- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Colitis
The content of the article:
- Colitis causes and risk factors
- Forms of the disease
-
Colitis symptoms
- Acute colitis symptoms
- Chronic colitis symptoms
- Colitis during pregnancy
- Diagnostics
-
Colitis treatment
- Acute colitis treatment
- Chronic colitis treatment
- Potential consequences and complications
- Forecast
- Prevention
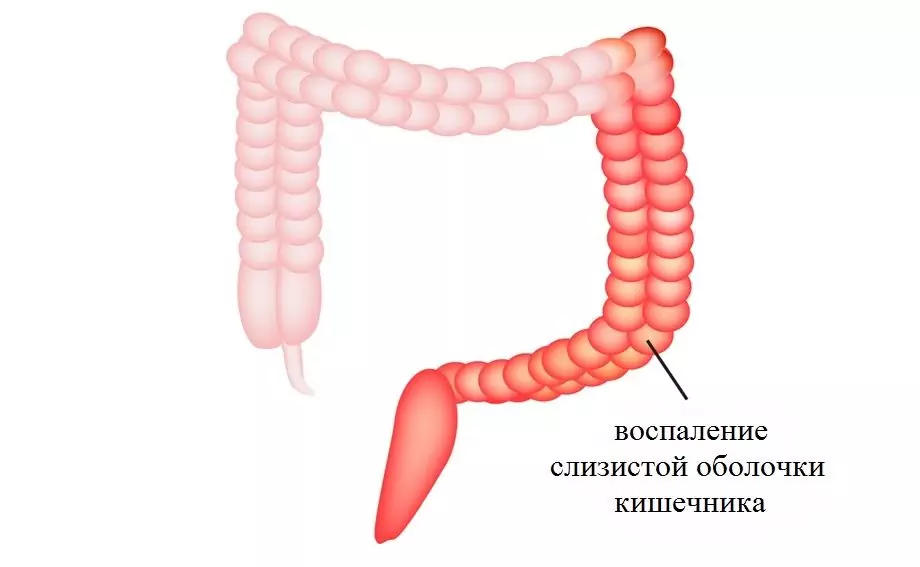
Colitis is an inflammation of the mucous membrane of the large intestine due to its infectious, ischemic, drug or toxic lesion. The disease is very common, it is diagnosed in about 50% of patients experiencing problems with the digestive system. Most often, colitis affects women from 20 to 60 years old and men from 40 to 60 years old.

Colitis accounts for about half of all digestive problems
Colitis causes and risk factors
In about 30% of patients, intestinal infections (salmonellosis, dysentery) are the cause of inflammation of the large intestine. Somewhat less often, the cause of colitis lies in long-term antibiotic therapy, which causes a disturbance in the normal balance of the intestinal microflora, while damage to the mucous membrane is caused by opportunistic microorganisms that normally live in the intestine, but excessively multiply due to dysbiosis.
Eating poor-quality food, alcohol abuse, irrational and irregular nutrition contribute to the development of inflammation of the intestinal mucosa.
In some cases, colitis develops as a complication of diseases of the gastrointestinal tract (hepatitis, pancreatitis, chronic gastritis), and may also be the result of abnormalities and functional insufficiency of the intestine.
Forms of the disease
By the nature of the clinical course, colitis is distinguished:
- acute - characterized by a rapid course, the stomach and small intestine are usually drawn into the pathological process, in this case they speak of acute gastroenterocolitis;
- chronic - the symptoms of colitis are poorly expressed, alternating periods of remission and exacerbations are characteristic.
Depending on the cause that caused the development of the inflammatory process in the large intestine, the following types of colitis are distinguished:
- infectious (tuberculous, salmonella, shigellosis colitis);
- alimentary, that is, due to nutritional errors;
- exogenous toxic caused by intoxication with salts of heavy metals or other poisons;
- endogenous toxic, in which intoxication of the body is caused by the accumulation of metabolic products, for example, uric acid in gout;
- medicinal, arising from prolonged therapy with antibiotics, laxatives;
- mechanical, caused by abuse of rectal suppositories and / or enemas, chronic constipation;
- allergic;
- ischemic, which developed due to a violation of blood flow in the branches of the abdominal aorta that supply blood to the large intestine;
- ulcerative, the development of which is based on complex autoimmune mechanisms.

Types of colitis depending on the location of the inflammation
Depending on the localization of the inflammatory process:
- pancolitis (the entire large intestine is involved in the pathological process);
- typhlitis (inflammation of the cecum);
- transversitis (inflammation of the transverse colon);
- sigmoiditis (inflammation of the sigmoid colon);
- proctitis (inflammation of the rectum).
Colitis symptoms
The clinical picture of acute and chronic colitis is significantly different.
Acute colitis symptoms
Regardless of the etiological factor, the following symptoms are characteristic of acute colitis:
- intense cramping abdominal pain;
- diarrhea up to 20-25 times a day;
- tenesmus (false urge to defecate).
In the feces with acute colitis, impurities of pus, mucus, blood are often found.

In acute colitis, abdominal cramps and repeated diarrhea are observed
A number of general symptoms are also characteristic of acute colitis:
- an increase in body temperature up to 38-39 ° С;
- dry skin and mucous membranes;
- the appearance of a gray plaque on the tongue;
- loss of appetite;
- weakness.
Chronic colitis symptoms
The specific symptoms of chronic colitis are:
- aching dull or cramping pains that are diffuse or localized in a certain part of the abdomen;
- flatulence;
- rumbling intestines;
- stool disorders;
- tenesmus.

Aching abdominal pain, flatulence, stool disorders are characteristic of chronic colitis
In chronic colitis, an increase in the severity of pain syndrome can be caused by tension in the abdominal muscles, setting a cleansing enema, and eating. After a bowel movement, passing gas, or taking antispasmodic drugs, abdominal pain subsides.
Defecation in chronic colitis can occur up to 7-8 times a day. At the same time, the volume of feces is small; impurities of blood and / or mucus are found in them.
When palpation of the abdomen is determined by pain along the colon.
The most common forms of chronic colitis are proctosigmoiditis and proctitis. They arise as a result of bacterial dyskinesia of the large intestine, systematic mechanical irritation of its mucous membrane, usually caused by chronic constipation. The symptoms of these chronic forms of colitis are:
- aching pain in the left iliac region;
- bloating;
- nausea;
- general malaise;
- subfebrile temperature.
With exacerbation of proctosigmoiditis and proctitis, patients develop pronounced tenesmus. Feces take the form of a "sheep's stool" (small dense balls covered with blood and mucus streaks). Palpation reveals pain in the projection of the sigmoid colon.
Common symptoms of chronic colitis include:
- general malaise;
- headaches and dizziness;
- weakness;
- increased fatigue;
- weight loss;
- astheno-neurotic syndrome.
In severe chronic colitis, patients have impaired psychological status. This is manifested by a disturbance in the rhythm of sleep and wakefulness, the appearance of unmotivated anxiety, increased irritability, unexplained anxiety and panic.
Colitis during pregnancy
Patients with this disease have a decrease in fertility by 7-15%. The reasons for the decrease in fertility are the adhesions in the abdominal cavity, conditions after surgical treatment of colitis (resection of the colon with the imposition of an ileostomy or ileoanal anastomosis, subtotal or total colectomy). But even in the case of pregnancy, women with ulcerative colitis may have problems with gestation.
The course of ulcerative colitis during pregnancy is largely determined by the activity of the inflammatory process at the time of conception. If pregnancy occurs against the background of a stable remission of the disease, then in most cases this remission will be maintained. If at the time of conception ulcerative colitis was in the acute stage, then in 30% of women the activity of the inflammatory process will be preserved throughout pregnancy, and in 35% it will even increase. Exacerbations of the disease usually occur in the first half of pregnancy, in the post-abortion and postpartum periods.

Colitis can negatively affect the course of pregnancy, so treatment is necessary
Many patients refuse treatment for ulcerative colitis from the moment of pregnancy. This approach is fundamentally wrong, since an exacerbation of the disease can lead to the development of complications of pregnancy:
- fetal malnutrition;
- spontaneous miscarriage;
- premature birth.
It has been proven that exacerbation of ulcerative colitis during pregnancy increases the risk of miscarriage by more than 2 times. At the same time, adequate drug therapy can reduce the activity of the inflammatory process in the large intestine, transfer the disease to the stage of remission, and thereby improve the prognosis of the course of pregnancy and childbirth. Medicines used to treat colitis during pregnancy do not adversely affect the fetus.
Diagnostics
If you suspect colitis, a set of diagnostic procedures is performed, including:
- general analysis of feces;
- feces for protozoan eggs;
- bacteriological examination of feces;
- general blood analysis;
- contrasting irrigoscopy;
- colonoscopy;
- digital examination of the anus.

To diagnose colitis, colonoscopy and contrast irrigoscopy are performed
Colitis treatment
Treatment regimens for acute and chronic colitis are different.
Acute colitis treatment
Treatment of acute colitis begins with providing the patient with bed rest and a water-tea break in food for 24-48 hours. At this time, only warm drinks (water, unsweetened tea) are allowed. After improving the condition, the diet for colitis is gradually expanded, introducing weak broths, pureed soups, dishes from lean meat, slimy cereals into the diet.
In cases where the cause of acute colitis is an intestinal infection, treatment begins with gastric lavage, and, if necessary, with cleansing enemas. It should be borne in mind that any medication, especially pain relievers, should not be prescribed without a doctor, since the symptoms will be blurred, which will affect the selection of therapy and, therefore, its success.

In acute colitis, gastric lavage and cleansing enemas are indicated.
If a patient has severe paroxysmal pain in the abdomen against the background of acute colitis, antispasmodic drugs are used to relieve them. The use of painkillers for this purpose is undesirable.
From the first days of the disease, broad-spectrum antibiotics are prescribed. After receiving the antibioticogram, the antibiotic is changed taking into account the sensitivity of the causative agent of the disease. If necessary, sulfa drugs can be prescribed as antibiotic therapy.
To prevent the development of dysbiosis and normalize the intestinal microflora, pro- and eubiotics are used.
With severe dehydration, infusion therapy is carried out, aimed at correcting violations of the water-salt balance.
After suffering acute colitis, patients are recommended to adhere to dietary nutrition for 2-3 weeks (table No. 4 according to Pevzner), which provides mechanical and chemical sparing of the intestines. You should switch to regular food, gradually expanding the diet, introducing familiar dishes into it, one a day.
Chronic colitis treatment
With an exacerbation of chronic colitis, treatment is carried out in a hospital setting. A significant role in the treatment of the disease is assigned to a therapeutic diet. All foods that irritate the intestinal mucosa should be excluded from the diet. Food is taken in mashed form in small portions 5-6 times a day.
In cases where chronic colitis is accompanied by constipation, the diet includes dishes from boiled vegetables, bran bread, fruit purees, vegetable oil. To soften the stool, it is important to observe the water regime.

The key to successful treatment of chronic colitis is a therapeutic diet
In case of complications of chronic colitis of infectious genesis, antibiotic therapy is carried out in short courses. If a worm is detected in the feces of eggs, anthelmintics are prescribed. In order to relieve pain, antispasmodic drugs are used.
If chronic colitis is accompanied by the development of diarrhea, then enveloping and astringent agents (decoction of oak bark, jelly, white clay, bismuth nitrate, tannin with albumin) are prescribed to patients inside.
In addition to the drugs listed above, eubiotics, enzymes, enterosorbents, anticholinergics can also be used in the treatment of chronic colitis.
In chronic proctosigmoiditis, systemic treatment is supplemented with local:
- microclysters with protargol, tannin or a decoction of medicinal herbs that have anti-inflammatory and / or tanning effects;
- rectal suppositories with anesthesin, belladonna extract;
- hydrocolonotherapy.
Outside of periods of exacerbation, patients with chronic colitis are shown spa treatment. Balneotherapy contributes to the achievement of persistent and long-term remissions of the disease, improves the psychological state of patients.
Potential consequences and complications
Acute colitis, if treatment is not started on time, may be accompanied by the development of serious and potentially life-threatening complications for the patient:
- dehydration (hypovolemic) shock;
- pyelitis;
- subhepatic abscess;
- sepsis;
- peritonitis;
- acute renal failure.
Severe chronic nonspecific ulcerative colitis can be complicated by:
- intestinal perforation;
- intestinal bleeding;
- intestinal obstruction.
Forecast
The prognosis for acute colitis is favorable in most cases. With timely treatment started, complications develop extremely rarely. In severe forms, untimely or incorrectly selected therapy, the disease can take a protracted course.
With active and long-term therapy of chronic colitis, it is usually possible to achieve a stable remission. Exacerbations of the disease are mainly provoked by gross errors in the diet, if they are avoided, remission can take years.
Prevention
Prevention of colitis is aimed at eliminating factors that can cause the development of an inflammatory process in the large intestine. It includes the following activities:
- careful observance of hygiene rules (washing hands before eating food and after using the toilet, washing fruits and vegetables, drinking bottled or boiled water);
- compliance with food preparation and storage technology;
- rational balanced nutrition;
- refusal of self-medication with antibiotics, laxatives, enemas;
- timely detection and treatment of intestinal infections.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!