- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
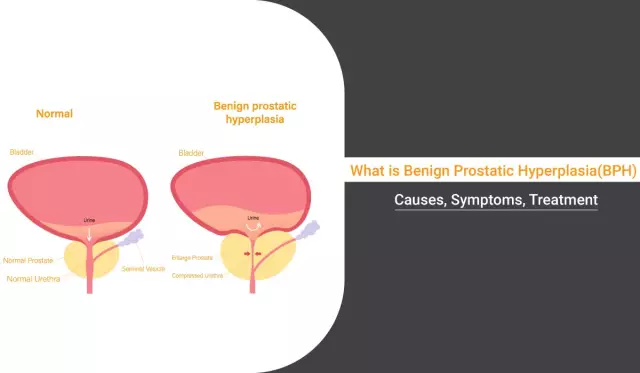
Hyperplasia of the prostate
The content of the article:
- Causes and risk factors
- Forms of the disease
- Disease stages
- Symptoms of prostatic hyperplasia
- Diagnostics
- Treatment of prostatic hyperplasia
- Possible complications and consequences
- Forecast
- Prevention
Hyperplasia of the prostate gland (prostate adenoma) is a common urological disease in which the cellular elements of the prostate proliferate, which causes compression of the urethra and, as a result, urination disorders. The neoplasm develops from the stromal component or from the glandular epithelium.

Source: radikal.ru
Most often, the disease is diagnosed at the age of 40-50. According to statistics, up to 25% of men over 50 years old have symptoms of prostatic hyperplasia, at 65 years old, the disease is found in 50% of males, and at an older age - in about 85% of men.
The prostate gland (prostate) is an unpaired androgen-dependent tubular-alveolar gland of external secretion, which is located under the bladder, the initial part of the urethra passes through it - the prostate gland circularly covers the neck of the urethra and its proximal section. The excretory ducts of the gland open into the urethra. The prostate comes in contact with the pelvic diaphragm, the ampulla of the rectum.
Prostate function is controlled by androgens, estrogens, steroid hormones, and pituitary hormones. The secretion produced by the prostate is released during ejaculation, taking part in the liquefaction of semen.
The prostate gland is formed by the glandular tissue itself, as well as muscle and connective tissue. The process of hyperplasia, that is, pathological growth, usually begins in the transient zone of the prostate gland, after which polycentric growth of nodes occurs, followed by an increase in the volume and mass of the gland. An increase in tumor size leads to a displacement of the prostate tissue outward, growth is possible both in the direction of the rectum and in the direction of the bladder
Normally, the prostate gland does not interfere with the process of urination and the functioning of the urethra as a whole, since, although it is located around the posterior urethra, it does not squeeze it. With the development of prostatic hyperplasia, the prostatic urethra is compressed, its lumen narrows, making it difficult for urine to flow.
Causes and risk factors
One of the main causes of prostatic hyperplasia is hereditary predisposition. The likelihood of the disease increases significantly in the presence of close relatives suffering from prostatic hyperplasia.
In addition, risk factors include:
- changes in hormonal levels (primarily a violation of the balance between androgens and estrogens);
- metabolic disorders;
- infectious and inflammatory processes of the urogenital tract;
- advanced age;
- lack of physical activity, especially a sedentary lifestyle, which contributes to congestion in the small pelvis;
- hypothermia;
- bad habits;
- inappropriate nutrition (high content of fatty and meat foods in the diet with an insufficient amount of plant fibers);
- exposure to adverse environmental factors.
Forms of the disease
Depending on the direction of growth, prostatic hyperplasia is divided into:
- subbubble (the neoplasm grows towards the rectum);
- intravesical (the tumor grows towards the bladder);
- retrotrigonal (the neoplasm is localized under the bladder triangle);
- multifocal.
On the morphological basis, prostatic hyperplasia is classified into glandular, fibrous, myomatous and mixed.
Disease stages
In the clinical picture of prostatic hyperplasia, depending on the state of the organs and structures of the urogenital tract, the following stages are distinguished:
- Compensation. It is characterized by compensated hypertrophy of the bladder detrusor, which ensures complete evacuation of urine, there are no disorders of the kidneys and urinary tract.
- Subcompensation. The presence of dystrophic changes in the detrusor, signs of residual urine, dysuric syndrome, decreased renal function.
- Decompensation. Disorder of the detrusor function of the bladder, the presence of uremia, aggravation of renal failure, involuntary excretion of urine.
Symptoms of prostatic hyperplasia
The disease develops gradually. The severity of symptoms of prostatic hyperplasia depends on the stage.
The main signs of an early stage of the tumor process are frequent urination, nocturia. The prostate gland is enlarged, its borders are clearly delineated, the consistency is densely elastic, the stream of urine during urination is normal or somewhat sluggish. Palpation of the prostate is painless, the median groove is well palpated. The bladder is emptied completely. The duration of this stage is 1-3 years.
At the stage of subcompensation, compression by the neoplasm of the urethra is more pronounced, the presence of residual urine, thickening of the bladder walls are characteristic. Patients complain of a feeling of incomplete emptying of the bladder after urinating, sometimes of the involuntary discharge of a small amount of urine (leakage). Signs of chronic renal failure may appear. Urine when urinating is excreted in small portions, it can be cloudy and contain an admixture of blood. Stones can form in the bladder due to stagnation.
At the decompensated stage of the disease, the volume of excreted urine is insignificant, urine can be excreted dropwise, it is cloudy, with an admixture of blood (rusty color). The bladder is distended with large amounts of residual urine.
Symptoms of prostatic hyperplasia in the later stages include weight loss, a feeling of dry mouth, the smell of ammonia in the exhaled air, loss of appetite, anemia, and constipation.
Diagnostics
Diagnosis of prostatic hyperplasia is based on the collection of complaints and anamnesis (including family), examination of the patient, as well as a number of instrumental and laboratory tests.
During the urological examination, the condition of the external genital organs is assessed. Finger examination allows to determine the condition of the prostate gland: its contour, soreness, the presence of a groove between the lobes of the prostate gland (normally present), areas of compaction.
General and biochemical blood tests are prescribed (the content of electrolytes, urea, creatinine is determined), a general urine test (the presence of leukocytes, erythrocytes, protein, microorganisms, glucose). Determine the concentration of prostate-specific antigen (PSA) in the blood, the content of which increases with prostatic hyperplasia. It may be necessary to conduct a bacteriological culture of urine in order to exclude an infectious pathology.
The main instrumental methods are:
- transrectal ultrasound (determination of the size of the prostate gland, bladder, the degree of hydronephrosis, if any);
- urofluometry (determination of the volumetric rate of urination);
- survey and excretory urography; and etc.
If necessary, differential diagnosis with bladder cancer or urolithiasis, cystoscopy is used. This method is also indicated in the presence of a history of sexually transmitted diseases, prolonged catheterization, trauma.
Treatment of prostatic hyperplasia
The main goals of treatment of prostatic hyperplasia are elimination of urinary disorders and prevention of further development of the disease, which causes severe complications from the bladder and kidneys.
In some cases, they are limited to dynamic monitoring of the patient. Dynamic observation implies regular examinations (with an interval of six months to a year) by a doctor without any therapy. Expectant tactics is justified in the absence of pronounced clinical manifestations of the disease with the absence of absolute indications for surgical intervention.
Indications for drug therapy:
- the presence of signs of the disease that give the patient anxiety and reduce the quality of his life;
- the presence of risk factors for the progression of the pathological process;
- preparation of the patient for surgery (in order to reduce the risk of postoperative complications).
As part of drug therapy for prostatic hyperplasia, the following can be prescribed:
- selective α 1 -adrenergic blockers (effective in the presence of acute urinary retention, including postoperative genesis, in which it is impossible to empty the overflowing bladder for 6-10 hours after surgery; improve cardiac activity with concomitant ischemic heart disease);
- 5-alpha-reductase inhibitors (reduce the size of the prostate gland, eliminate gross hematuria);
- preparations based on herbal extracts (reducing the severity of symptoms).
In the case of acute urinary retention, a patient with prostatic hyperplasia is shown hospitalization with bladder catheterization.
Androgen replacement therapy is performed in the presence of laboratory and clinical signs of age-related androgen deficiency.
The absolute indications for surgical treatment of prostatic hyperplasia are:
- relapses of acute urinary retention after removal of the catheter;
- lack of a positive effect from conservative therapy;
- the formation of a diverticulum or large bladder stones;
- chronic infectious processes of the urogenital tract.
Surgical intervention for prostatic hyperplasia is of two types:
- adenomectomy - excision of hyperplastic tissue;
- prostatectomy - resection of the prostate gland.
The operation can be performed using traditional or minimally invasive methods.
Transvesical adenomectomy with access through the bladder wall is usually used in the case of intratrigonal neoplasm growth. This method is somewhat traumatic compared to minimally invasive interventions, but with a high degree of probability it provides a complete cure.
Transurethral resection of the prostate is characterized by high efficiency and low trauma. This endoscopic method assumes that there is no need to dissect healthy tissues when approaching the affected area, makes it possible to achieve reliable control of hemostasis, and can also be performed in elderly and senile patients with concomitant pathology.
Transurethral needle ablation of the prostate gland consists in the introduction of needle electrodes into the hyperplastic tissue of the prostate gland, followed by the destruction of pathological tissues using radio frequency exposure.
Transurethral vaporization of the prostate is carried out using a roller electrode (electrovaporisation) or a laser (laser vaporisation). The method consists in evaporation of hyperplastic prostate tissue with its simultaneous drying and coagulation. Also, for the treatment of prostatic hyperplasia, the method of cryodestruction (liquid nitrogen treatment) can be used.
Embolization of the arteries of the prostate belongs to endovascular operations and consists in the clogging of the arteries supplying the prostate gland with medical polymers, which leads to its reduction. The operation is performed under local anesthesia by access through the femoral artery.
Endoscopic holmium laser enucleation of prostatic hyperplasia is performed using a holmium laser with a power of 60-100 W. During the operation, the hyperplastic prostate tissue is excreted into the bladder cavity, after which the adenomatous nodes are to be removed by means of an endomorcellator. The effectiveness of this method approaches that of open adenomectomy. The advantages are a lower likelihood of complications in comparison with other methods and a shorter rehabilitation period.
The patient is advised to adhere to a diet with the exception of spicy, spicy, fatty foods, and alcoholic beverages.
Possible complications and consequences
Against the background of prostatic hyperplasia, serious pathologies of the urinary tract can develop: urolithiasis, pyelonephritis, cystitis, urethritis, chronic and acute renal failure, bladder diverticula. In addition, orchiepididymitis, prostatitis, bleeding from the prostate gland, and erectile dysfunction can be a consequence of advanced hyperplasia. There have been suggestions of possible malignancy (i.e., degeneration into cancer), but they have not been proven.
Forecast
With timely, correctly selected treatment, the prognosis is favorable.
Prevention
In order to reduce the risk of developing prostatic hyperplasia, it is recommended:
- upon reaching 40 years of age - annual preventive examinations by a urologist;
- timely seeking medical help at the first signs of a urinary disorder;
- rejection of bad habits;
- avoiding hypothermia;
- balanced diet;
- regular sex life with a regular partner;
- sufficient physical activity.
YouTube video related to the article:

Anna Aksenova Medical journalist About the author
Education: 2004-2007 "First Kiev Medical College" specialty "Laboratory Diagnostics".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!