- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Fat embolism
The content of the article:
- Causes and risk factors
- Forms of pathology
- Symptoms
- Diagnostics
- Treatment
- Possible complications and consequences
- Forecast
- Prevention
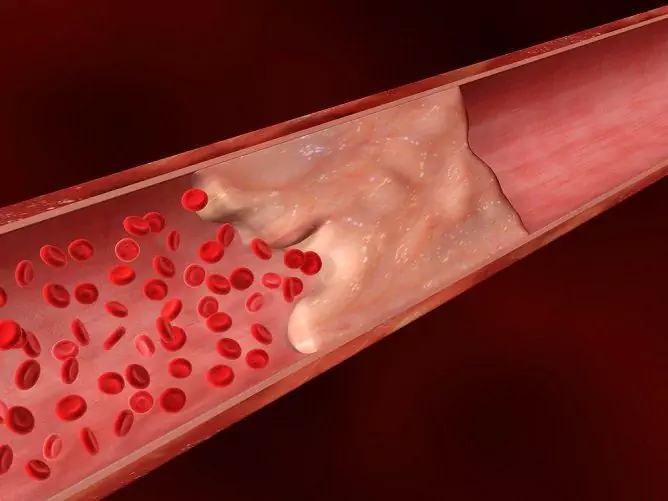
Fat embolism is a pathology in which blood vessels are clogged with droplets of fat, which leads to impaired blood flow.

Source: spy-bubble.org
Fat embolism is considered as a systemic inflammatory reaction that develops under the influence of mechanical and biochemical processes: from the site of damage to the bone marrow or subcutaneous tissue, fatty particles enter the bloodstream and cause the development of a local inflammatory reaction at the site of deposition. In addition, the release of fat globules into the bloodstream entails a slowdown in blood flow, a change in the rheological properties of blood, and a violation of microcirculation.
Large fat particles are able to pass through the capillaries of the lungs and stay in them. Small fat droplets penetrate into the systemic circulation to the target organs (brain, heart, skin and retina, less often the kidneys, spleen, liver, adrenal glands), causing a clinical picture of fat embolism.

Source: healthandsymptoms.com
Causes and risk factors
Most often, fat embolism occurs as a complication of skeletal injuries (fractures of the pelvic bones, lower leg, femur, damage to adipose tissue) or surgical interventions (extensive surgical interventions on tubular bones, joint replacement, hip osteosynthesis, reposition of fragments, maxillofacial surgery, liposuction) …
The occurrence of a fatty embolism is also possible with the following pathologies:
- sepsis;
- tumors;
- diabetes;
- osteomyelitis;
- severe burns;
- acute pancreatitis, pancreatonecrosis in severe form;
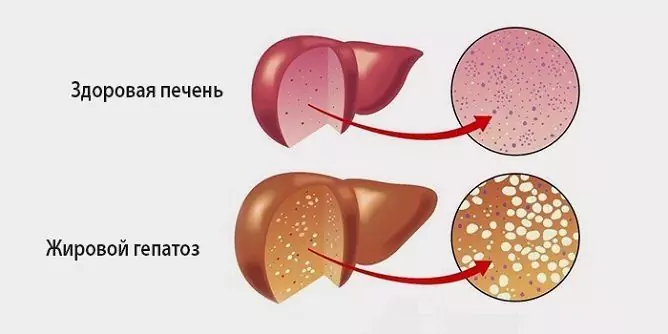
- toxic and fatty degeneration of the liver;
- long-term corticosteroid therapy;
- postresuscitation states;
- sickle cell anemia;
- bone marrow biopsy;
- erroneous intravenous administration of liposoluble drugs;
- shock states.
Risk factors: a large amount of blood loss and a prolonged period of hypotension, incorrect immobilization and transportation of the patient.

Source: okardio.com
Forms of pathology
Depending on the rate of development of manifestations, the duration of the latent period, the following forms of fat embolism are distinguished:
- acute - develops within a few hours after injury, one of the severe options is lightning-fast, in which massive damage to the musculoskeletal system leads to the rapid flow of a large number of fat globules into the vascular bed and lungs (fat embolism in fractures); this form is fatal in a few minutes;
- subacute - the clinical picture develops within 12-72 hours; may develop 2 weeks or more after injury.
According to the localization of the lesion, fat embolism is divided into pulmonary, cerebral and mixed (fatty embolism of the lungs, brain, liver, less often other organs).
Depending on the causes, fat embolism is classified as occurring during or after surgery, as a result of amputation, trauma, exposure to certain drugs.

Source: cf.ppt-online.org
Symptoms
The clinical picture of fatty embolism does not have clearly defined symptoms and manifests itself in a variety of symptoms that only make it possible to suspect it. Symptoms include non-specific manifestations: pulmonary, neurologic, and cutaneous.
On the first day, the pathology may be asymptomatic. The clinical picture is often superimposed on the picture of traumatic shock or traumatic brain injury. The first symptoms of fat embolism in fractures and injuries are usually pulmonary and respiratory disorders:
- feeling of tightness in the chest, lack of air, chest pain;
- pleural pain;
- dyspnea;
- signs of acute respiratory distress syndrome (hyperthermia, tachycardia, tachyarrhythmia, fever, cyanosis, etc.);
- dyspnea;
- oliguria;
- cough, wheezing, hemoptysis.
In the early stages, cerebral symptoms appear. As a result of cerebral embolism and hypoxic damage, the following neurological symptoms develop:
- motor restlessness;
- irritability or lethargy;
- convulsive syndrome (both local and generalized convulsions);
- disturbances of consciousness: disorientation, delirium, stupor, coma;
- focal neurological symptoms (impaired ability to speak or understand speech, paralysis, impaired complex movements, anisocoria, visual impairment).
In most patients, petechial rashes are found on the skin. The appearance of petechiae is based on capillary blockage by fatty emboli and damage to them by released fatty acids. Petechiae are localized in the upper half of the body, in the axillary region. They usually disappear within a day.
When examining the fundus, signs of retinal damage are found:
- exudate;
- hemorrhages (subconjunctival petechiae);
- plaques, spots;
- intravascular fat globules.
Diagnostics
When making a diagnosis, a set of diagnostic criteria for fat embolism is used, the presence of axillary or subconjunctival petechial rashes, and dysfunctions of the central nervous system are revealed. The state of consciousness is assessed on the Glasgow Coma Scale. There are signs of pulmonary edema and hypoxemia (a decrease in the oxygen content in the blood).
During the diagnosis of fat embolism, laboratory data are taken into account:
- decrease in hemoglobin;
- increased ESR;
- a decrease in the number of platelets;
- decrease in fibrinogen levels;
- decreased hematocrit (the volume of red blood cells in the blood);
- presence of drops of neutral fat in urine measuring 6 microns, fat globules in blood plasma, sputum, cerebrospinal fluid;
- the presence of fat on skin biopsy in the area of petechiae.
Instrumental studies are more informative. Chest X-ray can be used to assess changes resulting from a fatty pulmonary embolism. On the roentgenogram, the appearance of small focal shadows and an increase in the pulmonary pattern are noted: manifestations of diffuse lung infiltration, characteristic of the development of ARDS.

Source: cf.ppt-online.org
EKG allows to identify unmotivated persistent tachycardia, cardiac arrhythmias, which indicate an overload of the right half of the heart or myocardial ischemia.
In the course of computed tomography of the brain, cerebral edema, the presence of petechial hemorrhages, foci of necrosis, and perivascular infarctions are determined. Magnetic resonance imaging visualizes diffuse hyperechoic areas, revealing the etiology of cerebral embolism. Fundoscopy reveals the presence of fatty angiopathy in the fundus retina. Monitoring using pulse oximetry, control of intracranial pressure is also used.
Treatment
Treatment of fatty embolism consists in stopping the main clinical manifestations of the injury or disease that caused it. The main directions of therapy:
- provision of oxygen delivery to tissues, oxygen therapy and respiratory support;
- infusion therapy of systemic microcirculation disorders, eliminating spasm of peripheral vessels, replenishment of circulating blood volume, rheological, transfusion therapy by introducing biological fluids, correction of water-electrolyte balance using colloidal and crystalloid solutions. The introduction of albumin is shown, which is able to restore the volume of circulating blood, bind free fatty acids and reduce the degree of damage to lung functions;
- with high intracranial pressure - dehydration therapy using osmotic diuretics;
- therapy of brain hypoxia using antihypoxants, barbiturates and opiates;
- metabolic therapy - course administration of nootropic drugs;
- sedation therapy;
- correction of the coagulation and fibrinolysis system using anticoagulants, in particular, heparin, which, along with anticoagulant properties, has the ability to activate lipoproteins and accelerate the enzymatic reaction of triglyceride hydrolysis, helping to cleanse the lungs from fat globules;
- intensive hormone therapy, the use of corticosteroids - provide protection against free oxygen radicals and enzymes;
- the use of drugs, the action of which is aimed at reducing the concentration of fat globules in the blood, restoring the physiological dissolution of de-emulsified fat and for the prevention of de-emulsification (Lipostabil, Essentiale);
- detoxification and detoxification therapy - forced diuresis, exchange plasmapheresis. Plasmapheresis operations normalize the rheological properties of blood, its electrolyte, morphological, biochemical composition and hemodynamic parameters;
- surgical treatment, timely operative stabilization of fractures (transosseous wire osteosynthesis with wire rod devices, intramedullary osteosynthesis with a nail);
- correction of the immune status under the control of data from immunological studies.
Possible complications and consequences
Possible consequences of fat embolism include the development of pneumonia, respiratory failure, acute pulmonary failure, renal failure, ischemic stroke.
Forecast
3-13% of all cases of fatty embolism are fatal. However, the unfavorable prognosis lies in the fact that fat embolism occurs against the background of severe conditions, early diagnosis and adequate therapy of fat embolism improves the prognosis.
Prevention
Prevention of fat embolism includes: prevention of injury in high-risk patients, timely and correct immobilization of the limb in case of injury, early surgical stabilization of fractures of the pelvis and tubular bones, stabilization of bone fragments, adherence to the technique of infusion therapy.
YouTube video related to the article:

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!