- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Lichen planus
The content of the article:
- Lichen planus causes and risk factors
- Forms of the disease
- Symptoms of lichen planus
- Diagnostics
- Treatment of lichen planus
- Possible complications and consequences
- Forecast
- Prevention
Lichen planus (LP, Wilson's lichen, true lichen) is a chronic disease that affects the skin, mucous membranes, and occasionally nails. Pathology occurs in all age groups, but it is more often diagnosed in persons 30-60 years old. Women are more susceptible to disease. The share of lichen planus is approximately 1-2.5% in the structure of all dermatological pathologies.

Cutaneous manifestations of lichen planus
Lichen planus causes and risk factors
The causes of lichen planus are not fully understood. The disease often occurs against the background of a decrease in the activity of the immune system or with metabolic disorders, as a result of which the cells of the skin and mucous membranes begin to respond inadequately to exogenous stimuli. A genetic predisposition to lichen planus was revealed. The disease is not transmitted by contact.
Risk factors are:
- diseases of the gastrointestinal tract;
- pathology of the cardiovascular system;
- dental diseases;
- chronic infectious processes;
- endocrine disorders;
- allergic reactions;
- strong emotional upheaval;
- taking certain medications;
- chronic trauma to the oral mucosa;
- galvanic currents in the oral cavity (occur in the presence of prostheses and fillings from different metals).
Forms of the disease
Depending on the characteristics of the clinical picture, the following forms of lichen planus are distinguished:
- typical;
- hypertrophic warty (verrucous);
- atrophic;
- pemphigoid (vesicular);
- lightning;
- pigmented;
- pointed (perifollicular);
- annular;
- erosive and ulcerative;
- rare forms (obtoznaya, serpigious, erythematous, etc.).
According to the nature of the flow of CPL, there are the following forms:
- acute (duration up to one month);
- subacute (up to six months);
- long-term, or chronic (more than six months).
Symptoms of lichen planus
The clinical picture varies depending on the form of the disease.
Elements of the rash with a typical form of lichen planus have an umbilical depression in the central part and are predominantly red, brownish or cyanotic in color. The presence of elements of a rash with a shiny waxy surface is the most characteristic symptom of lichen planus. The brilliance of the lesions is best seen at an angle in the light of a lamp directed in the same way. Most often, the size of the papules is small (2-3 mm), but they can grow over time. The lesions are prone to merging with each other, the surface of the morphological elements formed in this way begins to peel off.
The rash is often accompanied by itching, which intensifies at night, and sometimes painful sensations that are permanent. The pain can be intense, leading to poor appetite, sleep disorders, and a decrease in the quality of life in general.
Rashes are localized on the flexor surface of the forearms, in the wrist joints of the hands, on the inner thighs, as well as on the legs, groin, armpits, and on the oral mucosa. There is practically no rash on the palms, feet, face and scalp. In some cases, mucous membranes are affected in isolation.
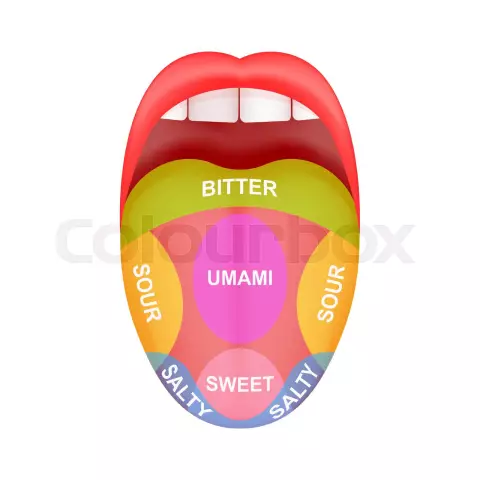
With the localization of rashes on the oral mucosa, white stripes often appear on the inner surface of the cheeks, their formation is not accompanied by itching, pain or other discomfort. Lips, gums and tongue can be involved in the pathological process. The rash on the tongue is white and resembles the clinical picture of leukoplakia. Their appearance is accompanied by dry mouth, dullness of taste.
With genital localization of LP in women, hyperemia of the mucous membranes of the external genital organs is observed, as well as the appearance of white stripes on them, which are easily injured and can bleed. There is no pain or itching. In men, ring spots of white or purple color are formed around the glans of the penis, itching and pain are also not observed.
In some patients, the nail plates are involved in the pathological process. When the nails are damaged, their surface becomes red due to the inflammatory process, cloudy spots and longitudinal striations form on it, the nails become thinner and become brittle. In rare cases, the esophagus, eyelids, ear canal and anus are involved in the pathological process.
The disease usually lasts for a long time (from several months to several years).
With a hypertrophic warty (verrucous) form of the disease, rashes are usually localized on the legs. Elements of the rash may have a cyanotic hue. This form of lichen planus is characterized by warty layers on the surface of the rash elements.
With the atrophic form of lichen planus, atrophic changes and seals at the site of resolved lesions are characteristic. When the elements of the rash are localized on the scalp, point baldness occurs.
The pemphigoid form is a rare variety of lichen planus. It is localized mainly on the legs. It is manifested by the formation of small vesicles on the skin, filled with serous contents (in some cases, serous-hemorrhagic, that is, with an admixture of blood). Often, in addition to vesicles, the patient has rashes typical of LPL.

Erythematous lichen planus
With fulminant red flat lichen, large foci of waxy nodular elements appear on the skin, located in the form of chains. In some cases, the lesions may be small, arranged in strips resembling scars. As a rule, large areas of the skin are affected. Rashes can be localized on the back of the ears and neck, on the elbows, hands, as well as on the abdomen and buttocks. The palms, soles and external genitals are not affected with this form of lichen planus.
For the pigmented form of the disease, in addition to lesions typical for lichen planus, the presence of pigment elements (brown spots or nodules) localized on the skin of the abdomen, buttocks and legs is characteristic.
With acute lichen planus, in addition to the usual rashes for the disease, sharp-pointed papules appear on the scalp, neck, shoulder blades, as well as on the pubis and groin. After the rash resolves, small scars remain in its place.
In the case of the annular form of lichen planus, the elements of the rash quickly increase in size, at the same time, healing of their central part begins. Thus, a kind of ring is formed (lesions can have the form of arcs, half rings, garlands). After the resolution of the rash, in place of the central part of the morphological element, an area of skin with a brighter color remains. In many cases, this form of pathology affects the genital area, the inner surface of the legs. The annular form of the disease is more common in men.
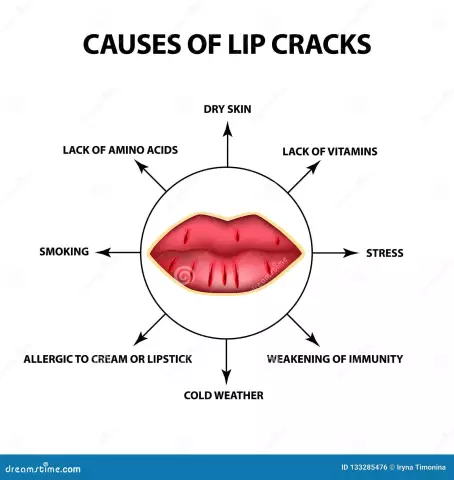
The erosive and ulcerative form of lichen planus is the most severe and difficult to treat type of disease. With this form, the mucous membranes of the oral cavity are usually affected, sometimes rashes form on the lips. Patients complain of pain and burning sensation in the mouth. The lesions are transformed into erosion, the areas of the mucous membrane around them become edematous and hyperemic. The morphological elements are covered with fibrinous plaque and films; when the films are removed, the surface under them is easily injured and bleeds. Some elements of the rash disappear on their own, others - under the action of therapy, however, after the treatment, recurrence of erosions in the same or in another area of the mucous membrane is possible.
Malignancy of the elements of the rash with lichen planus in the mouth is observed in about 1% of cases of the disease. Usually, malignant degeneration of the cells of the affected areas is observed in elderly patients with a long history of erosive-ulcerative LP of the oral cavity in the anamnesis. At the same time, there is an increase in the process of keratinization (keratinization) and compaction of the infiltrate at the base of the morphological element.
Diagnostics
To make a diagnosis of lichen planus, collect complaints and anamnesis, as well as an objective examination of the patient. The indicative signs of the disease, which attract attention during the examination, are the presence of a rash with a depressed center and a characteristic color on the skin. In the case of lichen planus, the patient has a Wickham symptom ("Wickham grid"), which consists in the fact that after the elements of the rash are smeared with oil, a grid formed by intersecting lines appears on their surface. With the localization of rashes on the mucous membranes, visual diagnosis of pathology is difficult.
To clarify the diagnosis, apply:
- skin biopsy with further histological analysis of the material obtained (lichen planus is characterized by the presence of moderate epithelial hyperplasia, signs of hyperkeratosis, parakeratosis and granulosis, slight vacuolization of the basal layer cells, lymphoid infiltrate in the subepithelial layers);
- cytological examination (with suspicion of malignant degeneration of cells);
- allergological research;
- determination of immunological parameters;
- serological analysis (to exclude secondary syphilis);
- blood chemistry;
- analysis of the electrochemical composition of saliva and determination of the presence of galvanic currents.

Skin biopsy helps confirm the diagnosis of lichen planus
Specific changes in the general analysis of blood and urine with lichen planus were not found. In some cases, in the general analysis of patients' blood, an increase in the number of leukocytes, eosinophilia, an increase in the erythrocyte sedimentation rate (ESR) is noted.
Differential diagnosis with secondary syphilis, squamous cell carcinoma, pemphigus vulgaris, non-acantholytic pemphigus (pemphigoid), exudative erythema multiforme, systemic lupus erythematosus, leukoplakia, candidiasis is required.
Treatment of lichen planus
Therapeutic tactics for lichen planus depends on the type, clinical picture of the disease, the prevalence of the pathological process, the presence of concomitant pathologies and / or complications, as well as on the general condition of the patient. The disease is capable of spontaneous healing, but in this case, there is a high probability of relapse.
First of all, it is necessary to eliminate irritating factors, if any (for example, to replace dentures, fillings, which injure the mucous membrane of the oral cavity, etc.).
With the localization of skin rashes and their absence on the mucous membranes (or in the case of minor damage to the mucous membranes), bromine-containing sedatives, antihistamines, and vitamin complexes are used. In the absence of positive dynamics, drugs containing adrenal cortex hormones (glucocorticoids) are prescribed.
In case of relapses, drugs are recommended that improve the oxygen supply of tissues.
As a local treatment for lichen planus, anti-inflammatory ointments (including those containing glucocorticoids), alcohol solutions are used. When a bacterial infection is attached, local antibiotics are used. In the case of severe itching, external use of drugs with menthol, antihistamines, citric acid, application of ointments containing glucocorticoids is indicated.

Large elements of the rash are removed by cryodestruction or electrocoagulation
Of the methods of physiotherapeutic treatment, inductometry (exposure to the body with a high-frequency alternating magnetic field) on the affected areas, electroscopy, and ultraviolet radiation are used.
Large elements of the rash can be eliminated by cryodestruction or electrocoagulation.
With lichen planus in the oral cavity, in general, the same drug treatment is used as with the localization of skin rashes, in addition, a hypoallergenic sparing diet is indicated for patients. Avoid eating too hot food, as well as foods that can cause additional trauma to the oral mucosa (in addition to highly allergenic foods, spicy foods, spices, and alcohol are excluded from the diet).
Possible complications and consequences
The consequence of the transferred red flat lichen can be baldness, destruction of the nail plate. The most severe, but, fortunately, rare complication is the malignant transformation of cells of the damaged surface.
Forecast
With correctly selected and timely treatment, the prognosis is favorable.
Prevention
Since the reasons contributing to the occurrence of lichen planus are not fully known, there is no specific prevention of the disease. General preventive measures include hardening the body, strengthening the immune system, giving up bad habits, correcting metabolic disorders, if any, sanitizing the oral cavity.
Prevention of relapses of lichen planus is carried out by treating chronic infectious diseases, as well as neuropsychiatric and psychosomatic disorders.
Patients with oral cavity LP are subject to dispensary registration with regular preventive examinations.
YouTube video related to the article:

Anna Aksenova Medical journalist About the author
Education: 2004-2007 "First Kiev Medical College" specialty "Laboratory Diagnostics".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!