- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Obstetric bleeding
The content of the article:
- Causes
- Kinds
- Stages
- Signs
- Diagnostics
- Treatment
- Prevention
- Consequences and complications
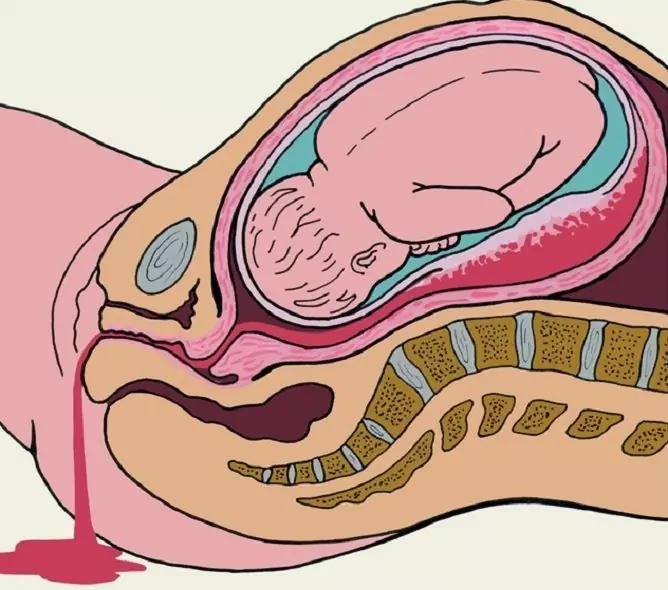
Obstetric refers to bleeding from the birth canal that occurs during pregnancy, childbirth and the early postpartum period. According to various sources, they are observed in 4-12% of all pregnancies.
Obstetric hemorrhages always pose a serious threat to a woman's life and health; they occupy the first place in the structure of maternal mortality.

Obstetric bleeding occurs during pregnancy, childbirth, or early postpartum
Causes
In the first trimester of pregnancy, bleeding can result from:
- cervical pregnancy;
- cystic drift;
- undeveloped pregnancy;
- spontaneous miscarriage;
- some pathologies of the cervix (cancer, polyps).
In the second half of pregnancy, the causes of obstetric bleeding are:
- premature placental abruption;
- placenta previa;
- rupture of the uterus.
Causes of obstetric bleeding that occur during labor:
- rupture of the cervix;
- rupture of the body of the uterus;
- premature placental abruption;
- partial true or dense attachment of the placenta;
- remnants of placental tissue in the uterine cavity;
- spasm of the pharynx with infringement of the placenta.

Multiple pregnancy is also a risk factor for the development of obstetric bleeding.
In the early postpartum period, the most common cause of obstetric bleeding is uterine hypotonia, that is, its insufficient contraction. Risk factors for the development of hypotonic uterine bleeding:
- burdened obstetric and gynecological history;
- gestosis;
- multiple pregnancy;
- polyhydramnios;
- large fruit.
Kinds
Depending on the cause, obstetric bleeding can be roughly divided into several types:
- Associated with insufficient uterine tone.
- Associated with disorders of blood coagulation.
- Associated with a delay in the uterine cavity of the embryo or placental tissues.
- Associated with traumatic injuries of the uterus and (or) birth canal.
Stages
According to the volume of lost blood, obstetric bleeding is of several stages:
- Acute blood loss.
- Syndrome of massive blood loss.
- Hemorrhagic shock.
Signs
The main symptom of obstetric bleeding is bleeding from the genital tract of a woman. For obstetric bleeding, a sudden and abrupt onset is characteristic, they quickly acquire a massive character, often combined with pain syndrome.
Against the background of blood loss in women, hemodynamic parameters worsen, circulatory and anemic hypoxia develops. This is manifested by the following signs:
- pallor of the skin;
- severe weakness;
- nausea;
- cold sweat;
- lowering blood pressure;
- tachycardia;
- dyspnea;
- decreased urine output.
As the amount of blood loss increases, the severity of symptoms increases. Consciousness is disturbed - up to its complete loss.

Obstetric bleeding usually begins suddenly, quickly becomes massive, and often leads to the development of coagulopathy
Obstetric bleeding often leads to the development of a coagulopathy of the type of disseminated intravascular coagulation (DIC), which is accompanied by massive bleeding that threatens the woman's life. The difference between coagulopathic bleeding from other types is that the blood flowing from the genital tract forms very loose clots or does not form them at all.
Diagnostics
Diagnosis of obstetric bleeding is aimed at finding out their cause, but emergency medical attention is required. Usually diagnostics is carried out according to the following algorithm:
- Taking anamnesis. The doctor specifies when the bleeding occurred, what preceded its appearance, what is the volume of blood loss before the start of the examination and the features of the course of pregnancy.
- Calling a laboratory assistant for blood sampling. The patient's blood group and Rh, hemoglobin level, blood coagulation time are urgently determined, a coagulogram is done.
- General examination, including measuring blood pressure, counting the pulse, respiratory rate.
- External gynecological examination. Examine the external genitalia, palpate the uterus through the anterior abdominal wall, assessing its size and the state of the tone of the myometrium.
- Inspection in mirrors. With the help of a vaginal speculum, the gynecologist examines the vagina and cervix for possible damage, as well as the presence of neoplasms of the cervical canal.
- Ultrasound of the uterus. During the study, the condition of the fetus and the location of the placenta are determined in pregnant women, and its possible premature detachment is revealed. In the postpartum period, ultrasound can detect a delay in the uterine cavity of the placental lobules or fetal membranes.
- Cardiotocography. The method allows you to assess the condition of the fetus.

In order to prevent and find out the cause of obstetric bleeding, a woman should be examined regularly
Treatment
The main task of the treatment of obstetric bleeding is to implement reliable hemostasis, save the life of the woman and, if possible, the fetus. A pregnant woman should be admitted to a hospital. She is provided with strict bed rest and close medical supervision.
Conservative therapy for obstetric bleeding that occurs at any stage of pregnancy and at any stage of labor is aimed at treating the underlying pathology that caused the bleeding. In addition, active correction of the consequences of massive blood loss is carried out.
If obstetric bleeding occurs during a premature pregnancy and, at the same time, according to objective studies, the condition of the fetus is not affected, therapy is aimed at both stopping bleeding and maintaining pregnancy. It includes the appointment:
- tocolytics;
- fortifying drugs;
- angioprotectors;
- agents affecting blood rheology;
- sedatives.
With massive blood loss caused by premature placental abruption, it may be necessary to transfuse whole blood, erythrocyte mass, and plasma.
If obstetric bleeding occurs in the last trimester of pregnancy or in the initial period of labor, in some cases, emergency caesarean section is used to stop it. The indications are:
- full placenta previa;
- premature placental abruption, accompanied by massive bleeding;
- cervical cancer;
- rupture of the body of the uterus.
To stop obstetric bleeding that occurs in the postpartum period, carry out:
- the introduction of uterine-reducing drugs (uterotonics);
- manual examination of the uterine cavity with the removal of the remaining placenta and fetal membranes;
- massage of the body of the uterus on the fist.
If it is not possible to stop bleeding with conservative methods, in order to save lives, women resort to removing the uterus.

For massive obstetric bleeding in late pregnancy, an emergency caesarean section is performed
With severe obstetric bleeding during pregnancy or childbirth, a caesarean section is first performed, after which a ligation of the uterine arteries is performed. If this does not lead to the proper clinical effect, amputation or extirpation of the uterus is performed.
Indications for the removal of the uterus in the postpartum period are:
- Couveler's uterus;
- inability to achieve hemostasis by conservative methods.
In the postpartum period, obstetric bleeding is often caused by trauma to the birth canal. In this case, the tears are sutured.
Prevention
Prevention of the occurrence of obstetric bleeding includes the following measures:
- examination and treatment of identified gynecological and somatic diseases in a woman at the stage of pregnancy planning;
- early registration of a pregnant woman;
- regular scheduled visits to a pregnant district obstetrician-gynecologist;
- timely diagnosis and treatment of any complications of pregnancy (threats of spontaneous interruption, placental insufficiency, gestosis, arterial hypertension);
- control of blood glucose levels;
- rational nutrition of a pregnant woman;
- regular exercise therapy;
- rational management of childbirth.
Consequences and complications
The prognosis for obstetric bleeding, especially massive, is always serious. The most common complications are:
- fetal hypoxia;
- intrauterine fetal death;
- development of Kuveler's uterus;
- development of disseminated intravascular coagulation syndrome;
- hemorrhagic shock;
- acute renal failure;
- Sheehan's syndrome;
- death of a woman.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!