Fatty acids in feces in adults and children: causes, diagnosis, treatment
The content of the article:
- Reasons for the content of fatty acids and neutral fats in feces
- Features of steatorrhea in children
- Classification of steatorrhea
- Symptoms of steatorrhea
-
Diagnostics
Fecal lipidogram
- Treatment
Fatty acids in feces, as well as neutral fat or soap, are found in steatorrhea. What does it mean? Mainly, the fact that fat is not absorbed properly, and for whatever reason, the examination should show.

The causes of the appearance of fatty acids in feces are diseases of the digestive system or nutritional errors
A healthy body should assimilate from 90% to 98% of dietary fat. Normal feces do not contain triglycerides (neutral fats) and fatty acids. Their residual fragments can be found in feces in small quantities in the form of soaps.
Reasons for the content of fatty acids and neutral fats in feces
Reasons for insufficient absorption of fatty acids by the body:
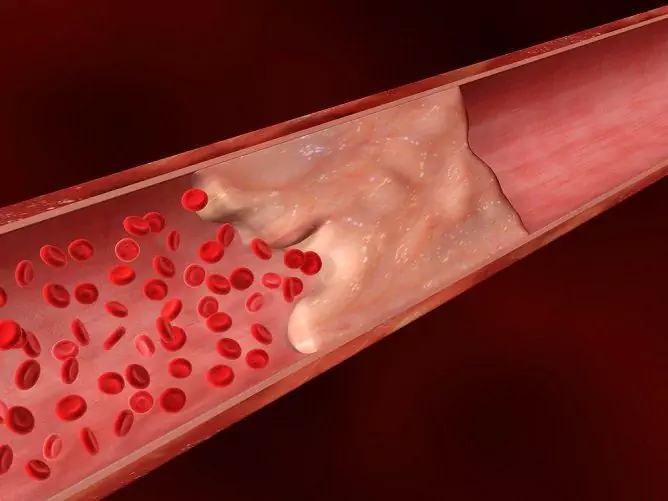
- dysfunction of the pancreas. To break down neutral fats in the intestine into glycerol and fatty acids, the pancreas synthesizes a water-soluble enzyme - pancreatic lipase. A decrease in the activity of the pancreas leads to a deficiency of lipase in the body, a violation of its digestive action. At the same time, triglycerides do not lend themselves to complete splitting, neutral fat appears in the feces;
- deficiency of bile acids. Insufficient flow of bile into the intestine leads to a violation of the breakdown and absorption of fats. Fats are available for the action of digestive enzymes only in the form of a thin emulsion. Bile performs the function of mixing fatty masses with water, which is necessary for their digestion. In case of a lack of bile, the fat drops remain so large that aqueous solutions of enzymes cannot mix with them. As a result, fats are not completely digested and are found in feces;
- violation of absorption (malabsorption) of fat in the intestine and accelerated evacuation from the rectum. The movement of the food lump (chyme) occurs due to the undulating contractions of the intestinal walls. Violations of its motor function, accelerated movement and evacuation of food masses from the intestines leads to the fact that fats do not have time to be completely absorbed. As a result, the general appearance of feces changes, they acquire a light, grayish tint, a greasy sheen and an unpleasant odor that is not characteristic of them;
- excessive fat content in the diet, especially refractory (for example, lamb fat);
- taking castor oil and using rectal suppositories;
- a large amount of fatty components with impaired patency of the lymphatic ducts.
Disorders of digestion, absorption and constant loss of fats lead to a decrease in serum levels of all lipid components, primarily cholesterol and fatty acids.
Diseases of the small intestine (ulcerative colitis, Crohn's disease, enteritis), liver pathologies (hepatitis, cystic fibrosis, cholecystitis), cholestasis, dyskinesia of the gallbladder and biliary tract, pancreatic insufficiency, chronic alcoholic pancreatitis, cardiospasm. The appearance of fatty acids in the feces is characteristic of celiac disease, pancreatogenic malabsorption syndrome, biliary dysfunction, enterokinase deficiency, excessive colonization of the bacterial microflora of the small intestine, conditions after resection of the small intestine. The mechanisms responsible for the digestion of fats can be affected by taking certain medications. The syndrome of accelerated evacuation of intestinal contents can be observed after excessive use of laxatives, anti-obesity drugs.
Features of steatorrhea in children
The presence of fat in the feces in a child is most often the result of a lack of pancreatic enzymes and the immaturity of the enzyme system.
Enzymes involved in the lipid metabolism of the newborn begin to be produced in sufficient quantities only by three months, which leads to inadequate digestion of fats. Also, steatorrhea in infants can be caused by defective liver function due to genetic disorders that can be structural and metabolic in nature. In weakened infants, metabolism is restored only by 4-5 months of age.
With proper therapy, the signs of steatorrhea in infants can be smoothed out until they disappear completely.
Classification of steatorrhea
There are several types of steatorrhea:
- food (alimentary) - is the result of nutritional characteristics and manifests itself in the case of excessive consumption of fat-containing foods that the body cannot assimilate in full;
- intestinal - occurs with damage to the mucous membrane of the small intestine and impaired absorption of fats. In this case, fats are not absorbed in the small intestine and are excreted in the feces;
- pancreatic - diagnosed with dysfunction of the pancreas and lipase deficiency.
In addition, steatorrhea is classified according to the type of bowel movement:
- feces contain neutral fats;
- fatty acids and soaps are found in feces;
- mixed form: fats, fatty acids and soaps are present in feces.
Symptoms of steatorrhea
Long-term excretion of fats from the body along with feces affects the state of all systems and organs.
The main symptoms are an increased urge to defecate, diarrhea with profuse loose stools. Constant diarrhea leads to dehydration of the body, with all its inherent symptoms (dry skin, constant thirst, etc.). The feces have an oily consistency, are distinguished by a greasy sheen, it is difficult to wash off with water. These symptoms are joined by nausea, heartburn, belching, bloating and rumbling in the intestines, dry cough. Less commonly, there is soreness in the upper abdomen.

Steatorrhea accompanied by diarrhea, frequent bowel movements, dyspepsia
In the absence of timely adequate therapy for the disease that caused steatorrhea, disorders of the cardiovascular, endocrine, genitourinary and nervous systems can develop, which is due to a secondary violation of protein metabolism. A decrease in protein content occurs for several reasons: abdominal digestion and protein absorption are disrupted. Also, with malabsorption, the permeability of the intestinal barrier often increases and protein excretion occurs with its loss through the intestine.
Moderate loss of protein occurs with malabsorption of any genesis. In this case, the patient complains of general weakness, decreased performance. Disorders of protein metabolism leads to a progressive decrease in body weight, a decrease in the amount of total protein and albumin, ascites, hypoproteinemic (protein-free) edema.
Also, steatorrhea is accompanied by vitamin deficiency. The development of hypovitaminosis is explained by impaired absorption in the intestine, as well as the property of a number of vitamins to be absorbed only in the presence of fats. The severe course of malabsorption is accompanied by a violation of the metabolism of almost all vitamins, but clinically pronounced hypovitaminosis appears rather late. The deficiency of vitamins of group B is manifested earlier than others. The absorption of fat-soluble vitamins - A, D, E, K is significantly impaired. These vitamins normally have the same mechanisms of absorption as triglycerides. Their assimilation changes with an inferiority of the bile micelle (chronic biliary insufficiency, dysbiosis), an increase in hydrostatic pressure in the intestinal lymphatic system (Whipple's disease), and metabolic disorders of enterocytes.
Hypovitaminosis can have the following manifestations:
- dizziness;
- soreness of the spine and joints;
- convulsive conditions;
- swelling;
- dryness and pallor of the mucous membranes;
- itchy skin;
- decreased visual acuity;
- dull and brittle hair, flaking nails;
- glossitis, stomatitis (including angular), looseness and bleeding of the gums.
Absorption of fat-soluble vitamins occurs mainly in the small intestine, therefore, in pathological conditions accompanied by atrophy of the mucous membrane of the small intestine, the process of their assimilation is disrupted. At the same time, the presence of pancreatic lipase for the absorption of this group of vitamins is not required, therefore, with pancreatic insufficiency, there is usually no vitamin deficiency.
Despite the absence of specific symptoms of hypovitaminosis, it should be borne in mind that vitamin E is one of the most powerful antioxidants, vitamin D regulates the absorption of calcium in the intestine, and vitamin K is a factor in blood coagulation, so even their latent deficiency must be corrected.
Diagnostics
The examination begins with the collection of complaints. On palpation, there is a rumbling and splashing on the left side of the abdomen, you can feel the transfusion of the mass that is in the intestine. After the examination, the doctor prescribes a number of laboratory (feces, blood, urine tests) and instrumental (ultrasound, colonoscopy, MRI) studies.
Fecal lipidogram
An important stage in the diagnosis is a laboratory study of feces, in which fecal masses are checked for the presence of fatty acids, neutral fat, soap - the so-called fecal lipid profile. This analysis is prescribed to assess the functions and identify pathologies of the digestive tract and pancreas. A fecal lipidogram is indicated if the following diseases are suspected:
- pancreatitis;
- benign or malignant tumors of the gastrointestinal tract;
- intestinal tuberculosis;
- malabsorption syndrome;
- cholelithiasis;
- violation of the secretory function of the pancreas (for example, insufficient lipase activity);
- violation of lymph outflow with damage to the mesenteric lymph nodes;
- increased peristalsis of the small intestine.
Compliance with the rules of preparation and collection technique affects the reliability of the lipid profile result. It is forbidden to collect material for research earlier than 2 days after X-ray examination of the digestive tract using contrast. Three days before collection of feces, it is recommended to exclude drugs that affect peristalsis, composition and color of feces.
The stool intended for the test should be formed naturally, no enema or laxatives should be used. On the eve of the test, it is necessary to exclude from the diet foods that contribute to the staining of feces, excessive gas formation in the intestines, the occurrence of diarrhea or constipation.
Before collecting the material, it is recommended to empty the bladder, wash the external genitals with clean water, and pat dry with a towel. For hygiene procedures, it is better to use soap without foaming additives or fragrances.
Feces are collected in a plastic container with a special spatula built into the lid. In advance, you need to take care of the container from which the feces will be collected for analysis. It can be a dry and clean vessel, or you can also attach plastic wrap to the surface of the toilet bowl. After defecation, about 20–25 ml of feces are collected in a prepared dish. It is allowed to store the material in the refrigerator at a temperature of +3 to +7 ° C during the day. It is important not to forget to sign the container before submitting it for analysis.
There are several methods of analysis, the qualitative test is usually performed microscopically, and the quantitative test is performed by chromatography.
In a qualitative test, a stool sample is stained with Sudan dye and examined under a microscope to assess the presence of fatty acids, soaps, and neutral fat drops, which have a bright orange-red color.
Quantitative detection of lipid levels is performed on an automatic analyzer by chromatography. During the study, fat is extracted with a mixture of chloroform and ethanol. The extracts are subjected to chromatography on a silica gel layer in the ether-acetone system (85:15). After staining with a solution of phosphoric-molybdic acid, all lipids contained in the test sample are detected. The fecal lipidogram will be performed within one or two working days.
The norms of fecal lipid profile are indicated in the table.
| Index | Norm |
| General lipids | 606–672 mg / dL |
| Unesterified fatty acids | 17.1-20.5% |
| Monoglycerides | Absent |
| Diglycerides | 3.7-4.7% |
| Triglycerides | 10.2-13.3% |
| Phospholipids | 13.7-15.3% |
| Cholesterol | 33.2-35% |
| Coprosterol | Absent |
| Coprostanone | 18-20.9% |
Treatment
Treatment of steatorrhea consists in eliminating the causes of insufficient absorption of fatty acids by the body, as well as correcting impaired metabolism. Drug therapy includes taking medications, the action of which is aimed at eliminating the consequences of steatorrhea: enzyme preparations with an increased content of lipases, antacids to neutralize stomach acid, cortisone, hydrochloric acid, vitamin complexes containing vitamins gr. B, ascorbic and niacin, fat-soluble vitamins A, D, E and K.

An important condition for the treatment of steatorrhea is diet.
The therapy also provides for the correction of the diet and diet. A fractional meal with a three-hour interval between meals is recommended, the weight of one portion should not exceed 200 g, and the daily volume of consumed fats should be 50–65 g. Fatty, fried and spicy foods, alcohol, and sugary drinks should be excluded from the diet. Reduce carbohydrate intake. Preference should be given to dishes from lean meats, low-fat fish, dairy products, low-fat cottage cheese, fresh vegetables.
YouTube video related to the article:

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.