- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Laser correction after keratotomy
A large part of the population has been experiencing problems with vision since ancient times. The situation is aggravated with the development of technical progress, the improvement of computer technology, lengthening daylight hours due to electrical appliances and an increase in the load on the organ of vision and the entire nervous system as a whole.
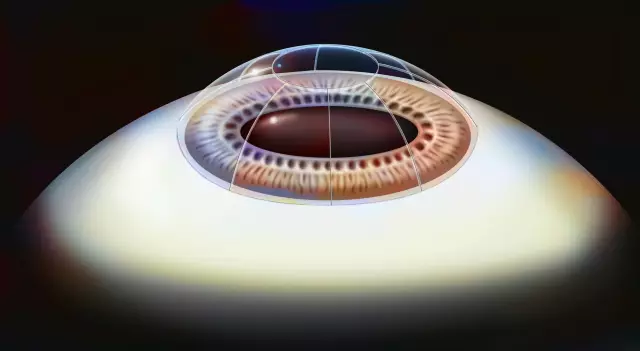
In the 80s, the task of improving vision was solved through keratotomy. The essence of the operation is the application of circular incisions to the cornea of the eye using diamond blades in certain areas. At that time, this made it possible to correct abnormalities in refraction in farsighted or nearsighted people, giving a chance for normal vision. During the healing process, the curvature of the eye changed and correction took place.
However, the past attempt to correct the anomalies of the organ of vision did not always end successfully, leaving behind a number of complications and new problems with vision. To date, this technique is not used, its place was taken by more advanced technologies of laser eye microsurgery. But thousands of patients who at one time underwent keratotomy, to this day experience significant difficulties with vision. Naturally, they are interested in getting rid of the problem with a surgical method at minimal cost. Today, there is an alternative way to help such patients: it is laser correction after keratotomy.

A little about the history and the principle of laser action on the cornea
For the first time, the attention of scientists was attracted by the use of a laser beam in 1976 when engraving computer microchips. It has been crafted with true jewelry craftsmanship and precision. After the development of technologies and a series of tests, the first operation of this kind was carried out in 1985.
The laser effect on the cornea is completely different from that of keratotomy. Instead of mechanical incisions of the cornea, high-tech methods are used here, which allow predicting the final result of the intervention with the utmost accuracy. The laser acts directly on the cornea, changing its curvature by evaporation (photochemical ablation) of the desired tissue layers from its surface. The result is precise focusing of the rays directly onto the retina.
The advantages of laser technology:
- high accuracy;
- safety and efficiency;
- low invasiveness;
- simplicity and availability;
- short duration of the procedure;
- minimal pain sensation;
- favorable result and negligible percentage of complications.
Modern computer installations clearly define the ideal corneal profile in this particular case, correcting almost any refractive error. For example, if it is necessary to normalize vision in case of myopia, tissues "evaporate" in the central part. In this case, the cornea changes its curvature and becomes flatter. To eliminate hyperopia, tissues are removed at the periphery, which leads to its more convex forms. Correction of astigmatism is a slightly more complex process, in which individual areas located in different meridians are subject to evaporation.
Contraindications to the operation and possible complications
Like any operation, laser correction has certain limitations. The possibility of this operation is decided in persons with myopia up to -15.0 D, as well as farsightedness up to +4.0 D, astigmatism up to ± 3.0 D. The issue of laser correction in patients with a thin cornea and a single eye is resolved separately. …
The following diseases are significant contraindications:
- severe immunodeficiencies of various etiologies;
- collagenoses;
- systemic and autoimmune diseases;
- organic brain damage with mental disorders;
- glaucoma, cataracts, retinal detachment;
- rough corneal scars;
- viral pathology.
In order to minimize the risk of complications, you should carefully diagnose, choose a progressive clinic with professional doctors who have experience in this area. It is of great importance that the surgeon is aware of your concomitant and chronic diseases, which can also cause complications. Naturally, you should strictly follow the doctor's recommendations during the recovery period.
What recommendations should be followed
The doctor will recommend using special eye gels and antibiotic drops. In case of pain, you can use pain relievers. It is allowed to lead an active lifestyle, doing dosed loads and even gentle sports (in accordance with the doctor's recommendations). You can not rub your eyes, allow touching the cornea. The next day, you can wash gently. Do not use makeup.
Efficiency and forecast
The overwhelming majority of operations are effective and result in 100% vision restoration. If this cannot be achieved, then you will be notified of this even before the operation. Vision is restored within 7-14 days. Complications in microsurgical practice are rare and range from 0.5 to 1.5% of cases.
Found a mistake in the text? Select it and press Ctrl + Enter.