- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Pulmonary embolism
The content of the article:
- Causes and risk factors
- Forms of the disease
- Pulmonary embolism symptoms
- Diagnostics
- Pulmonary embolism treatment
- Potential consequences and complications
- Forecast
- Prevention
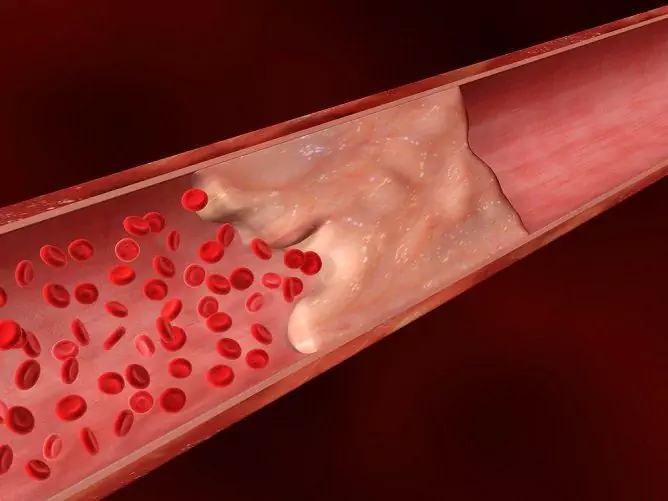
Pulmonary embolism (pulmonary embolism, pulmonary embolism, pulmonary embolism) is a mechanical obstruction (obstruction) of blood flow in the pulmonary artery basin caused by an embolus (thrombus) entering it, which is accompanied by severe spasm of the pulmonary artery branches, the development of acute pulmonary heart, and a decrease in cardiac output, bronchospasm and a decrease in blood oxygenation.
Of all autopsies carried out annually in Russia, pulmonary embolism is found in 4-15% of cases. According to statistics, 3% of surgical interventions in the postoperative period are complicated by the development of PE, and death is observed in 5.5% of cases.
Pulmonary embolism occurs predominantly in people over 40.

Source: okeydoc.ru
Causes and risk factors
In 90% of cases, the source of blood clots leading to pulmonary embolism is located in the inferior vena cava basin (ilio-femoral segment, veins of the small pelvis and prostate gland, deep veins of the leg).
Risk factors are:
- malignant neoplasms (usually cancer of the lungs, stomach and pancreas);
- diseases of the cardiovascular system (myocardial infarction, atrial fibrillation, mitral valve disease, myocarditis, infective endocarditis);
- heart failure;
- stroke;
- sepsis;
- inflammatory bowel disease;
- erythremia;
- nephrotic syndrome;
- obesity;
- hypodynamia;
- estrogen therapy;
- primary hypercoagulability syndrome;
- antiphospholipid syndrome;
- lack of proteins C and S;
- lack of antithrombin III;
- pregnancy and the postpartum period;
- dysfibrinogenemia;
- epilepsy;
- trauma;
- postoperative period.
Forms of the disease
Depending on the localization of the pathological process, the following types of pulmonary embolism are distinguished:
- embolism of small branches of the pulmonary artery;
- embolism of the lobar or segmental branches of the pulmonary artery;
- massive - the place of localization of the thrombus is the main trunk of the pulmonary artery or one of its main branches.
Four forms of pulmonary embolism are distinguished depending on the volume of the vessels excluded from the bloodstream:
- fatal (the volume of switched off pulmonary arterial blood flow over 75%) - leads to a rapid death;
- massive (the volume of the affected vessels is over 50%) - tachycardia, hypotension, loss of consciousness, acute right ventricular failure, pulmonary hypertension are noted, cardiogenic shock may develop;
- submaximal (30 to 50% of the pulmonary arteries are affected) - characterized by moderate shortness of breath, mild signs of acute right ventricular failure at normal blood pressure;
- small (less than 25% is disconnected from the bloodstream) - slight shortness of breath, there are no signs of failure of the right stomach.
In accordance with the clinical course, pulmonary embolism can take the following forms:
- Lightning (acute) - occurs when a thrombus is completely blocked by a thrombus of both main branches or the main trunk of the pulmonary artery. The patient suddenly develops and rapidly increases acute respiratory failure, blood pressure drops sharply, and ventricular fibrillation appears. A few minutes after the onset of the disease, death occurs.
- Acute - observed with occlusion of the main branches of the pulmonary artery, part of the segmental and lobar branches. The disease begins suddenly. In patients, cardiac, respiratory and cerebral insufficiency occurs and rapidly progresses. Lasts 3-5 days, in most cases is complicated by the formation of a lung infarction.
- Prolonged (subacute) - develops with occlusion of the middle and large branches of the pulmonary artery and is characterized by multiple pulmonary infarctions. The pathological process lasts several weeks. The severity of right ventricular and respiratory failure gradually increases. Repeated thromboembolism often occurs, which can be fatal.
- Recurrent (chronic) - characterized by repeated thrombosis of the lobar and segmental branches of the pulmonary artery, as a result of which the patient develops recurrent pulmonary infarctions, pleurisy, which are usually bilateral. Right ventricular failure and hypertension of the pulmonary circulation are gradually increasing. Recurrent pulmonary embolism usually occurs in the postoperative period, as well as in patients suffering from cardiovascular or oncological diseases.

Source: myshared.ru
Pulmonary embolism symptoms
The severity of the clinical picture depends on the following factors:
- the rate of development of impaired blood flow in the pulmonary artery system;
- the size and number of thrombosed arterial vessels;
- the severity of violations of the blood supply to the lung tissue;
- the initial state of the patient, the presence of concomitant pathology.
Pathology manifests itself in a wide clinical range from asymptomatic to sudden death. The clinical symptoms of pulmonary embolism are not specific; they are characteristic of many other diseases of the lungs and cardiovascular system. However, their sudden occurrence and the impossibility of explaining them by another pathology (pneumonia, myocardial infarction, cardiovascular insufficiency) makes it highly probable that the patient has a pulmonary embolism.

Source: uslide.ru
In the classic clinical picture of pulmonary embolism, several syndromes are distinguished.
- Pulmonary pleural. Its signs are shortness of breath (caused by impaired ventilation and perfusion of the lungs) and cough, which in 20% of patients is accompanied by hemoptysis, pain in the chest area (usually in its posterior regions). With massive embolism, pronounced cyanosis of the upper half of the body, neck and face develops.
- Cardiac. Characterized by a feeling of discomfort and pain behind the sternum, tachycardia, heart rhythm disturbances, severe arterial hypotension up to the development of a collaptoid state.
- Abdominal. It occurs somewhat less frequently than other syndromes. Patients complain of pain in the upper abdomen, the occurrence of which is associated with stretching of the glisson capsule against the background of right ventricular failure or irritation of the dome of the diaphragm. Other symptoms of abdominal syndrome are vomiting, belching, intestinal paresis.
- Cerebral. More often observed in elderly people suffering from severe atherosclerosis of the arteries of the brain. It is characterized by loss of consciousness, convulsions, hemiparesis, psychomotor agitation.
- Renal. After removing patients from shock, they may develop secretory anuria.
- Feverish. Against the background of inflammatory processes in the pleura and lungs, patients' body temperature rises to febrile values. The duration of the fever is 2 to 15 days.
- Immunological. It develops in the second or third week from the onset of the disease and is characterized by the appearance of circulating immune complexes in the blood of patients, the development of eosinophilia, recurrent pleurisy, pulmonitis, and the appearance of a urticarial rash on the skin.
Diagnostics
If a pulmonary embolism is suspected, a complex of laboratory and instrumental examination is prescribed, including:
- chest x-ray - signs of pulmonary embolism are: atelectasis, plethora of the roots of the lungs, amputation symptom (sudden breakage of the vessel), Westermark symptom (local decrease in pulmonary vascularization);
- ventilation-perfusion lung scintigraphy - signs of a high probability of pulmonary embolism are: normal ventilation and decreased perfusion in one or several segments (the diagnostic value of the method decreases with previous episodes of pulmonary embolism, lung tumors and chronic obstructive pulmonary disease);
- angiopulmonography is a classic method for diagnosing pulmonary embolism; the criteria for making a diagnosis are the detection of a thrombus contour and a sudden break of a branch of the pulmonary artery;
- electrocardiography (ECG) - allows you to identify indirect signs of pulmonary embolism and exclude myocardial infarction.

Source: stopvarikoz.net
Differential diagnosis is carried out with non-thrombotic pulmonary embolism (tumor, septic, fatty, amniotic), psychogenic hyperventilation, fractured ribs, pneumonia, bronchial asthma, pneumothorax, pericarditis, heart failure, myocardial infarction.
Pulmonary embolism treatment
Patients with pulmonary embolism require urgent hospitalization in the intensive care unit. At the first stage, medical treatment of pulmonary embolism consists in the administration of heparin, indirect anticoagulants and fibrinolytic agents.
With severe arterial hypotension, infusion therapy is performed, dopamine, Dobutamine, Adrenaline hydrochloride are used. In case of a recurrent clinical course of pulmonary embolism, indirect anticoagulants, acetylsalicylic acid (Aspirin) are prescribed for a long period or for life, a cavafilter is installed, which prevents blood clots from entering the inferior vena cava.
The development of infarction pneumonia is an indication for the appointment of broad-spectrum antibiotics.
With massive pulmonary embolism and ineffectiveness of the conservative therapy, surgical intervention is performed in one of two ways:
- closed embolectomy with a suction catheter;
- open embolectomy in conditions of artificial circulation.
Surgical treatment of pulmonary embolism is accompanied by a rather high risk of complications and death.

Source: cf.ppt-online.org
Potential consequences and complications
Acute massive pulmonary embolism can cause sudden death. In those cases when compensatory mechanisms have time to work, the patient does not die immediately, but his secondary hemodynamic disorders rapidly increase, which, in the absence of timely treatment, lead to death. Possible consequences of a pulmonary embolism can be:
- acute cor pulmonale;
- pneumonia;
- pleurisy;
- lung abscess;
- gangrene of the lung.
Forecast
With timely and adequate treatment of pulmonary embolism, the mortality rate does not exceed 10%, without treatment it reaches 30%. The prognosis is worse in people with previous heart or lung disease.
Chronic pulmonary hypertension develops in about 1% of patients who underwent pulmonary embolism in the long-term period.
Prevention
In order to prevent pulmonary embolism, the preoperative preparation of patients with risk factors includes:
- pneumatic compression;
- wearing compression underwear (elastic stockings);
- small doses of heparin.
In the postoperative period, small doses of heparin are injected subcutaneously, and indirect anticoagulants are prescribed.
With a recurrent course of pulmonary embolism, indirect anticoagulants are prescribed for life, deciding whether to install a cavafilter.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!