damage and severe TBI. Almost immediately after the blow, the victim falls into a coma and remains in this state unchanged.
The greatest duration of the light interval is found in subacute epidural hematomas and can reach from 10 to 12 days. The patient's consciousness during this period remains mostly clear, but some mild focal signs and a tendency to bradycardia are recorded.
In the future, gradually, sometimes in waves, disturbances of consciousness are aggravated up to deep sopor against the background of excitement and severe headache.
Depending on the place where the education is located, the focal symptoms differ, namely:
| Location of injury | Manifestations |
| Frontal lobe | Mental disorders with a frontal coloration against the background of a weak severity of other focal symptoms |
| Parasagittal region | Pyramidal disorders with the greatest severity of paresis in the foot |
| Occipital region |
Homonymous hemianopsia (loss of fields of the same name) |
Diagnostics
Epidural hematoma is diagnosed by a neurosurgeon or neurologist in conjunction with a traumatologist. The anamnesis, complaints of the victim and typical clinical manifestations - bradycardia, disturbance of consciousness, etc., are taken into account.
X-ray of the skull is mandatory, during which the presence of a fracture crossing the grooves of the meningeal vessels is established. In most of the victims, the localization of the formed cavity corresponds to the site of the fracture.

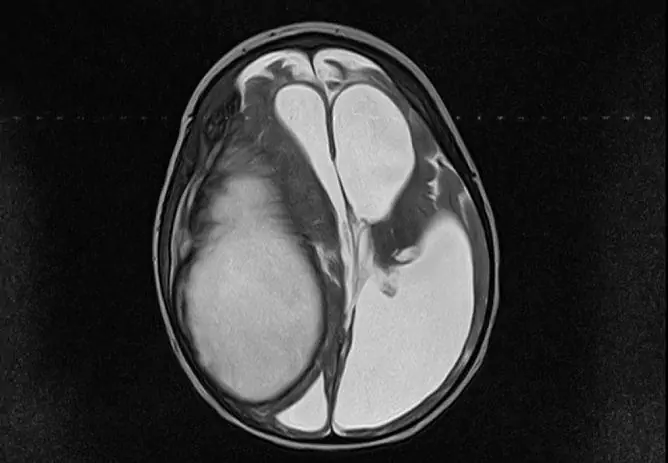
To clarify the diagnosis, CT or MRI is prescribed
Other diagnostic methods:
| Study | Description |
| Computed tomography (CT) | CT allows you to more accurately establish the volume of the formed hematoma and the place of its localization, and also gives more complete information about other intracranial injuries, if any |
| Magnetic resonance imaging (MRI) | MRI visualizes isodense and small lesions. It is used to assess the state of the brain stem and basal structures, as well as for the differential diagnosis of epidural and subdural hematomas. |
| Echoencephalography (Echo-EG) | If MRI or CT is not possible, Echo-EG of the brain is preferred. The study helps to determine the presence of a pathological volumetric process in the substance of the brain. Echoencephalography usually shows progressive displacement of the middle ear |
Therapy
Conservative treatment
If the volume of the formed cavity does not exceed 30-50 ml, the patient has no progressive symptoms and signs of brain compression, conservative treatment is possible.
Surgical intervention
For larger formations and the presence of compression of the brain, urgent surgical intervention is indicated. In such cases, a milling hole is made in the area of the skull with the assumed localization of the accumulation.
The choice of treatment tactics is determined by the degree of damage and its localization
Through it, using a special aspirator of blood clots and fluid, part of the hematoma is removed, after which craniotomy is performed with the removal of the formation in full and the ligation of the damaged vessel.
If the veins are the source of bleeding, they are coagulated, followed by tamponing with a hemostatic sponge. In cases of damage to the diploic veins, surgical wax is used, and if injuries of the sinuses are found, they are plastic and tamponade. At the end of the operation, a bone flap is placed in place and the wound is sutured on the surface of the scalp.
Simultaneously with the performed manipulations, hemostatic, anti-edematous and symptomatic treatment is used. During the recovery period, patients receive neurometabolic and resorption medications. To speed up the recovery process of the muscles of the paretic limbs, therapeutic massage and physical education are shown.
Closed external drainage
As an alternative to craniotomy, a minimally invasive surgical procedure - closed external drainage - can be chosen. This method is recognized as more gentle and has a number of advantages, however, it can be used only in cases where urgent removal of the formation is not required.

Minimally invasive surgical intervention is performed according to indications
An intraosseous needle is inserted through the skin to perforate the skull. A special drainage catheter is placed in the resulting hole, the diameter of which does not exceed 3 mm. A liquid receiver is attached to it, which is placed 15–20 cm below head level to ensure optimal outflow of liquid.
Forecast and possible consequences
The prognosis for epidural hematomas directly depends on the age of the patient, the volume of formation and the timing of the operation. The most favorable outcome is observed in the following cases:
- conservative treatment of small formations;
- surgical intervention at the stage of moderate decompensation. Moreover, the probability of restoration of lost neurological functions is the highest, and the risk of mortality is minimal.
When performing an operation at the stage of decompensation, the prognosis is the least positive. In 40% of cases, craniotomy is fatal, and surviving patients often have significant neurological deficits.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.