- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Clinical analysis of urine in a child: deciphering indicators, norm and deviations
The content of the article:
-
Organoleptic analysis
- Volume
- Colour
- Smell
- Frothiness
- Transparency
-
Physico-chemical analysis
Specific gravity
-
Biochemical analysis
- Protein
- Glucose
- Bilirubin
- Ketone bodies
-
Microscopy
- Erythrocytes
- Leukocytes
- Cylinders
- Slime
- Bacteria
- Amylase
- Salt
- Urine collection rules
Deciphering the analysis of urine in a child is carried out by the specialist who appointed the study. This allows you to avoid misinterpretation of the results and timely identify possible pathologies.
Urine (urine) is a physiological fluid produced by the kidneys. The main function of urine is to remove waste products from the body (toxins, dead cells, hormones and other metabolites). The formation and excretion of urine is of great importance for maintaining the water-salt balance in the body.

It is recommended that children take a general urine test regularly, even if they are healthy.
Clinical (general) urine analysis - study of the physicochemical properties of urine and sediment microscopy. The main indications for passing a urine test:
- symptoms of kidney and genitourinary system diseases;
- preventive examination;
- general assessment of the patient's condition;
- dynamic assessment of the course of diseases, monitoring the development of complications and the effectiveness of treatment.
Healthy children are recommended to have a general urine test 1-2 times a year. Children who have had streptococcal infection (tonsillitis, scarlet fever) are advised to pass a control urine test 1-2 weeks after recovery.
The following describes how to decipher the results of urinalysis in children, which means each of the indicators.
Organoleptic analysis
The research is carried out in several stages. The first stage is the method of organoleptic assessment of the biomaterial, in which the characteristics of urine are assessed using the senses. During the study, the volume of urine, its color, odor, transparency and foaminess are analyzed.
Volume
The daily volume of urine depends on the child's age, the amount of fluid he has drunk, the loss of water with sweat, natural emptying, and exhaled air. In children under 3 months of age, diuresis is normally relatively small, since they consume little fluid, but it seems significant due to the frequency of urination.
The daily urination rate in children under 10 years old is calculated by the formula: 600 + 100 × (n-1), where n is the child's age (number of full years). When determining the daily urine output, the number of daytime and nighttime urination is taken into account.
Also, to determine the rate of daily urine volume, depending on the age of the child, you can use the table.
| Age | Daily urine volume, ml |
| Up to 6 months | 250-450 |
| 1 to 2 years | 330-600 |
| 2 to 3 years old | 760-820 |
| 3-5 years old | 900-1070 |
| 5-7 years old | 1070-1300 |
| 7-9 years old | 1240-1520 |
| 9 to 12 years old | 1520-1670 |
| 13 to 15 years old | 1580-1700 |
| 15-18 years old | 1720-1900 |
A deviation from the norm of daily urine output in children may be a sign of a disease of the urinary system.
Excessive urine production is called polyuria. It is diagnosed by comparing the existing diuresis with the norm. Polyuria can be physiological, associated with the use of foods and liquids that cause increased urination, taking diuretics, hypothermia. The pathologies leading to polyuria in childhood include chronic renal failure, kidney stones, pyelonephritis, sarcoidosis, diabetes, and heart failure.
Nocturia is a condition when nocturnal urine output prevails over daytime. Increased formation of night urine can be a variant of the norm in children under two years of age, less often up to 7 years. From 7 to 12 years old, nocturia occurs in only 4% of children. The appearance of nocturia may indicate heart failure, nephrosclerosis, atherosclerosis of the renal arteries, chronic glomerulonephritis, pyelonephritis, cystitis, cirrhosis of the liver, diabetes, pernicious anemia, thyroid diseases.
A decrease in daily urine output (oliguria) is observed with restriction of the drinking regimen, increased sweating, vomiting, diarrhea, febrile diseases, and taking certain medications. Slower urine production can be caused by nephrological diseases (glomerulonephritis, renal vein embolism, pyelonephritis, acute renal failure), hemolytic anemia, urinary tract obstruction, heart failure.
Colour
The normal color of urine in children is straw yellow, lighter than in adults. In newborns, it is almost colorless, in some cases in the first few days after birth it has a reddish or orange tint. Normally, the shades of urine in children range from light yellow to amber.

Normal urine in children is very light, almost colorless.
Discoloration is often associated with changes in diet, vitamins, and certain medications. Pale urine can be a sign of diabetes, kidney problems. In a light brown color, urine is stained with acute infectious processes, febrile conditions, stagnant processes in the kidneys, loss of fluid with vomiting and diarrhea, cirrhosis and burns. Beer-colored urine is a sign of hepatitis, neonatal jaundice, hemolytic anemia. An orange tint is characteristic of hepatic pathologies, uric acid infarction in newborns. Meat slop urine is a symptom of kidney injury, acute and chronic glomerulonephritis. With hemoglobinuria, urine becomes dark brown (black). The high content of leukocytes in the urine gives it a cloudy white color and indicates the presence of inflammation of the genitourinary system.
Smell
The urine of a healthy newborn child does not have a pronounced odor, but as it grows up, it acquires the characteristic odor characteristic of the urine of an adult. The pungent smell of baby urine can serve as a signal of infectious inflammation of the urinary tract, diabetes mellitus, acetonemia.
Frothiness
In healthy children, urine practically does not foam. The physiological reason for the appearance of foam can be rapid and profuse urination. Foaming urine can occur with hypothermia, dehydration, stress, allergic reactions, and the use of chemicals to clean the toilet.
Foamy urine, regardless of the water balance and diet, may indicate the presence of protein in the urine, i.e., proteinuria. Urinary tract infections, amyloidosis, diabetes, renal failure, heart disease, rheumatoid arthritis, sarcoidosis, and anemia can cause increased protein in the urine. A yellow foam is characteristic of jaundice.
Transparency
Fresh urine in children is clear. Its turbidity is associated with a violation of the water-salt balance. Such a reaction may be due to dietary habits, insufficient fluid intake. If the opacity is persistent, it may be a sign of uric acid or calcium oxalate diathesis, pyelonephritis, cystitis, urolithiasis.
Physico-chemical analysis
The second stage of the study is an assessment of the physicochemical indicators of urine analysis (density and acidity).
Specific gravity
The relative density (specific gravity) of urine shows the concentration of nitrogenous compounds dissolved in the biomaterial and characterizes the ability of the kidneys to excrete urine with a high concentration of toxins. In children, the ability of the kidneys to concentrate urine is reduced, therefore, the upper limit of the norm for the volume of daily urine output in them is greater than in adults, and the relative density of urine is less.
The specific gravity of urine may vary depending on the age of the child and some external factors. Indicators of the norm of the relative density of urine in newborns are 1.002-1.020 g / ml. Then the density gradually increases and by the age of three it is 1.010-1.017 g / ml. From the age of 12, this indicator reaches normal values for an adult.
The increased density of urine is due to the appearance of glucose or protein in the urine. It is observed with dehydration or oliguria, uric acid diathesis, blood loss, glomerulonephritis, gastrointestinal diseases, accompanied by frequent vomiting and diarrhea, diabetes mellitus, circulatory failure. An increase in urine density can also be the result of the administration of certain drugs, radiopaque contrast agents.
A low specific gravity of urine can be a sign of diabetes insipidus, chronic renal failure, chronic nephritis, polyuria, glomerulonephritis, pyelonephritis, heart failure. Also, a reduced specific gravity of urine may be the result of a lack of antidiuretic pituitary hormone, kidney damage with heavy metals, alimentary dystrophy, polydipsia, and taking diuretic drugs.
Acidity
The indicator of urine acidity (pH) is normally 4.5-8. The acidity of urine varies depending on the diet, temperature changes and acid metabolism in the stomach and intestines. In infants, this indicator is closer to alkaline, which is explained by the increased consumption of milk. If urine for analysis is collected after a meal, slight alkalization may be recorded.
An elevated pH level may indicate metabolic disorders, chronic renal failure, and tumors of the genitourinary system. Acidification of urine (lowering pH) develops when proteins and fats are predominant in the diet, high physical exertion, fasting, and can also indicate diabetes mellitus, dehydration, diarrhea or tuberculosis. A shift in urine pH values upward or downward from the norm may indicate the formation of stones.
Biochemical analysis
The third stage of urine analysis is an assessment of its biochemical composition.
Protein
There is no protein in the urine of a healthy child, in some cases its maximum allowable content is up to 0.036 g / l. The reason for the temporary appearance of a small amount of protein in the urine may be dehydration, exposure to high or low temperatures, intense physical activity, stress, fever, allergies, burns, and taking certain medications. Physiological proteinuria is observed in newborns in the first days of life.
Protein in urine appears in significant amounts in kidney or urinary tract pathology, kidney injury, diabetes mellitus, infectious diseases, multiple myeloma, hemoblastosis, epilepsy.
Glucose
Sugar (glucose) in a child's urine reflects the state of carbohydrate metabolism. In healthy children, glucose is absent in the urine. If it is found, additional tests should be taken (study of daily urine excretion, fasting blood glucose, glucose tolerance test).
The appearance of glucose in a child's urine is usually associated with diabetes mellitus. Other causes of glucosuria can be hyperthyroidism, liver dysfunction, kidney disease, and pancreatic disease.
Bilirubin
In healthy children, bilirubin is excreted by the liver as part of bile, therefore, it is normally not detected in the urine, with the exception of newborns. In newborns, the presence of bilirubin in the urine is allowed, since the process of excretion of bile pigments has not yet been fully formed. By the end of the second week, the bilirubin level decreases until it disappears completely.
The reason for the appearance of this substance in the urine can be an excess of carbohydrates in the child's diet, as well as liver and kidney pathologies, and impaired outflow of bile. Sometimes elevated bilirubin indicates that stones have formed in the kidneys or urinary tract.
Ketone bodies
Ketone bodies (acetone, acetoacetic and beta-hydroxybutyric acid) in the urine of a child are not normally found, their excess is excreted from the body with sweat. Their appearance in the urine occurs as a result of impaired absorption of glucose by tissues, the supply of which in children is less than in adults. The presence of ketone bodies in urine (ketonuria) can be caused by a lack of carbohydrates in the diet, fasting, stress, excessive physical exertion, hypothermia, and taking certain medications. Pathological causes of ketonuria are infectious or somatic diseases, diabetes mellitus, hyperthyroidism, anemia.

Normally, urine in children does not contain either glucose or ketone bodies.
Microscopy
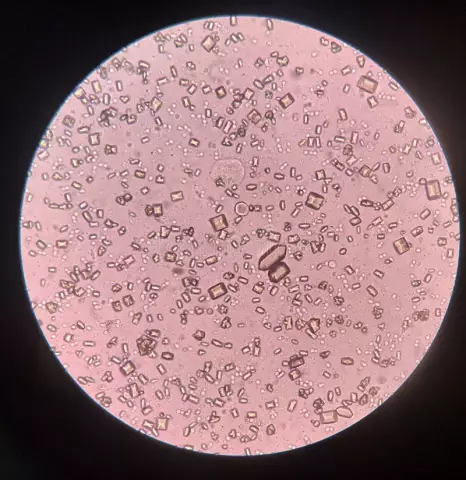
The fourth stage of clinical analysis is the study of the microscopic characteristics of urine. The object of study is the sediment, which is obtained by centrifuging urine. Distinguish between organic and inorganic indicators of microscopic examination. Elements of organic origin include erythrocytes, leukocytes, epithelial cells and casts. Elements of inorganic origin - crystalline and amorphous salts.
Erythrocytes
The permissible content of erythrocytes in the urine of a child under sediment microscopy is 2 per field of view. An increase in the number of erythrocytes indicates inflammation, a viral or bacterial infection associated with an increase in body temperature, trauma, urolithiasis, tumor diseases, intoxication.
Leukocytes
Leukocytes in the urine of a healthy child are normally absent or present in small amounts (0-6 in the field of view). An increased number of them indicates an inflammatory process in the urinary tract.
Cylinders
Cylindrical particles are found only in the presence of protein in the urine, which should not be in healthy children. The appearance of cylinders is characteristic of infectious diseases, acute inflammation of the kidneys, and damage to the renal tubules.
Slime
Normally, there is no mucus in the child's urine. The reason for its appearance is often a violation of the rules of personal hygiene and / or collection of analysis. In other cases, the presence of mucus is a sign of urinary tract inflammation.
Bacteria
Bacteria in the urine of a child is a symptom of infectious and inflammatory diseases of the genitourinary system (pyelonephritis, cystitis, urethritis). Yeast fungi in the urine often appear after inappropriate antibiotic therapy, leading to candidiasis.
Amylase
Amylase (diastase) is an enzyme by which complex carbohydrates are broken down in the digestive tract. Amylase is produced by the pancreas and salivary glands, its level indicates the enzymatic activity of the digestive system. The normal content of amylase in a child's urine is up to 460 units / l. Exceeding this indicator indicates the development of pancreatitis, pathologies of the pancreatic ducts, kidney diseases, diabetes mellitus, diseases of the salivary glands. Low urinary amylase levels can be caused by hepatitis, cystic fibrosis, chronic renal failure, and certain medications.
Salt
The presence of salts in the urine sediment is a sign of inaccuracies in the child's nutrition.
Urine collection rules
In order for the analysis result to not be distorted, it is necessary to follow the rules for collecting material for analysis:
- on the eve of the study, limit the child's consumption of vegetables and fruits that can change the color of urine (beets, carrots, oranges, blackberries, rhubarb), stop taking vitamins;
- cancel diuretics, taking other medicines should be agreed with the doctor who gave the referral for the analysis;
- prepare a clean and dry container for urine in advance (can be purchased at any pharmacy);
- in the morning, thoroughly wash the child's external genitals with warm water, blot with a clean towel;
- collect an average portion of morning urine;
- tightly close the container;
- if possible, deliver the analysis to the laboratory within two hours, if this is not possible, store the container with urine at a temperature of 2-8 ° С.
YouTube video related to the article:

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.