- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Diabetic polyneuropathy
The content of the article:
- Causes and risk factors
- Forms of the disease
- Disease stages
- Symptoms of Diabetic Polyneuropathy
- Diagnostics
- Treatment
- Possible complications and consequences
- Forecast
Diabetic polyneuropathy is a condition that is a complication of diabetes mellitus and is characterized by progressive degeneration of peripheral sensory and motor nerve fibers. The disease is chronic in nature, its manifestations slowly increase over many years, the rate of development depends on the adequacy of diabetes treatment and maintenance of normal blood sugar levels. Nerve pathology is one of the factors in the formation of neurocirculatory disorders in diabetes mellitus - diabetic foot, trophic ulcers, etc.

Source: cf.ppt-online.org
Causes and risk factors
The immediate cause of diabetic polyneuropathy is a persistent increase in blood sugar levels that occurs in diabetes mellitus due to decreased insulin production. At the same time, the mechanism of damage to nerve fibers in this condition is multifactorial and is due to several pathological processes. Several factors play a leading role.
- Metabolic disorders in the nervous tissue. Lack of insulin leads to the fact that glucose from the blood does not enter the cells, which is manifested by hyperglycemia. At the same time, this carbohydrate is the main and practically the only source of energy for the nervous tissue. Lack of energy leads to fiber degeneration and the development of diabetic polyneuropathy.
- General metabolic disorders. Due to the lack of glucose in the tissues, bypass metabolic pathways are turned on to replenish the energy deficit. This leads to the formation of ketone bodies (a breakdown product of fats) and other toxic substances that can damage the nervous tissue.
- Ischemic disorders. Diabetes mellitus is characterized by the development of angiopathies (vascular lesions) associated with pathological processes in the vascular wall. This reduces the blood supply to tissues and organs, especially at the microcirculatory level. Insufficient blood circulation aggravates the phenomenon of energy deficiency in nerve fibers and accelerates their degeneration.

Source: myshared.ru
The likelihood of developing diabetic polyneuropathy is higher in patients with diabetes mellitus, who often violate their diet and take hypoglycemic drugs. In some cases, peripheral nerve disorders may be the first sign of insufficient insulin production, but more often neuropathy occurs many years after the development of diabetes. Pathological changes in the nervous system are irreversible.
Forms of the disease
Diabetic polyneuropathy is characterized by a variety of clinical forms, depending on which group of nerves is most affected. There is a certain discussion about classification in the scientific community.
According to some researchers, only one of the forms of damage to the nervous system in diabetes mellitus - distal symmetric sensorimotor neuropathy should be considered a true diabetic polyneuropathy. From this point of view, the condition has the following variants of the clinical course:
- violation of vibration sensitivity and individual tendon reflexes (for example, Achilles). This is a mild form, for many years it proceeds without noticeable progression;
- damage to individual nerves, becoming acute or subacute. Most often affects the nerve trunks of the limbs (ulnar, femoral, median nerves) and the head (facial, trigeminal, oculomotor);
- inflammation and degeneration of the nerves of the lower extremities, affecting the autonomic innervation. It is characterized by significant pain and is often complicated by trophic ulcers of the feet and legs, gangrene.
Another point of view is that all types of peripheral nerve damage in diabetes mellitus are referred to as diabetic polyneuropathy. In this case, symmetric sensorimotor neuropathy and autonomic neuropathy are distinguished in it. The latter includes pupillary, gastrointestinal, perspiration, cardiovascular forms - depending on which system or organ is most affected by the pathology. Separately, diabetic neuropathic cachexia is distinguished - a severe syndrome that includes both sensorimotor and autonomic neuropathy, combined with a significant decrease in body weight.
Disease stages
There are currently no clearly defined criteria for the clinical stages of diabetic polyneuropathy. However, the pathology has a pronounced progressive character, the rate of increase in symptoms depends on the degree of hyperglycemia, the type of neuropathy, and the patient's lifestyle. In general, the course of the disease can be divided into stages:
- Nonspecific neurogenic manifestations. These include disturbances in sensitivity, a feeling of "goose bumps" on the skin, in some cases - soreness along the nerve trunks and in the area of their innervation. This condition can persist for many years and not turn into more severe forms.
- Movement disorders. They arise when motor fibers are involved in the pathological process, including the autonomic nervous system. Muscle twitching, paresis, and, extremely rarely, convulsions may develop. When the nerves of the autonomic nervous system are affected, there are disturbances in accommodation, pupillary reflexes, sweating, and the work of the cardiovascular and digestive systems.
- Trophic disorders. The most severe consequences of diabetic polyneuropathy develop as a result of a combination of pathology of autonomic innervation and microcirculatory disorders. They can be both local (trophic ulcers, gangrene of the feet) and general (neuropathic cachexia).
Another common outcome of diabetic polyneuropathy is damage to the 3rd and 4th pairs of cranial nerves responsible for the movement of the eyeballs. This is accompanied by a significant deterioration in vision due to a violation of the processes of accommodation, convergence, pupillary reflexes, the development of anisocoria and strabismus. Most often, this picture develops in patients with diabetes mellitus over 50 years old, who have suffered from other manifestations of neuropathy for a long time.

Source: ytimg.com
Symptoms of Diabetic Polyneuropathy
Diabetic polyneuropathy is characterized by a significant variety of manifestations, the clinical picture depends on the form of the pathology, the degree of its progression, the type of nerve fibers (motor, sensory, autonomic) that were affected more than others. Most often, the first to appear are violations of sensitivity (mainly temperature and vibration). Later, movement disorders (weakness of the muscles of the limbs, paresis) can join them. If the nerves of the eyeball were affected, anisocoria and strabismus occur.
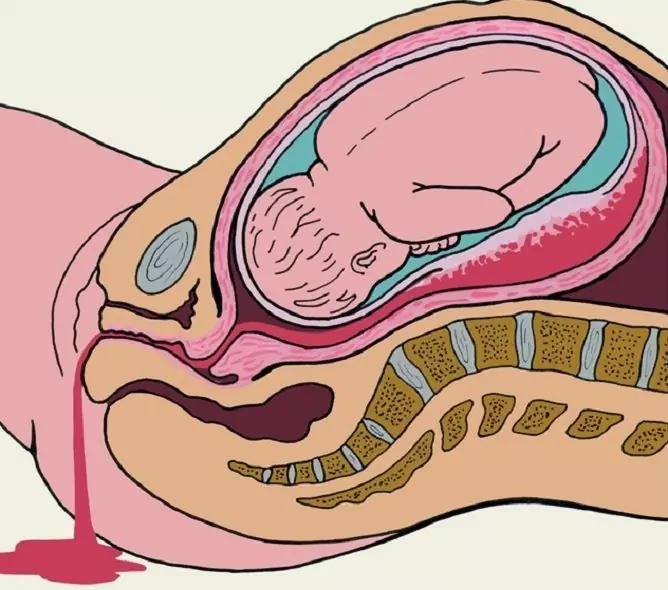
Diabetic polyneuropathy is almost always accompanied by vegetative-circulatory disorders, mainly in the lower extremities. Initially, the temperature of the skin of the feet and legs decreases, there may be violations from the skin - peeling, keratinization. Injuries and injuries to the legs take a long time to heal. As the pathology progresses, severe pains in the legs occur (both at rest and during exercise), trophic ulcers develop. Over time, necrosis of individual areas of the feet often develops, which then turn into gangrene.

Source: feedmed.ru
Diagnostics
In the diagnosis of diabetic polyneuropathy, a number of instrumental and laboratory techniques are used to study the functions of the peripheral nervous system, the state of muscles, and the skin. The choice of diagnostic technique depends on the form of the pathology and the severity of its symptoms. In addition, diagnostic measures should include methods for determining diabetes mellitus and the severity of hyperglycemia - blood and urine tests for glucose levels, glycosylated hemoglobin content and other studies. The definition of diabetic polyneuropathy directly includes:
- examination by a neurologist - study of complaints and subjective symptoms, study of the anamnesis of the underlying disease, determination of skin sensitivity, activity of tendon reflexes and other neurological functions;
- electromyography - allows you to assess the relationship between the nervous and muscular systems and thereby indirectly determine the degree of damage to nerve fibers;
- the study of nerve conduction (NPT) - studies the speed of passage of nerve impulses along the fibers to assess the degree of damage, often carried out in conjunction with electromyography.
Other medical specialists can also participate in the diagnosis of diabetic polyneuropathy - endocrinologist, ophthalmologist, urologist, gastroenterologist. This is necessary in cases where nerve damage leads to disruption of the work of certain organs and systems.
Treatment
The main principle of the treatment of diabetic polyneuropathy is to reduce the negative effect of hyperglycemia on the peripheral nervous system. This is achieved by a properly selected diet and hypoglycemic therapy, the rules of which the patient must strictly follow. With the development of nerve damage, pathological changes are usually irreversible, therefore it is important not to allow the progression of the condition.

In addition to treating the underlying disease, drugs are prescribed that improve trophism and metabolism in nerve tissues, enhancing microcirculation. For local action (for example, to improve the trophism of the tissues of the feet), you can use massages, electrophoresis and other physiotherapeutic procedures.
In the treatment of diabetic polyneuropathy, symptomatic measures are also used - for example, analgesics from the NSAID group are prescribed for pain and inflammation of the nerves. With the development of trophic ulcers, their careful processing is necessary to prevent infection. In severe cases (with extensive ulcers or gangrene), surgical treatment is necessary, up to amputation.
Possible complications and consequences
The progression of diabetic polyneuropathy can cause paresis and muscle weakness, which limits mobility. The defeat of the cranial nerves leads to paralysis of the facial muscles and visual disturbances. Vegetative and circulatory disorders accompanying polyneuropathy of the extremities are often complicated by trophic ulcers and gangrene, which is an indication for amputation of the legs.

The most severe complication of diabetic polyneuropathy is neuropathic cachexia, accompanied by weight loss, sensorimotor disorders, and numerous pathologies of internal organs.
Forecast
The prognosis is conditionally unfavorable, since the developed disorders are irreversible. However, timely detection of pathology in combination with the correct selected therapy can significantly slow down its progression.
YouTube video related to the article:

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!