- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Desarterization of hemorrhoids: reviews, the essence of the operation, pre- and postoperative period
The content of the article:
- Desarterization of hemorrhoids - what is it
- Training
- Operation progress
- Postoperative period
- Consequences of dearterization of internal hemorrhoids
- Advantages and disadvantages of the method
- Video
Desarterization of hemorrhoids is one of the minimally invasive interventions to avoid large-scale invasive surgery. As a rule, in the later stages of hemorrhoids, surgical intervention is required. Often, patients do not want to agree to it, the very prospect of such a complex procedure scares them. But the means of modern medicine and proctology can solve the problem with minimal tissue damage.
Desarterization of hemorrhoids - what is it
The term "dearterization of hemorrhoids" means the surgical suturing of the vessels that supply blood to the hemorrhoids. The essence of the method is to reduce arterial inflow, and as a result - venous congestion in the hemorrhoidal plexus. When the arteries are sutured, the veins no longer fill up, blood flow is normalized. At the same time, the blood supply to the rectum is not disturbed - the manipulation has a high selectivity, the doctor locates the desired artery with high precision and stitches it. Vessels providing mucosal trophism remain intact. After about a week, the nodes begin to dry out, their independent rejection.

HAL RAR method provides complete cure for hemorrhoids in 90% of cases
The procedure includes plastic manipulations, so external traces of surgery are invisible. Desarterization is characterized by a rapid period of convalescence (recovery) - complete normalization of blood circulation occurs two weeks after surgery.
The operation was developed in 1995 and since then has noticeably improved both in hardware and in terms of the execution method. Now specialists adhere to the HAL RAR technology. This abbreviation stands for hemorrhoidal artery ligation with recto anal repair. The concept includes not only suturing the arteries with a special ligature, but also the subsequent transanal mucopexy - suturing the hanging mucous membrane and pulling it up with subsequent fixation.
If earlier it was believed that dearterization is effective only at the 2nd and occasionally 3rd stages of the disease, then thanks to the updated methodology, patients with the 3rd and 4th stages are also subject to treatment. The method allows you to get rid of the disease in one operation, and the patient's stay in the hospital is usually not required.
Training
In the preoperative period, the patient undergoes a mandatory examination in the form of an ECG, a blood test, an overview x-ray or contrast angiography is possible. Before manipulation, it is forbidden to take drugs that affect blood clotting.
The day before the intervention, the patient's diet is limited to light broths. No food is consumed on the day of surgery. Be sure to defecate with laxatives or a cleansing enema.
Operation progress
The stages of surgical intervention are as follows:
- The anesthesiologist paints the patient. Both spinal anesthesia and intravenous anesthesia can be used.
- The surgeon carries out the obligatory processing of the operating field.
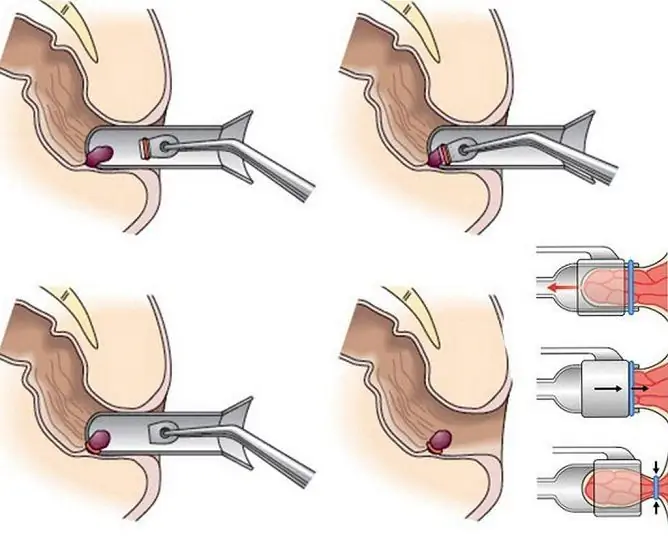
- A modified anoscope combined with a Doppler probe is inserted into the anus. This small device captures the slightest pulsation of the hemorrhoidal arteries and displays it in several imaging modes. Now the surgeon can detect the bearing vessels accurately.
- The anoscope tip has a hole for a needle. A needle with a ligature is inserted there, with the help of which the arteries are ligated, starting from the superior rectal artery. On average, this step takes from 30 minutes to an hour, depending on the number of vessels to be ligated.
- After that, the doctor examines the rectal mucosa for the presence of sagging epithelium, prolapses and various kinds of defects that may appear after the hemorrhoids collapse. He performs mucopexy by suturing the overhanging mucous membrane to the walls. Additionally, lifting of the mucous membrane can be performed - pulling it up with the straightening of the folds that appeared after mucopexy. This concludes the operational manipulations.
Postoperative period
Now the patient goes into the postoperative period. For several hours he is under the supervision of doctors. This is necessary to monitor the condition for possible complications - seam divergence, bleeding. The patient receives recommendations from the doctor on the further way of life, antibiotic therapy and a gentle diet are prescribed.
Despite the fact that transanal dearterization of hemorrhoids refers to surgical procedures of the 3rd degree of complexity, the effectiveness of such treatment even in patients with the 3rd and 4th stages of hemorrhoids reaches 90%, and for patients with early treatment it is almost absolute.
Consequences of dearterization of internal hemorrhoids
After the operation, the patient can return home on the same day, but he should adhere to the recommendations, especially carefully those related to diet. It is not recommended to eat non-mechanically processed and coarse food, as well as spicy. Alcohol is excluded from the diet. You should drink up to three liters of water in total with all daily meals. For two weeks after the intervention, it is prohibited:
- physical activity (running, lifting weights, sex). Minimum activity should be maintained in the form of moderate exercise to improve circulation in the lower half of the body, leisurely walks are also recommended;
- thermal procedures - sauna, hot bath, bath, since there is a strong vasodilation, which can cause bleeding and damage to the wound surface;
- manipulations in the area of surgery - do not put enemas or rectal suppositories. If you have any discomfort, you should consult your doctor.
The patient should listen to his own well-being and take a responsible attitude to the recovery period. He should monitor the state of feces - its color, consistency. This is to prevent rectal bleeding. If the stool is hard during the diet, your doctor may prescribe mild laxatives.
At the end of the period of convalescence and spontaneous rejection of dry hemorrhoids, another examination can be carried out, after which no restrictions on lifestyle and activities are imposed.
Advantages and disadvantages of the method
Positive reviews about the dearterization of hemorrhoids note the painlessness of the operation, its speed, the absence of large-scale cavity intervention, and a quick return to normal life. Also, positive evidence in favor of the operation are:
- successful treatment of even advanced stages of hemorrhoids;
- scarless healing - a known disadvantage of invasive methods is the characteristic stenosis (narrowing) of the rectum due to the postoperative scar. It can turn into intestinal obstruction. HAL RAR does not have this disadvantage;
- minimal likelihood of relapse;
- efficiency indicator - about 90%;
- the ability to choose the method of pain relief;
- outpatient procedure, carried out without hospitalization;
- together with hemorrhoids, the surgeon simultaneously, in the course of one operation, treats anal fissures and fistulas of the rectum.
Desarterization is contraindicated in patients with ischemic heart disease, heart failure, severe arterial hypertension. However, if necessary, these conditions can almost always be stopped with medication.
You cannot perform surgery during pregnancy and breastfeeding. Clinical contraindications for surgery are:
- thrombosis of hemorrhoids;
- paraproctitis;
- purulent fistulas of the rectum.
The disadvantage of this method is its relatively high cost. Not every clinic performs such an operation, since expensive equipment is needed. In addition, a small number of surgeons have sufficient qualifications and skills to perform operations of the 3rd degree of complexity.
Video
We offer for viewing a video on the topic of the article.

Nikita Gaidukov About the author
Education: 4th year student of the Faculty of Medicine No. 1, specializing in General Medicine, Vinnitsa National Medical University. N. I. Pirogov.
Work experience: Nurse of the cardiology department of the Tyachiv Regional Hospital No. 1, geneticist / molecular biologist in the Polymerase Chain Reaction Laboratory at VNMU named after N. I. Pirogov.
Found a mistake in the text? Select it and press Ctrl + Enter.