- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Hemangioma of the liver
The content of the article:
- Causes of liver hemangioma
- Forms
- Liver hemangioma symptoms
- Diagnostics
- Liver hemangioma treatment
- Possible complications and consequences
- Forecast
- Prevention
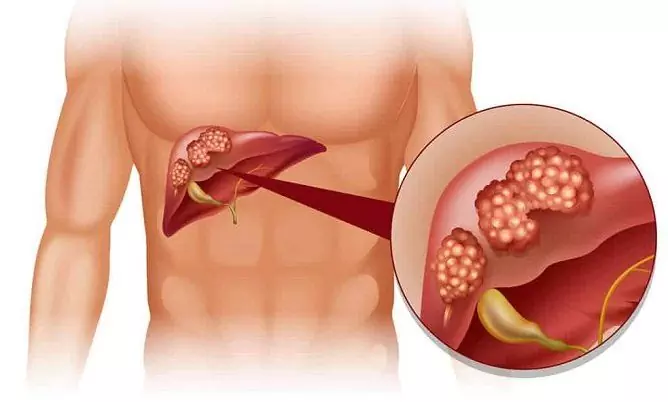
Hemangioma of the liver is a benign vascular neoplasm of embryonic origin. According to statistics, hemangiomas in one or two lobes of the liver are present in 7% of the population, ranking first in prevalence among all benign neoplasms of the hepatobiliary system.

It looks like a liver hemangioma
Causes of liver hemangioma
The cause of hemangiomas in the liver is considered to be a violation of the processes of laying the vessels of the venous bed in the first trimester of pregnancy, due to the effect of damaging factors on the maternal body. Direct correlation between the incidence of hemangiomas and blood group A (II) suggests the presence of a genetic component in pathogenesis and the possibility of inheriting a tendency to form hemangiomas.
Hemangiomas of the liver, diagnosed in infants, resolve on their own in about 80% of cases. In adulthood, large hemangiomatous nodes are more often found in women. According to one hypothesis, estrogens (female sex hormones) increase the growth rate of vascular neoplasms. In many patients, the first signs of hemangioma appeared during pregnancy or while taking estrogen-containing drugs.

Hemangioma of the liver develops as a result of a violation of the processes of laying the vessels of the venous bed in the fetus in the first trimester of pregnancy
According to another version, the causes of liver hemangioma are not associated with tumor growth and lie in congenital malformations of blood vessels, which lead to telangiectasia - persistent expansion of capillaries. With regard to the cavernous form, the assumption is partly confirmed by cases of detection of multiple hemangiomas or total hemangiomatosis, which is uncharacteristic for tumors. The results of pathomorphological studies of the substrate of nodes put liver hemangiomas in an intermediate place between the embryonic tumor and congenital malformation of the hepatic veins.
Forms
In gastroenterological practice there is a tendency towards a broad interpretation of the concept of "hemangioma": this is the name for almost all benign neoplasms of the liver vessels, including venous, cavernous, uviform and capillary angiomas, as well as benign hemangioendotheliomas.
Actually hemangiomas, depending on the structure, are classified into capillary and cavernous. Capillary hemangioma consists of several blood-filled sinusoidal cavities, separated by connective tissue septa. Each sinusoid contains a vessel.
Cavernous hemangioma of the liver, or caveroma, is formed as a result of the fusion of several cavities into one. Cavernous nodes can reach large sizes - 10 cm or more, and in 10-15% of cases in the hepatic parenchyma, two or three formations or multiple small caveromas up to 2 cm in size are simultaneously present.

Stages of liver hemangioma
Liver hemangioma symptoms
In most cases, liver hemangioma does not exceed 3-4 cm in size and does not manifest itself in anything. Clinical manifestations are observed only with an increase in the node up to 5-6 cm or more, when the tumor begins to squeeze adjacent organs and blood vessels and injure tissues, causing internal bleeding, but giant hemangiomas account for no more than 8-10% of cases. Since tumor nodes are characterized by slow growth, the manifestation of hemangioma usually occurs at a mature age - from 40 to 50 years.

Aching pains in the right hypochondrium are early symptoms of liver hemangioma
Early symptoms of liver hemangioma are nonspecific and characteristic of many diseases of the hepatobiliary system:
- aching pain in the right hypochondrium;
- frequent bouts of nausea;
- belching and bitterness in the mouth;
- enlarged liver;
- a feeling of squeezing in the stomach;
- jaundice;
- dyspeptic phenomena.
Diagnostics
Asymptomatic hemangioma is usually discovered by chance during ultrasound, MRI or multispiral CT of the abdominal organs as part of a routine examination or examination for another disease. To clarify the benign nature of the neoplasm, static scintigraphy, a radioisotope study, is required. Selective concentration of the radio indicator in the liver makes it possible to identify altered areas and pathological foci in the hepatic parenchyma and distinguish malignant tumors from benign ones, differentiate hemangioma with cysts and Finnish parasites, clarify its size and localization, and also identify concomitant pathologies - diffuse changes in the parenchyma, hepatomal hypertension, portal hypertension etc.

Hemangioma of the liver is detected on ultrasound, MRI, CT
When the neoplasm is localized in the right lobe of the liver, it is also required to undergo angiography of the celiac trunk to assess the state of blood flow and the presence of blood clots in the arterial, venous and capillary phases. To assess the general condition of the hepatobiliary system, clinical blood tests and liver function tests may be prescribed.
Liver hemangioma treatment
With a small size of the neoplasm, treatment is usually not required. To control the dynamics of the process, the patient is recommended systematic observation by a gastroenterologist. Three months after the diagnosis is made, a control ultrasound or MRI of the liver and biliary tract is prescribed. If the tumor does not increase, the patient undergoes subsequent examinations once or twice a year.
To maintain the functions of the hepatobiliary system, it is important to adhere to a sparing diet and avoid self-medication with medications with a hepatotoxic effect. The recommended diet for liver hemangioma was developed by M. Pevzner and is known in gastroenterological practice as table No. 5. Limit the intake of fats, purines, oxalic acid, salt, coarse fiber and foods rich in extractives that stimulate the production of digestive enzymes. Vegetables and fruits rich in fiber must be ground, white bread must be dried in the oven, and sinewy meat must be finely chopped. Food and drink are best consumed warm. The basis of the menu for liver hemangioma should be dairy and vegetarian soups that do not contain sorrel and tomato paste, boiled and baked dishes; stews can be added occasionally. It is advisable to completely exclude fried foods from the diet. Also subject to the ban are:
- rich broths;
- red meat and offal;
- smoked meats and sausages;
- fatty cheeses and dairy products;
- fatty fish and canned fish, granular caviar;
- mushrooms;
- legumes;
- corn, raw white cabbage, eggplant, radish, radish, turnip, ginger, rhubarb, sorrel, spinach;
- pearl barley, barley and corn grits;
- coarse bread;
- chocolate;
- ice cream;
- rich pastries and puff pastry;
- all types of marinades.
From drinks, freshly squeezed and concentrated juices, coffee, cocoa, green tea, hibiscus, sweet soda and alcohol are undesirable. To improve protein and lipid metabolism, a course intake of vitamin B 12 preparations is shown; if necessary, a course of hepatoprotectors is prescribed.

With liver hemangioma, the patient is shown diet number 5 according to Pevzner
In case of proliferation of the hemangiomatous node and the appearance of alarming symptoms, the question of radical removal of the neoplasm is considered. The operation is supported by:
- knot size more than 5 cm;
- rapid growth of neoplasm (more than 50% per year);
- compression of blood vessels and neighboring organs;
- tumor infection;
- vascular thrombosis and necrotization of hemangioma;
- rupture of tumor tissues with intraperitoneal hemorrhage;
- suspicion of malignancy.
Various surgical techniques are used to remove hemangiomas of different sizes and locations:
- segmental liver resection - removal of one or more segments affected by hemangioma. The boundaries of the segments are determined taking into account the bilio-vascular structure;
- lobectomy - removal of the affected lobe of the liver along the anatomical border;
- hemihepatectomy - removal of the V, VI, VII and VIIIth segments of the right lobe of the liver with drainage of the bile ducts. If necessary, the IV segment of the left lobe is also removed.

Hemangiomas are removed surgically using different methods
To reduce the volume of the operation and prevent postoperative complications, the patient is prescribed a course of hormone therapy before the operation, aimed at reducing the vascular node.
Contraindications to radical surgical treatment are:
- germination of the tumor into large veins,
- cirrhosis of the liver;
- location of hemangiomas in both lobes of the liver;
- multiple hemangiomatosis.
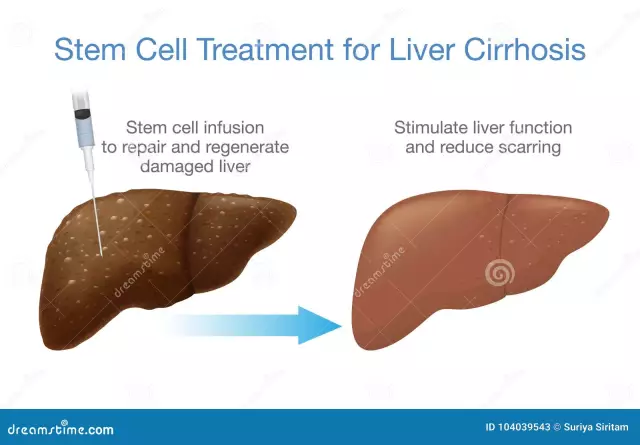
An alternative to surgical treatment can be non-invasive techniques - sclerotherapy and embolization of hemangiomas using radiotherapy, microwave and laser therapy. One of the promising areas is the introduction of ferromagnetic particles into tumor tissues in order to generate a high-frequency electromagnetic field, which causes a significant increase in temperature in the area of the hemangiomatous node and massive death of tumor cells.
Possible complications and consequences
The greatest threat is a rupture of a tumor with extensive intraperitoneal hemorrhage and large blood loss, which can be triggered by sudden movements, excessive physical exertion or trauma to the abdominal region. Therefore, if you have acute abdominal pain lasting more than two hours, you must urgently seek medical help.
Against the background of a persistent increase in pressure in the portal system of the liver, gastrointestinal bleeding may occur; there is also a likelihood of sepsis due to infection of the hemangioma or necrotization of the tissues of the hemangiomatous node due to thrombosis of the vessels supplying the tumor. With total hemangiomatosis with damage to a significant part of the parenchyma, the development of liver failure and liver cirrhosis is possible.
Forecast
With a small hemangioma, the prognosis is favorable: as a rule, a neoplasm up to 4-5 cm in size does not cause a serious deterioration in well-being and does not limit the patient's physical capabilities. After removal of large hemangiomas, the possibility of relapse is not excluded. Malignant degeneration of hemangiomas is extremely rare. One of the signs of malignancy may be the rapid growth of a neoplasm.
Prevention
Due to the congenital nature of the pathology, a pregnant woman is responsible for the prevention of hemangiomas, especially if there have already been cases of vascular neoplasms of the liver in the family history. In the early stages of pregnancy, it is important to avoid viral infections, contact with pesticides, and the use of potent drugs with teratogenic effects.
Only the prevention of complications of liver hemangioma depends on the patient's behavior. To track the dynamics of the process, it is important to undergo scheduled examinations in a timely manner and take action at the first signs of trouble. In order to prevent internal bleeding, it is worth avoiding traumatic sports or using reliable means of protecting the abdominal region, and women, when choosing oral contraceptives or before undergoing hormonal therapy, should warn the gynecologist about the presence of liver hemangioma.
YouTube video related to the article:

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!