- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Lymphadenopathy
The content of the article:
- Causes
- Kinds
- Signs of lymphadenopathy
- Diagnostics
- Lymphadenopathy treatment
- Prevention
Lymphadenopathy is a pathological condition characterized by enlarged lymph nodes and is one of the leading symptoms of many diseases.
Lymph nodes are the peripheral organs of the lymphatic system. They play the role of a kind of biological filter that cleans the lymph flowing into them from the limbs and internal organs. There are about 600 lymph nodes in the human body. However, only inguinal, axillary and submandibular lymph nodes can be palpated, that is, those that are located superficially.

Causes
Infectious diseases lead to the development of lymphadenopathy:
- bacterial [plague, tularemia, syphilis, benign lymphoreticulosis (cat scratch disease), pyogenic bacterial infections];
- fungal (coccidioidomycosis, histoplasmosis);
- mycobacterial (leprosy, tuberculosis);
- chlamydial (lymphogranuloma venereal);
- viral (HIV, hepatitis, measles, cytomegalovirus, Epstein-Barr virus);
- parasitic (filariasis, trypanosomiasis, toxoplasmosis).
The development of lymphadenopathy can lead to therapy with certain drugs, including cephalosporins, gold preparations, sulfonamides, Captopril, Atenolol, Allopurinol, Carbamazepine, Phenytoin, Penicillin, Hydralazine, Quinidine, Pyrimethamine.
The most common lymphadenopathy is observed against the background of the following diseases:
- lymphadenitis;
- Infectious mononucleosis;
- rubella;
- streptoderma;
- lymph node tuberculosis;
- non-Hodgkin lymphomas;
- lymphogranulomatosis (Hodgkin's disease);
- Gaucher disease;
- viral hepatitis;
- Still's disease;
- sarcoidosis;
- Waldenstrom's macroglobulinemia;
- Niemann-Pick disease;
- Lyme disease;
- tularemia;
- HIV infection;
- benign lymphoreticulosis.
Infections of the oropharynx often lead to cervical lymphadenopathy. Usually, this condition develops in children and adolescents against the background of childhood infectious diseases and is associated with the functional immaturity of the immune system, which does not always adequately respond to infectious stimuli. The highest risk of developing cervical lymphadenopathy in children who have not received timely vaccination against diphtheria, mumps, measles, rubella.
Axillary lymphadenopathy is caused by:
- purulent-inflammatory processes localized in the arms, shoulders or chest;
- some types of skin pathology (neurodermatitis, psoriasis);
- immunodeficiency states;
- diseases of the mammary glands (mastitis, mastopathy, cancer);
- autoimmune systemic diseases (systemic lupus erythematosus, rheumatoid arthritis, ankylosing spondylitis, systemic scleroderma).
Kinds
Depending on the number of lymph nodes involved in the pathological process, the following types of lymphadenopathy are distinguished:
- localized - an increase in one lymph node;
- regional - an increase in several lymph nodes located in one or two adjacent anatomical areas, for example, axillary lymphadenopathy;
- generalized - enlarged lymph nodes are localized in several non-adjacent anatomical areas, for example, inguinal and cervical adenopathy.
Localized lymphadenopathies are much more common (in 75% of cases) than regional or generalized ones. In about 1% of patients with persistent lymphadenopathy, medical examination reveals malignant neoplasms.
Depending on the etiological factor, lymphadenopathy is:
- primary - caused by primary tumor lesions of the lymph nodes;
- secondary - infectious, drug, metastatic (secondary tumor process).
In turn, infectious lymphadenopathy is subdivided into specific (caused by tuberculosis, syphilis and other specific infections) and non-specific.
According to the duration of the clinical course, acute and chronic lymphadenopathy is distinguished.
Signs of lymphadenopathy
With cervical, inguinal or axillary lymphadenopathy, an increase in lymph nodes is observed in the corresponding area, from insignificant to noticeable with the naked eye (from a small pea to a goose egg). Their palpation can be painful. In some cases, reddening of the skin is noted over the enlarged lymph nodes.

It is impossible to detect lymphadenopathy of the visceral nodes (mesenteral, perebronchial, lymph nodes of the hepatic hilum) visually or by palpation, it is determined only during the instrumental examination of the patient.
In addition to an increase in lymph nodes, there are a number of signs that may accompany the development of lymphadenopathy:
- unexplained loss of body weight;
- increased body temperature;
- excessive sweating, especially at night;
- enlargement of the liver and spleen;
- recurrent upper respiratory tract infections (tonsillitis, pharyngitis).
Diagnostics
Since lymphadenopathy is not an independent pathology, but just a symptom of intoxication in many diseases, its diagnosis is aimed at identifying the causes that led to an increase in lymph nodes. The examination begins with a thorough history taking, which in many cases allows a preliminary diagnosis to be made:
- eating raw meat - toxoplasmosis;
- contact with cats - toxoplasmosis, cat scratch disease;
- recent blood transfusions - hepatitis B, cytomegalovirus;
- contact with patients with tuberculosis - tuberculous lymphadenitis;
- intravenous drug administration - hepatitis B, endocarditis, HIV infection;
- casual sex - hepatitis B, cytomegalovirus, herpes, syphilis, HIV infection;
- work in a slaughterhouse or livestock farm - erysipeloid;
- fishing, hunting - tularemia.
With localized or regional lymphadenopathy, an examination of the area from which lymph flows through the affected lymph nodes is carried out for the presence of tumors, skin lesions, and inflammatory diseases. Other groups of lymph nodes are also examined in order to identify possible generalized lymphadenopathy.
With localized lymphadenopathy, the anatomical localization of enlarged lymph nodes can significantly narrow the number of suspected pathologies. For example, sexually transmitted infections usually lead to the development of inguinal lymphadenopathy, and cat scratch disease is accompanied by axillary or cervical lymphadenopathy.
Swollen lymph nodes in the right supraclavicular region are often associated with a malignant process in the esophagus, lungs, mediastinum. Left supraclavicular lymphadenopathy signals possible damage to the gallbladder, stomach, prostate, pancreas, kidneys, ovaries, seminal vesicles. A pathological process in the abdominal or pelvic cavity can lead to an increase in paraumbilical lymph nodes.
Clinical examination of patients with generalized lymphadenopathy should be directed towards the search for systemic disease. A valuable diagnostic finding is the detection of inflammation of the joints, mucous membranes, splenomegaly, hepatomegaly, and various types of rash.

In order to identify the cause that led to lymphadenopathy, according to indications, various types of laboratory and instrumental studies are performed. The scheme of a standard survey usually includes:
- general and biochemical blood test;
- general urine analysis;
- chest x-ray;
- Ultrasound of the abdominal and pelvic organs;
- computed and magnetic resonance imaging.
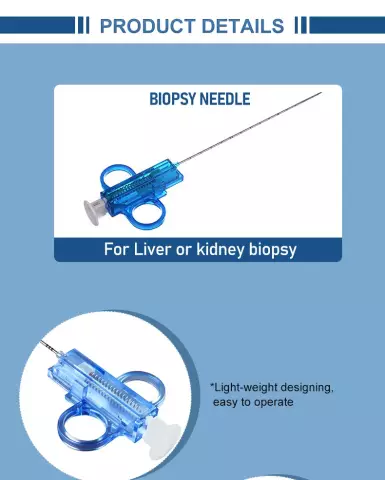
If necessary, a biopsy of the enlarged lymph node can be performed, followed by histological and cytological examination of the tissue samples obtained.
Lymphadenopathy treatment
Treatment of lymphadenopathy is to eliminate the underlying disease. So, if the enlargement of the lymph nodes is associated with a bacterial infection, a course of antibiotic therapy is indicated, the treatment of lymphadenopathy of tuberculous etiology is carried out according to a special DOTS + scheme, the treatment of lymphadenopathy caused by oncological disease consists of antitumor therapy.
Prevention
Prevention of lymphadenopathy is aimed at preventing diseases and intoxications that can provoke an increase in lymph nodes.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!