- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Frozen pregnancy
The content of the article:
- Causes of a frozen pregnancy and risk factors
- Forms of frozen pregnancy
- Symptoms of a frozen pregnancy
- Diagnostics
- Treatment
- Possible complications and consequences
- Forecast
- Prevention
Frozen pregnancy is one of the forms of miscarriage, which is characterized by the complete cessation of development and death of the embryo or fetus. It usually develops in the I-II trimester, in primiparous women over 30 years old.

Source: phunungaynay.vn
A normal pregnancy lasts 40 obstetric weeks from the last menstrual period. In the first trimester, the organs of the fetus are laid, by the end of the first trimester the placenta is completely formed, through which the fetus receives nutrients, and the end products of metabolism are removed. From the 28th week, the fetus is considered viable. If the development of the fetus stops before this time without expulsion from the uterine cavity, such a pregnancy is called frozen.
The share of those who have died is 10-15% of all pregnancies.
Causes of a frozen pregnancy and risk factors
The mechanism of development of a frozen pregnancy is not fully understood. Presumably, pregnancy stops developing due to fetal abnormalities, defects incompatible with life. Often, such a pathological process develops against the background of hormonal imbalance in the mother (decreased production of progesterone, increased level of androgens).
Infectious diseases, more often urogenital, can lead to the termination of the development of pregnancy, but they can also be of any other localization. The infectious agent is able to penetrate into the uterine cavity from the parts of the reproductive system that are located below (ascending route of infection) and infect the amniotic fluid. The fetus swallows amniotic fluid, the infection spreads, affecting the skin, lungs, gastrointestinal tract of the fetus, which leads to its antenatal death. The descending route of infection may be due to chlamydial or gonorrheal infection, in which case the infection penetrates from chronic foci of inflammation in the ovaries and fallopian tubes. The highest risk of developing a missed pregnancy is if a pregnant woman develops rubella, toxoplasmosis, or infection with cytomegalovirus,since in this case the pathogen affects the central nervous system of the fetus, causing the formation of severe anomalies, often incompatible with life.
In the second or third month of embryogenesis, the pathological process can develop against the background of antiphospholipid syndrome. At the same time, the fetus receives less nutrients and stops developing. According to statistics, without the necessary therapy for women with antiphospholipid antibodies, the death of the embryo or fetus occurs in 90-95% of cases.
In addition to the above, the cause of a frozen pregnancy is:
- Rh-conflict between mother and fetus - develops in women with a negative Rh factor and repeated pregnancy with a Rh-positive fetus;
- teratozoospermia - the presence of a large number of sperm with altered morphology in the father's ejaculate.
Risk factors include:
- menstrual irregularities;
- stillbirth, multiple miscarriages, history of abortion;
- endocrine diseases;
- cardiovascular pathology;
- kidney disease;
- taking certain medications;
- exposure to the body of ionizing radiation;
- insufficient stay in the fresh air;
- poor nutrition;
- excessive physical and / or mental stress;
- wearing tight clothing that squeezes the internal organs;
- bad habits;
- industrial hazards;
- abrupt climate change.
Forms of frozen pregnancy
Depending on the results of ultrasound, two forms of frozen pregnancy are distinguished:
- anembryonia;
- death of the embryo or fetus.
Echographically, anembryonia is divided into two types:
- The embryo is not visualized, the size of the uterus corresponds to the fifth to seventh week of pregnancy, the average diameter of the ovum does not exceed 2-2.5 cm.
- The absence of an embryo or visualization of its remnants, the growth of the ovum at a normal rate, the initiation of the villous chorion is not clearly detected.
Symptoms of a frozen pregnancy
There is no standard gynecological picture with a frozen pregnancy.
The pathological process in the first trimester is characterized by a decrease in the basal body temperature, an improvement in the general condition of a woman occurs - the nausea that had taken place earlier, tension and soreness of the mammary glands, stabilize the psycho-emotional state. During a gynecological examination, there is no increase in the uterus, which would correspond to the gestational age. Freezing in the early stages of pregnancy may not have clinical manifestations up to spontaneous abortion. If a spontaneous miscarriage does not occur, the body temperature rises, chills appear, the general condition of the patient deteriorates sharply.
A sign of a frozen pregnancy after the 18-20th week is the lack of fetal motor activity. The occurrence of bleeding, as well as pain in the lower abdomen, which can radiate to the lower back, indicates the beginning of the process of rejection of the dead fetus by the body.
The medical literature describes extremely rare cases when a dead fetus is mummified, and a frozen pregnancy persists for many years, without causing any subjective sensations in the patient, but leading to infertility.
Diagnostics
During the diagnosis of a frozen pregnancy, complaints and anamnesis are collected, an objective examination, instrumental and laboratory studies. Sometimes what happened does not attract the attention of the patient and is only discovered by the obstetrician-gynecologist who is observing the pregnancy during a routine examination.
If a frozen pregnancy is suspected, a laboratory determination of the level of human chorionic gonadotropin (hCG) in the blood is carried out. In case of fetal death, the level of hCG decreases and does not meet the standards established for the current gestational age.
In order to detect possible infectious diseases, they resort to the polymerase chain reaction method, a microbiological examination of the contents of the vagina. A blood test may be required for the content of certain hormones, determination of a coagulogram, genetic analysis, etc.

Source: astrakhan-pek.ru
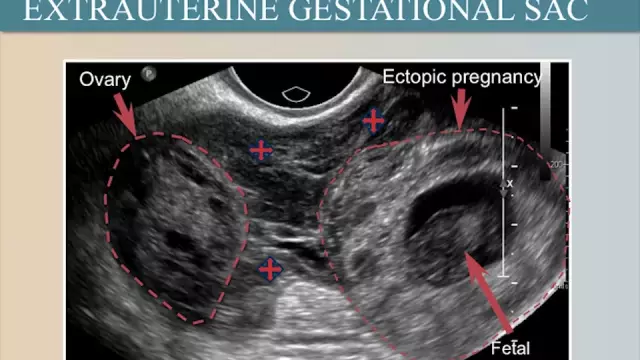
From the methods of instrumental diagnostics, ultrasound of the pelvic organs is used. In the course of the study, it is found that there are no signs of fetal activity (heartbeat, physical activity). With anembryo, the embryo is absent in the ovum after the 7th week of pregnancy, while the size of the ovum does not correspond to the norm of the expected gestational age.
In some cases, the size of the ovum is normal, but a smaller embryo is visualized without a heartbeat. In the case of recent fetal death, the ovum and fetus without signs of vital activity are visible. With a longer stay of the dead fetus in the uterine cavity, its visualization is impossible, the structure of the ovum changes abruptly (deformation, fuzzy shape and contours of the ovum, multiple constrictions, etc. are determined). Signs of fetal death at a later date include severe lack of water and damage to the fetal skull bones with displacement of bone fragments and overlapping of one fragment after another.
Treatment
With the development of a pathological condition in the first trimester of pregnancy and the absence of signs of an infectious and inflammatory process, expectant tactics can be chosen. In such cases, a decrease in the level of hCG, as a rule, leads to uterine contractions and the expulsion of the ovum from the uterine cavity.
In the absence of spontaneous abortion, it is necessary to remove the embryo or fetus from the uterine cavity. With the development of a pathological process in the first two months of pregnancy, an artificial abortion is most often performed with the help of hormonal drugs (medical abortion). For this purpose, a combination of a progesterone antagonist and a prostaglandin E1 analogue is used, which induce uterine contractions. After the expulsion of the fetus, hysteroscopy is indicated - a procedure that, if necessary, turns from diagnostic to therapeutic, allowing the elements of the ovum or placenta remaining in the uterus to be removed.
At a later date, they resort to the prompt removal of the ovum. In the I-II trimester of pregnancy, vacuum aspiration can be used - the extraction of the ovum from the uterine cavity using a special vacuum suction. This manipulation is usually performed without dilating the cervix (in some cases, the use of metal dilators is required, with the help of which the cervix is opened for the introduction of the necessary abortive instruments). During the operation, a catheter is inserted into the uterus, which is attached to the suction, a uniform negative pressure is created in the uterine cavity, while the ovum, regardless of its location, is separated from the wall. After vacuum aspiration, the patient is shown an ultrasound examination of the pelvic organs. In case of incomplete abortion, a second procedure is performed,in some cases, tissue remains are scraped out with a curette. The advantages of the method include low trauma, the possibility of performing vacuum aspiration on an outpatient basis, simplicity and short duration of the procedure (2-5 minutes), as well as a short recovery period.

Source: poznayka.org
If it is impossible to remove the ovum by vacuum aspiration, they resort to scraping with a frozen pregnancy. This surgical intervention is carried out in a hospital setting and consists in cleaning (curettage) of the uterus in order to remove the membranes and the dead embryo (surgical abortion). If a patient with a frozen pregnancy is found to have hypercoagulability, hyperaggregation, disseminated intravascular coagulation before curettage, preparation in the form of corrective therapy is necessary (introduction of blood substitutes, fresh frozen plasma, antihemorrhagic drugs). In the course of scraping with a frozen pregnancy, the cervical canal is expanded, after which the ovum is scraped out with a curette, along with the placenta and uterine mucosa. Curettage for a frozen pregnancy is carried out under general or local anesthesia. In the early postoperative period, anticoagulant and antiplatelet therapy is indicated.
If pathology is detected in the second trimester of pregnancy, the dead fetus can also be removed by artificial childbirth.
After removal of the embryo or the dead fetus, it is sent for histological examination. If you suspect the presence of chromosomal abnormalities, a genetic study of the embryo is shown.
After surgery, the patients are given drug therapy. In order to prevent the infectious and inflammatory process with the existing risk of its development, anti-inflammatory and antibacterial drugs are prescribed. Of no small importance for the possibility of having a child in the future is the restoration of the functionality of the endometrium. For this purpose, immunocorrective, hormonal and restorative therapy is prescribed. In order to prevent the formation of adhesions, restore the endometrium, and normalize the functions of the ovaries, they resort to physiotherapy (magnetotherapy, ultrasound therapy, water and mud therapy, hirudotherapy, gynecological massage).
Symptomatic treatment of a frozen pregnancy during the recovery phase may include taking painkillers, sedatives, and vitamin complexes. In some cases, to restore the psychoemotional state, women need to consult a psychologist or psychotherapist.
After the treatment of a missed pregnancy, it is recommended to refrain from planning the next pregnancy for 6-12 months. During this period, hormonal contraceptives can be prescribed, both for the purpose of contraception itself, and in order to normalize the hormonal background, the menstrual cycle.
Possible complications and consequences
In the absence of timely diagnosis and a properly selected treatment for a frozen pregnancy, there is a risk of developing disseminated intravascular coagulation (DIC). In this condition, the likelihood of death is high.
Complications that can develop after surgery include menstrual irregularities, inflammatory diseases of the reproductive organs, uterine perforation, pseudoembolism, acute blood loss, sepsis, and an increased risk of complications during the next pregnancy.
Forecast
Despite the fact that it is not possible to save the fetus, provided timely and adequate treatment of a frozen pregnancy, the prognosis for life, health and the subsequent possibility of conception, bearing and the successful completion of pregnancy is favorable. With prolonged presence of the dead fetus in the uterine cavity, the prognosis worsens.
Prevention
In order to prevent the development of a frozen pregnancy, it is recommended:
- timely treatment of hormonal pathologies, infectious and other diseases that can cause a frozen pregnancy;
- medical and genetic counseling in planning pregnancy;
- rejection of bad habits;
- balanced diet;
- avoidance of stressful situations;
- rational work and rest regime;
- getting enough night sleep.
YouTube video related to the article:

Anna Aksenova Medical journalist About the author
Education: 2004-2007 "First Kiev Medical College" specialty "Laboratory Diagnostics".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!