- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Optic neuritis
The content of the article:
- Causes and risk factors
- Forms of optic neuritis
- Symptoms of optic neuritis
- Diagnostics
- Treatment of optic neuritis
- Possible complications and consequences
- Forecast
- Prevention
- Video
Inflammation of the optic nerve is called optic neuritis, or optic neuritis.
The optic or optic nerve is a structure that provides human visual perception. Through its fibers, the image signals received by the retina are transmitted to the brain, where they are interpreted. Any damage to the optic nerve, including inflammation, affects visual function.
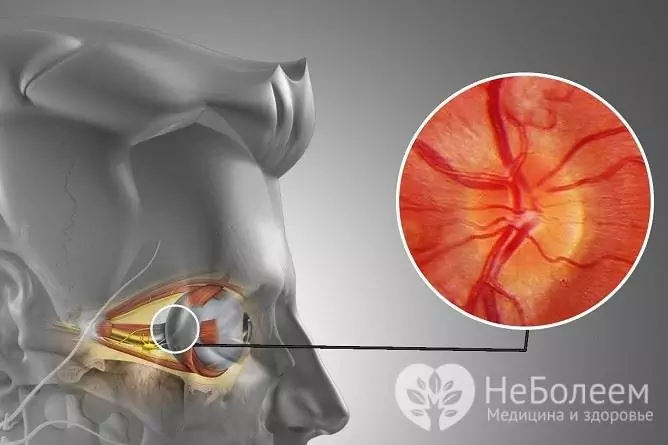
Inflammation of the optic nerve leads to visual impairment
Optic neuritis is the most common pathology of this structure, the incidence is estimated at about 1 case in every 10,000 population. It can occur at any age and in persons of any sex, but most often develops in young (20-40 years old) women (75% of cases).
Causes and risk factors
The most common cause of optic neuritis is the demyelinating process caused by multiple sclerosis, in which the myelin sheath of nerve endings is destroyed. Often, it is the lesion of the optic nerve that serves as the symptom with which multiple sclerosis manifests.
In addition, inflammation of the optic nerve can be caused by:
- intoxication with chemicals (arsenic, lead salts, methanol) and drugs (some antibiotics, ethambutol, quinine);
- infectious diseases (meningitis, tuberculosis, syphilis, Lyme disease, sinusitis of various etiologies, inflammation of the orbit, viral infections);
- optic neuromyelitis (opticomyelitis Devik);
- metastases of the primary tumor to the optic nerve;
- other systemic (autoimmune) diseases;
- Graves' ophthalmopathy (endocrine ophthalmopathy);
- diabetes mellitus (rarely, more often it does not cause inflammatory, but ischemic and degenerative damage to the visual apparatus);
- pernicious anemia;
- injury;
- bee venom (bee sting).
Risk factors include all conditions that contribute to nerve demyelination, primarily autoimmune pathology, as well as injuries of adjacent anatomical areas and inflammatory processes in them.
Forms of optic neuritis
Depending on the involvement of the optic nerve nipple in the inflammatory process, two forms of this disease are distinguished:
- Intrabulbar, or papillitis - the papilla of the optic nerve is inflamed.
- Retrobulbar - the papilla of the optic nerve is intact. This form, in turn, is divided into peripheral, axial and transverse neuritis, depending on the level of nerve damage. It occurs three times more often than papillitis.
Depending on where the inflammatory process has developed, optic neuritis is:
- orbital;
- intracanalicular;
- intracranial.
By the nature of the course, acute optic neuritis and chronic neuritis are distinguished.
Symptoms of optic neuritis
Violation of color perception is the main and constant sign of optic neuritis. At the same time, the colors are not intense enough, they are perceived as muted, some colors may be perceived distorted or not perceived at all.
Other symptoms:
| Sign | Description |
| Decreased vision |
It develops in one eye or both, begins suddenly and grows within a few days. Depending on the degree of inflammation, visual impairment can manifest itself in different ways, from the loss of one central or located near the center of the visual field (scotoma) to the onset of absolute blindness. The depth of perception of images is violated, the contours are blurred. |
| Pain in the affected eye | Appears together with deterioration of vision, increases with eye movement, increases during the first day, reaches a maximum by one and a half (while remaining moderate) and begins to decrease after the second or third day. |
| Photopsy | Moving objects (luminous points, lines, shapeless figures) appear in the field of view; occurs in a third of patients. |
| Uthoff phenomenon | Symptoms worsen with exercise or temperature changes (such as after taking a hot bath or shower). This is an unfavorable sign that is observed in about half of the patients and indicates a significant damage to the brain structures. |
Diagnostics
Eye pains that are aggravated by eye movement in combination with a deterioration in color perception and a decrease in visual acuity in patients and especially young patients are suspicious for optic neuritis. Basic diagnostic methods:
- tests that determine visual acuity, fields, peripheral and chromatic vision;
- examination of the fundus (disc and nipple of the optic nerve);
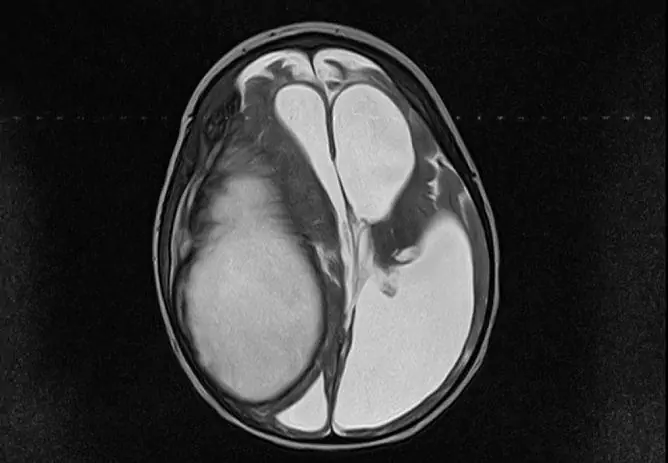
- MRI (Magnetic Resonance Imaging) with gadolinium, which also provides the ability to diagnose multiple sclerosis.

MRI is prescribed for optic neuritis, including for the diagnosis of multiple sclerosis
Depending on the results of the examination, consultations of related specialists may be shown - a therapist, an otolaryngologist (for sinusitis), a rheumatologist (if a demyelinating disease is suspected), an endocrinologist, an infectious disease specialist, an oncologist, etc.
Treatment of optic neuritis
The use of corticosteroids is recommended, which is absolutely necessary for suspected neuromyelitis optics or multiple sclerosis, and corticosteroids are recommended to be administered intravenously - it has been established that such a regimen can delay the progression of multiple sclerosis by at least 2 years. Typically, a regimen is used that includes intravenous methylprednisolone for three days, followed by oral prednisolone for 11 days. Dexamethasone may be given as a parabulbar injection.
In order to reduce papillary edema (with intrabulbar form of the disease), diuretics may be prescribed. With a bacterial origin of inflammation, antibiotics (Ampicillin, Cefrtiaxone) are indicated. Immunoglobulins, plasmapheresis, vitamin therapy can also be used.
Metastatic lesion of the optic nerve requires antitumor therapy and / or surgery. Intoxication - detoxification therapy. The main treatment for optic neuritis caused by multiple sclerosis or other autoimmune pathology is treatment of the underlying disorder.
Possible complications and consequences
Optic neuritis can resolve spontaneously, without treatment, but in this case, there is a high risk of recurrence, in addition, due to refusal to see a doctor, developing multiple sclerosis or other disease may be missed.
A complication of acute neuritis can be its chronicity, i.e. the development of chronic inflammation of the optic nerve, which is fraught with a gradual deterioration in vision. Long-term inflammation can lead to the death of the optic nerve with the onset of complete and irreversible blindness in the affected eye.
Forecast
In most cases, optic neuritis can be cured, pain and severe visual impairment disappear within a few days, and visual function is fully restored within two to three months. However, in 25% of patients, relapses of the disease are observed, not only in the previously injured eye, but also in the second, as well as inflammation of other nerves. This is usually due to the presence of an underlying chronic (autoimmune, demyelinating) disease.
Prevention
Prevention measures for optic neuritis:
- preventing head injuries;
- prevention of intoxication, if they occur, immediate and adequate detoxification;
- prevention of infectious diseases;
- timely treatment of ENT pathology (sinusitis).
Unfortunately, effective prevention of Devik's opticomyelitis, multiple sclerosis and other autoimmune diseases does not exist.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!