- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Metabolic acidosis
The content of the article:
- Causes of metabolic acidosis
-
Types of acidosis
- Large anion gap metabolic acidosis
- Metabolic acidosis with normal anion gap
- Signs
- Features of metabolic acidosis in children
- Diagnostics
- Treatment
- Prevention
- Consequences and complications
- Video
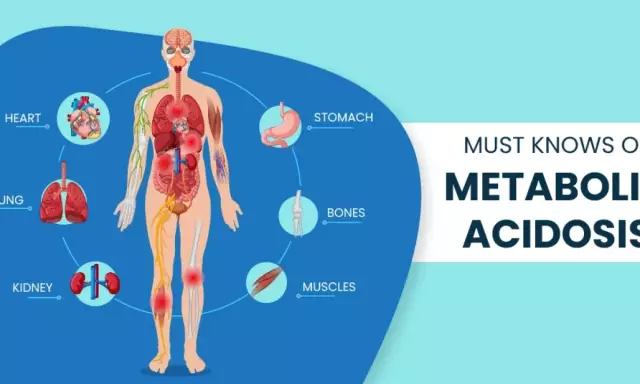
Metabolic acidosis (from Latin acidus - sour) is a violation of the acid-base balance in the body, when there is an accumulation of acids due to their increased production or consumption, reduced excretion from the body, as well as as a result of the loss of bicarbonates through the kidneys or the gastrointestinal tract. Until a certain time, compensatory mechanisms work, but then the acid load exceeds their capabilities, and acidemia occurs - what is sometimes called blood acidification. The lower limit of the normal arterial blood pH is 7.35 (a value in the range of 7.35-7.45 is considered normal), acidemia is said when the arterial blood pH becomes lower, ie, less than 7.35. This condition leads to disruption of the biochemical reactions in the body,the consequence of which are disorders of almost all body functions, including severe, life-threatening respiratory and cardiac disorders.
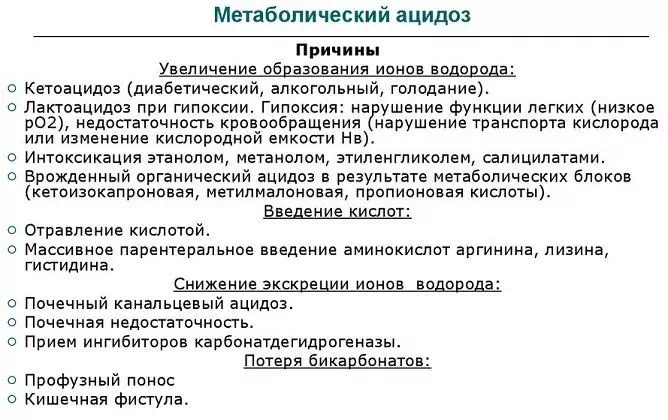
Causes of metabolic acidosis
Acidosis is not an independent disease, but a symptom that can develop in many diseases and pathological conditions, including:
- life-threatening conditions (clinical death and postresuscitation illness, shock, multiple organ failure, sepsis);
- lung disease (severe asthma, pneumothorax, sleep apnea);
- neuromuscular disorders (Guillain-Barré syndrome, amyotrophic lateral sclerosis, myasthenia gravis);
- infectious diseases (botulism);
- renal failure;
- decompensated diabetes mellitus;
- starvation;
- dehydration (dehydration);
- complicated pregnancy;
- prolonged diarrhea;
- intestinal fistulas;
- intestinal dysbiosis (excessive synthesis of D-lactate by the intestinal microflora);
- alcohol intoxication;
- drug overdose;
- poisoning with methyl alcohol (methanol), antifreeze, ethylene glycol, as well as salicylates and some other drugs.
Prolonged excessive physical exertion (hard exhausting work, vigorous training) can lead to metabolic acidosis.

The main causes of metabolic acidosis
Types of acidosis
Distinguish between metabolic acidosis with a large and normal anion gap.
Anionic interval - the difference between the concentration of Na + (sodium ions) in blood serum and the sum of the concentrations of Cl - (chlorine ions) and HCO 3 - (bicarbonate ions, or hydrocarbonate); thus, it is determined by the formula Na + - (Cl - + HCO 3 -). It is an important diagnostic indicator to help determine the type of acidosis and the conditions that led to them, such as severe poisoning.
Large anion gap metabolic acidosis
| Acidosis type | Description |
| Ketoacidosis | It develops in conditions of a lack of glucose, instead of which the body uses free fatty acids, from which keto acids (β-hydroxybutyric and acetoacetic) are formed in the liver. The cause may be diabetes mellitus, chronic malnutrition, chronic alcoholism, congenital acidemia (matilmalonic and isovalerian). |
| Lactic acidosis (lactic acidosis, lactic acidosis) |
The accumulation of lactate (lactic acid) is due to its increased synthesis and / or reduced utilization. Excessive synthesis is observed with shock, reduced utilization - with impaired liver function, generalized shock. Lactic acidosis, in turn, is divided into three types: · A - develops in violation of blood oxygenation or tissue hypoperfusion; · B - there are no signs of hypoperfusion, develops in liver pathology, malignant tumors, intoxications and some congenital metabolic disorders; · D - arises from the overgrowth of lactobacilli, which leads to an overproduction of D-lactate. |
| Acidosis due to renal failure | It develops due to a decrease in the excretion of acids and a violation of the reabsorption of HCO 3 -. In addition, there is an accumulation of urate, hippurate, phosphates, sulfates, which aggravates the condition. |
| Acidosis due to intoxication | It develops due to the formation of acidic metabolic products of toxins or their induction of lactic acidosis. |
| Acidosis due to rhabdomyolysis | The breakdown of muscles leads to the release of anions, which is the cause of acidosis. One of the rarest species. |
Metabolic acidosis with normal anion gap
This type is also known as hyperchloremic acidosis, due to the increasing concentration of Cl - in the blood, as these ions are reabsorbed in the kidneys instead of HCO 3 -.
This type of pathology is caused by the loss of HCO 3 - due to renal dysfunction or through the gastrointestinal tract, impaired excretion of acids in the kidneys.
GI-related causes include gastric drainage and severe diarrhea. Other types of metabolic acidosis with a normal anion gap include acidosis due to:
- obstruction of the ureters;
- removal of the bladder;
- intoxication with toluene, spironolactone, amphotericin B, acetazolamide, amiloride.
According to the degree of compensation, the following types of metabolic acidosis are distinguished:
- Compensated - the pH of arterial blood does not fall below the lower limit of the norm, i.e., at least 7.35. Manifested by rapid breathing, increased blood pressure, increased heart rate.
- Subcompensated - arterial blood pH is in the range of 7.34-7.25. It manifests itself as a deterioration in the work of the heart (arrhythmia may appear), shortness of breath, nausea, vomiting, diarrhea.
- Decompensated - arterial blood pH below 7.24. In addition to dysfunction of the cardiovascular system, it is characterized by disorders of the gastrointestinal tract and signs of damage to the central nervous system (headache, dizziness, drowsiness, blurred consciousness, stupor, coma).
Signs
Metabolic acidosis may be asymptomatic if the acidemia is mild and slow to develop. In other cases, its signs are nonspecific, that is, they are characteristic of many conditions.
Significant and / or rapidly developing acidemia is manifested by nausea and vomiting, and an increasing deterioration in well-being. The characteristic signs include hyperventilation due to hyperpnea (inhalation becomes slow and deep, but the frequency of inhalation does not increase - the so-called Kussmaul breathing) due to the action of compensatory processes. Compensatory shortness of breath develops. As the acidemia increases, cardiac function is impaired, and cardiogenic shock and ventricular artimia may occur.
Slowly developing (chronic) acidemia leads to bone demineralization.
Possible signs of acidosis include:
- deterioration of myocardial function, determined by a decrease in stroke and minute blood volume, as well as a decrease in sensitivity to the action of inotropic and vasopressor drugs;
- decrease in peripheral vascular resistance;
- hyperkalemia;
- spasm of the arterioles of the gastrointestinal tract and kidneys, which is accompanied by a decrease in intestinal motility and diuresis;
- decrease in surfactant synthesis;
- the development of seizures.
Since these signs are nonspecific, they should be assessed, paying attention to the history data that indicate the possible occurrence of acidosis:
- prolonged diarrhea;
- diagnosed diabetes mellitus or indications of its possible presence (increased thirst, polyuria, weight loss, epigastric pain, etc.);
- insufficient nutrition, starvation;
- renal failure (nocturia, polyuria, weight loss, pruritus);
- taking certain medications (for example, salicylates) or using toxic substances (for example, methanol);
- visual disturbances, increased photosensitivity, loss of visual fields;
- kidney stone disease;
- signs of intoxication.
Features of metabolic acidosis in children
Metabolic acidosis is a common pathology in pediatric practice. Acute severe metabolic acidosis generally has the same causes and manifestations as in adults, while chronic acidosis leads to rickets and growth retardation.
Most cases of metabolic acidosis encountered by pediatricians are related to lactic acidosis due to shock in critical conditions of various etiologies.
Diagnostics
Kussmaul breathing in combination with other signs allows suspecting metabolic acidosis. In order to confirm the diagnosis, carry out:
- blood test for electrolytes and gases;
- a blood test for ketone bodies (helps in determining diabetic, alcoholic and malnutrition-induced acidosis);
- determination of the level of lactate in plasma;
- determination of the anionic interval in blood and urine;
- a clinical blood test (leukopenia or leukocytosis may indicate possible acidosis due to sepsis, anemia may be accompanied by lactic acidosis).
If acidosis is suspected due to renal failure, the following are additionally determined:
- plasma renin activity;
- plasma aldosterone;
- transtubular potassium gradient;
- fractional excretion of bicarbonate, and some others.
Of the methods of hardware diagnostics, the following is used:
- electrocardiography (ECG);
- ultrasound examination (ultrasound) of the kidneys;
- measurement of blood pressure, heart rate, etc.
Treatment
Since metabolic acidosis is not an independent disease, but only one of the symptoms of another, underlying disease, etiotropic therapy is aimed at the underlying disease.
With decompensated, and in some cases with subcompensated form of metabolic acidosis, parenteral and then oral administration of buffer solutions containing sodium bicarbonate, glucose solution, sodium chloride are indicated. Solutions Acesol, Disol, Trisol, which help to eliminate electrolyte imbalance, can be prescribed. They contain acetate, which, as a result of oxidation, helps alkalinize the environment. Lactasol has a similar effect. Buffer solutions are used to normalize blood pH values.

Trisol is a drug for the treatment of decompensated metabolic acidosis
In severe conditions, resuscitation, hemodialysis, and artificial ventilation are performed.
Prevention
Prevention consists in preventing the development of pathological conditions accompanied by metabolic acidosis, and if they have developed, in their timely and adequate treatment.
Consequences and complications
Complications of metabolic acidosis can be:
- dehydration;
- a decrease in the volume of circulating blood;
- increased blood clotting, accompanied by the risk of thrombus formation;
- circulatory disorders (including such serious ones as myocardial infarction, infarction of parenchymal organs, peripheral thrombosis, stroke);
- arterial hypo- and hypertension;
- impaired brain function;
- coma;
- fatal outcome.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!