- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Fatty hepatosis
The content of the article:
- Causes and risk factors
- Forms of the disease
- Symptoms of fatty hepatosis
- Diagnostics
- Treatment of fatty hepatosis
- Potential consequences and complications
- Forecast
- Prevention
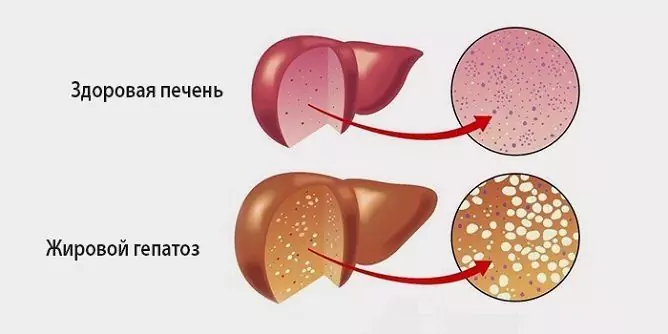
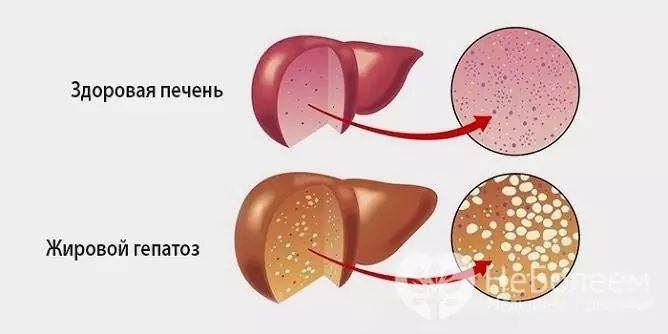
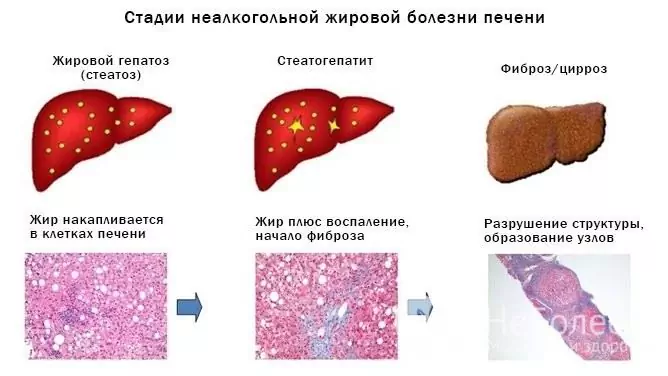
Fatty hepatosis is a pathological process characterized by fatty degeneration of hepatocytes and the accumulation of fat droplets both inside the cells themselves and in the intercellular substance.
Fatty hepatosis occurs in almost 100% of patients with alcoholic liver disease and in about 30% of patients with non-alcoholic lesions. In fact, this pathology is the initial stage of alcoholic liver disease, which later ends in cirrhosis, chronic liver failure, and then death. Women are more susceptible to the disease - according to statistics, among the total number of patients, their share is 70%.
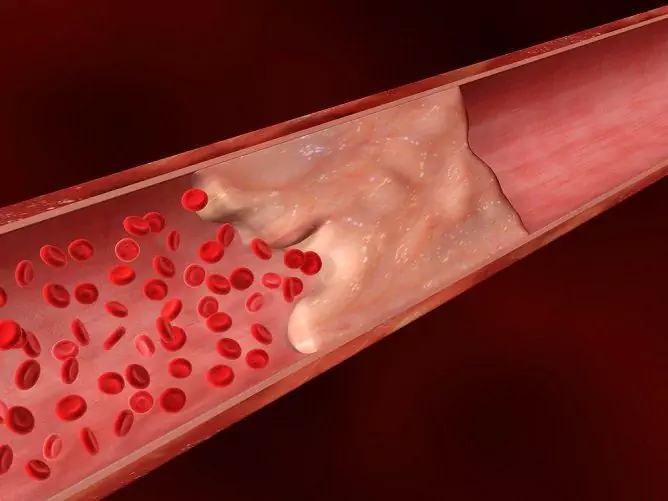
Fatty hepatosis is an urgent medical and social problem. It significantly increases the risk of developing cirrhosis, metabolic and endocrine disorders, diseases of the cardiovascular system, varicose veins, allergic pathologies, which, in turn, significantly limit the ability of patients to work and cause disability.
Source: bolitpechen.ru
Causes and risk factors
In most cases, the development of fatty liver hepatosis is caused by damage to hepatocytes by alcohol and its metabolites. There is a direct relationship between the duration of the patient's consumption of alcoholic beverages and the severity of fatty degeneration of hepatocytes, an increased risk of cirrhosis.
Often, fatty hepatosis develops against the background of diabetes mellitus. Hyperglycemia and insulin resistance increase the concentration of fatty acids in the blood, which enhances the synthesis of triglycerides by hepatocytes. As a result, fat is deposited in the liver tissue.
Another reason for the development of fatty liver hepatosis is general obesity. A significantly increased body weight is not only accompanied by an increase in the percentage of adipose tissue in the patient's body, but also the development of metabolic syndrome with tissue resistance to insulin. The results of proton spectroscopy show that there is a direct relationship between fasting serum insulin concentration and the amount of fatty deposits in the liver.
Many other diseases occurring with metabolic disorders can also provoke fatty hepatosis:
- tumors;
- chronic pulmonary failure;
- chronic heart failure;
- cardiac ischemia;
- arterial hypertension;
- Wilson-Konovalov disease (congenital disorder of copper metabolism, other names: hepatolenticular degeneration, hepatocerebral dystrophy);
- Itsenko-Cushing's syndrome;
- thyrotoxicosis;
- myxedema;
- chronic diseases of the digestive system, accompanied by a violation of the absorption process.
Fatty hepatosis can be triggered by improper diet - a high content of simple carbohydrates, hydrogenated fats in the diet, the so-called Western diet (the predominance of refined foods in the diet, lack of coarse fiber), as well as a sedentary lifestyle.
Signs of fatty hepatosis are often present in people with a hereditary deficiency of enzymes involved in the process of lipid metabolism.
Thus, the primary cause of fatty hepatosis in many cases is insulin resistance, while fatty degeneration of hepatocytes becomes one of the links in the formation of the metabolic syndrome.
Other factors contributing to the accumulation of fat in the cells and intercellular substance of the liver are:
- hyperlipidemia;
- violation of the utilization of fats in the process of peroxidation;
- violation of the synthesis of apoprotein - an enzyme involved in the formation of transport forms of fats and their removal from cells.
Usually, not one specific factor leads to the development of fatty liver hepatosis, but their combination, for example, alcohol consumption while taking medications or improper diet.
Forms of the disease
Depending on the etiological factor, fatty hepatosis is subdivided into non-alcoholic steatohepatitis and alcoholic fatty liver disease. On liver biopsy, non-alcoholic steatohepatitis is diagnosed in about 7% of cases. Alcoholic fatty degeneration is detected much more often.
Fatty hepatosis is of two types:
- primary - associated with endogenous (internal) metabolic disorders (hyperlipidemia, diabetes mellitus, obesity);
- secondary - due to external (exogenous) influences leading to metabolic disorders (intake of corticosteroids, tetracycline, methotrexate, non-steroidal anti-inflammatory drugs, synthetic estrogens, Wilson-Konovalov disease, fasting, long-term parenteral nutrition, intestinal resection, gastroplasty, ileastoplasty).
Depending on the characteristics of fat deposition, fatty hepatosis is divided into the following forms:
- focal disseminated - usually occurs without any clinical manifestations;
- pronounced disseminated;
- zonal - fat is deposited in various zones of the liver lobe;
- microvesicular steatosis (diffuse).
Symptoms of fatty hepatosis
There are no specific clinical signs of fatty hepatosis even with significant morphological changes in the liver. Many patients have obesity and / or type II diabetes.
Signs of fatty hepatosis are nonspecific. These include:
- mild pain in the right upper quadrant of the abdomen, aching in nature;
- feeling of slight discomfort in the abdominal cavity;
- slight enlargement of the liver;
- asthenization;
- dyspeptic syndrome (nausea, sometimes vomiting, stool instability).
With severe fatty hepatosis, an icteric staining of the skin and mucous membranes may develop. Fatty degeneration of hepatocytes is accompanied by the release of a tumor-necrotizing factor, which leads to fainting, decreased blood pressure, increased bleeding (tendency to hemorrhages).
Diagnostics
Diagnosis of fatty liver hepatosis presents significant difficulties, since the disease is asymptomatic in most cases. Biochemical analyzes do not reveal significant changes. In some cases, there is a slight increase in the activity of serum transaminases. During the examination, it should be borne in mind that their normal activity does not exclude fatty hepatosis. Therefore, the diagnosis of this condition is based mainly on the exclusion of other liver pathologies.
To identify the cause that led to the occurrence of fatty hepatosis, the following laboratory tests are prescribed:
- determination of markers of autoimmune hepatitis;
- detection of antibodies to hepatitis viruses, rubella, Epstein - Barr, cytomegalovirus;
- study of hormonal status;
- determination of glucose concentration in blood serum;
- determination of the level of insulin in the blood.
Ultrasound examination can detect fatty steatosis only with significant fat deposition in the liver tissue. Magnetic resonance imaging is more informative. With a focal form of pathology, a radionucleide scan of the liver is shown.
The C13-metacetin breath test allows assessing the detoxification functions of the liver and the number of normally functioning hepatocytes.
To make the final diagnosis, a puncture biopsy of the liver is performed, followed by a histological analysis of the resulting biopsy. The histological signs of fatty hepatosis are:
- fatty degeneration;
- steatonecrosis;
- fibrosis;
- intralobular inflammation.
Treatment of fatty hepatosis
Therapy for patients with fatty hepatosis is performed by a gastroenterologist on an outpatient basis. Hospitalization is indicated only with significant fatty degeneration of the liver tissue, accompanied by a pronounced violation of its functions, primarily detoxification.
Diet for fatty hepatosis plays an important, sometimes paramount role in complex therapy. The diet is limited to fat, especially of animal origin. Protein consumption should be 100-110 g per day. The body must be supplied with minerals and vitamins in sufficient quantities.
Be sure to correct the increased body weight, which allows you to reduce, and in some cases, completely eliminate insulin resistance, as a result of which lipid and carbohydrate metabolism is normalized. Patients with fatty hepatosis should lose no more than 400-600 g per week - at a faster rate of weight loss, fatty hepatosis begins to progress rapidly and can lead to the formation of calculi in the biliary tract, liver failure. Ursodeoxycholic acid preparations may be prescribed to reduce the risk of stone formation.
To eliminate fatty liver infiltration, lithotropic drugs are used (essential phospholipids, lipoic acid, B vitamins, folic acid).
If necessary, in order to eliminate insulin resistance, patients are prescribed biguanides and thiazolidinediones.
Exercise helps improve the utilization of fatty acids.
With severe fatty hepatosis, the question of the advisability of lipid-lowering therapy with statins is decided. This method has not found widespread use, as statins themselves can cause damage to liver cells.
In order to restore impaired liver functions, hepatoprotectors (taurine, betaine, ursodeoxycholic acid, vitamin E) are used. In the medical literature there is information about the possibility of using angiotensin and pentoxifylline receptor blockers in fatty hepatosis.
In case of alcoholic fatty hepatosis, the main condition for successful treatment is a complete refusal to further use any alcoholic beverages. If necessary, the patient is referred for a consultation with a narcologist.
Potential consequences and complications
In the absence of the necessary therapy, fatty hepatosis increases the risk of developing the following diseases;
- varicose veins;
- cholelithiasis;
- metabolic disorders;
- cirrhosis of the liver.
Forecast
The outlook is generally favorable. In most cases, elimination of the etiological factor allows not only to prevent further progression of the disease, but also to achieve restoration of liver tissue. The ability to work is usually not impaired. Patients for a long time must carefully follow the recommendations of the attending physician (refusal of alcoholic beverages, diet, maintaining an active lifestyle).
If the causative factors are not eliminated, then fatty hepatosis will slowly progress, causing degenerative and inflammatory changes in the liver tissue, ultimately causing liver cirrhosis and the development of chronic liver failure.
Source: gastroe.ru
Prevention
Prevention of fatty hepatosis includes the following areas:
- active lifestyle;
- balanced diet;
- refusal to use alcoholic beverages;
- maintaining a normal body weight;
- timely detection of metabolic diseases, organs of the digestive system and their active treatment.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!