- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Treatment of rhinitis in children and adults
The content of the article:
- The reasons for the development of pathology
- Types of rhinitis
- Stages of acute rhinitis
- Diagnostics
-
Treatment
- Drug therapy
- Additional treatments for rhinitis
- Complications
- Prevention
- Video
One of the most common diseases of the ENT organs, which affects both children and adults, is rhinitis, or runny nose. What it is?

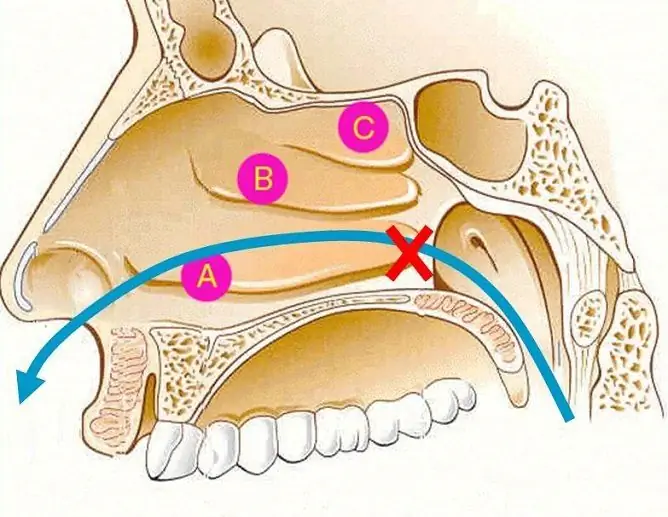
With inflammation of the nasal mucosa, nasal breathing is disturbed
Rhinitis is an inflammation of the lining of the nasal cavity that is characterized by difficulty breathing. It can be an independent disease of viral and bacterial etiology or a symptom of various infectious diseases.
The reasons for the development of pathology
The nasal mucosa provides the main protection for the nasal cavity and upper respiratory tract. It is represented by multilayered columnar ciliated epithelium and mucus covering it.
The nasal secretion performs the following functions:
- protects the nasal mucosa from drying out;
- ensures the normal functioning of the ciliated epithelium;
- moisturizes and heats the inhaled air;
- prevents the settling and reproduction of pathogenic microflora on the mucous membrane;
- provides specific and non-specific immune protection due to the produced lysozyme and secretory antibodies.
Sharp temperature fluctuations and vitamin deficiency in the spring-autumn periods contribute to rapid hypothermia, which reduces the overall resistance of the body to viruses and environmental bacteria.

Curvature of the nasal septum is one of the predisposing factors for the development of rhinitis.
Predisposing factors that reduce the protective functions of the nasal mucosa include:
- a general decrease in immunity;
- hypothermia;
- adverse changes in the gas composition of the inhaled air;
- irritation of the mucous membrane with various chemicals;
- nasal injuries, curvature of the nasal septum;
- the presence of polyps, adenoids in the nose;
- hypertrophy of the turbinates;
- aggravated allergic history;
- recurrent sinusitis;
- concomitant chronic diseases: diabetes mellitus, bronchial asthma, hypothyroidism, etc.
The risk group includes patients receiving immunosuppressive or hormonal therapy.
The main causative agents of the disease are streptococci, staphylococci, pneumococci and filtering viruses: influenza, parainfluenza, adenoviruses, respiratory syncytial viruses, rhinoviruses.

Respiratory syncytial viruses are often the cause of the disease.
Acute bacterial rhinitis is more commonly associated with Streptococcus pneumoniae and Haemophilus influenzae. Chronic inflammation of the nasal mucosa is associated with pathogens more adapted to long-term persistence in the altered structure of the mucous membrane. These include Staphylococcus aureus, Neisseria, Enterobacteriaceae, Pseudomonas aeruginosa.
Viruses have the greatest affinity for the epithelial cells of the nasal mucosa and paranasal sinuses. Reproducing in the cells of the ciliated epithelium, the virus leads to its disorganization. At the same time, a large number of tissue breakdown products accumulate, the local pH changes, the activity of cilia decreases, and a pronounced inflammatory process develops. This causes a violation of mucociliary clearance, leading to stagnation of mucous secretions and creating favorable conditions for the growth and development of pathogenic flora.
Bacteria produce pathogenic enzymes that contribute to a pronounced and persistent infiltration of the epithelium and a bright course of inflammation. Long-term exposure to toxins on the surface of the mucous membrane leads to the development of not only local, but also systemic pathological conditions of the body.
Types of rhinitis
Rhinitis is classified as acute or chronic.
Acute rhinitis can be nonspecific (in the case of the onset of a respiratory infection) and specific (occurs against the background of infectious diseases).
Chronic rhinitis has the following forms:
- catarrhal;
- hypertrophic;
- limited;
- diffuse;
- atrophic or subatrophic;
- simple form;
- fetid coryza (ozena).
Stages of acute rhinitis
The clinical picture of acute rhinitis includes three stages of the course:
- Dry stage of irritation. Acute rhinitis is characterized by a bright onset. The disease begins with sensations of tickling, burning, dryness in the nose and nasopharynx. The body temperature rises to 37 ° C, general malaise, chills, headaches appear. The duration of this stage is on average several hours.
- Stage of serous discharge. It is characterized by an increase in the symptoms of inflammation. A large amount of clear watery fluid sweats from the blood vessels. The glands of the mucous membrane begin to actively produce a secret, and the discharge becomes serous-mucous. The skin of the nasolabial triangle becomes red, swollen, cracked due to the irritating effect of secretions. There is nasal congestion, lacrimation and conjunctivitis are possible.
- The stage of mucopurulent discharge. Begins 4-5 days from the onset of the disease and is characterized by profuse, purulent, yellowish-greenish discharge.
The resolution of the inflammatory process occurs in 7-10 days.
In newborns and infants, acute rhinitis is considered a serious illness with a predominance of general symptoms and frequent development of complications. The younger the child, the more severe the acute form of the common cold. In children of the older age group, the course of the disease does not differ from that of adults.
Diagnostics
The diagnosis is made on the basis of complaints, history and rhinoscopy data.

To prescribe adequate treatment, it is important to determine the etiology of the development of the common cold.
In the first stage of acute rhinitis with anterior rhinoscopy, there is hyperemia of the nasal mucosa, its dryness, and no discharge. In the future, pronounced edema of the mucous membranes of the nose is recorded, the presence of serous or purulent discharge on the walls, less often - fungal plaque.
In infants, the accumulation of infected mucus often occurs in the posterior parts of the nasal cavity, which is associated with the difficulty of secretion into the nasopharynx due to the age-related anatomical features of the choanal structure. On the posterior wall of the pharynx, strips of viscous sputum descending from the nose are visualized, hyperemia of the posterior pharyngeal wall is noted.
In some cases, it is necessary to differentiate acute rhinitis from chronic forms and atopic dermatitis.
Treatment
How to cure rhinitis? According to Dr. Komarovsky, in order to avoid the consequences, an integrated approach is required. When choosing a therapy, one must take into account the alleged pathogens of the infection, the general condition of the body, the presence of somatic diseases.
Drug therapy
At the first stage of acute rhinitis and in the chronic form of the disease, drugs are used to activate local immunity that promote the production of secretory immunoglobulin and improve phagocytosis:
- interferons;
- lysozyme;
- antiviral immunoglobulins;
- lysates of bacterial antigens.

To relieve puffiness of the nasal mucosa, local vasoconstrictor drugs are prescribed
In the second stage of the disease, to restore nasal breathing, it is recommended to instill vasoconstrictor solutions into the nose. In infants and children of the younger age group, it is possible to suck out nasal discharge with a small rubber bulb. The most effective drugs with a vasoconstrictor effect include:
- Tizine;
- Sanorin;
- Xylometazoline;
- Naphthyzin;
- Galazolin.
During the third stage, preference is given to astringent and antimicrobial drugs - Collargol, Protargol.
In the treatment of rhinitis in adults and children, silver proteinate or Protargol is actively used. It is active against many microorganisms:
- staphylococcus (Staphylococcus aureus);
- streptococci (pneumococcus);
- haemophilus influenzae;
- Pseudomonas aeruginosa;
- gonococcus;
- meningococcus;
- viruses;
- mushrooms.
During the use of the drug, a high concentration of silver ions is created in the inflammation focus. Therapy does not lead to the development of dysbiosis. Active ions penetrating the bacterial wall destroy DNA and stop the reproduction of the microorganism. A protective film is formed on the surface of the damaged mucous membrane due to the deposition of silver proteins. The film ensures the normal functional state of cells, which allows quick tissue restoration.
In the treatment of rhinitis, mucolytic drugs (carbocysteine, acetylcysteine) are used to change the rheological properties of nasal secretions. They reduce the viscosity of the secretion, which helps to effectively cleanse the mucous membranes of the nasal cavity from pathological secretions.
Additional treatments for rhinitis
For the treatment of acute and chronic rhinitis, preparations based on seawater are also used. With their help at home, you can carry out irrigation, rinsing, rinsing the nasal cavity and pharynx. Sea water moisturizes mucous membranes, softens crusts and dense exudate, accelerates their separation and excretion. During irrigation or washing, mechanical and thermal effects are exerted on the mucous membrane, which improves tissue trophism and helps restore the protective function of the epithelium.
Often, acute rhinitis spreads to the paranasal sinuses, leading to the accumulation and stagnation of the discharge in the cavity of the paranasal sinuses. To cleanse the sinuses, washings are carried out according to Proetz. The use of this method in many cases avoids surgical intervention and the development of complications.

In the initial stages of rhinitis, reflex therapy is effective, in particular, hot foot baths
In the treatment of rhinitis in children and adults, in addition to basic medicinal prescriptions, reflex therapy is actively used: mustard plasters for calves, hot foot baths, as well as physiotherapy: erythemal doses of ultraviolet rays on the soles of the feet, on the face, microwave (microwaves).
Along with the treatment prescribed by the doctor, you can use folk remedies:
- ginger with lemon and honey;
- thuja oil;
- drops from coniferous broth;
- Kalanchoe juice;
- menthol drops.
In children under 5 years of age, the use of menthol is contraindicated. This is associated with the risk of developing reflex laryngospasm.
Complications
Possible complications of rhinitis:
- tracheobronchitis;
- bronchopneumonia;
- otitis;
- stomatitis;
- ethmoiditis;
- dacryocystitis;
- dermatitis of the vestibule of the nose and nasolabial triangle;
- retropharyngeal abscess.
Prevention
To avoid the development of the disease, it is recommended to observe the following preventive measures:
- systematic hardening;
- periodic intake of fortifying agents and complex vitamin preparations;
- timely diagnosis and treatment of acute and chronic diseases of the nasal cavity, nasopharynx, oral cavity (adenoids, curvature of the nasal septum, chronic sinusitis, etc.);
- using room air purifiers with humidification.
Video
We offer for viewing a video on the topic of the article.

Alina Ervasova Obstetrician-gynecologist, consultant About the author
Education: First Moscow State Medical University. THEM. Sechenov.
Work experience: 4 years of work in private practice.
Found a mistake in the text? Select it and press Ctrl + Enter.