- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Intestinal diverticulosis
The content of the article:
- Causes and risk factors
- Diverticulosis forms
- Bowel diverticulosis symptoms
- Diagnosis of diverticulosis
- Intestinal diverticulosis treatment
- Possible complications and consequences
- Forecast
- Prevention of diverticulosis
The concept of "diverticulosis" reflects the presence of diverticula (from Lat. Diverticulum - road to the side), clinical manifestations of the disease may be absent. Various factors lead to the appearance of diverticula, which are based on the weakness of the connective tissue. In the case of the formation of multiple diverticula, they speak of divertculosis. Diverticular disease is a broader definition applied to diverticulosis and its complications.

Source: gastrosapiens.ru
Causes and risk factors
Diverticulosis is one of the most common pathologies of the gastrointestinal tract in Europe, and is generally characteristic of developed countries. In rural Africa and vegetarians, it appears less often, so its pathogenesis is usually associated with a lack of vegetable fiber in the diet. The likelihood of developing diverticulosis increases with age.
The main part of the risk group is people over forty years old: at sixty, every third person suffers from diverticulosis, and from seventy-five - every second person. The incidence of this disease in women and men is the same.
Also, the formation of diverticula is facilitated by:
- obesity;
- transferred intestinal infections;
- flatulence;
- taking laxatives.
Risk factors:
- hereditary predisposition;
- elderly age;
- frequent constipation;
- poor nutrition, fiber deficiency, excess meat and flour products in the diet;
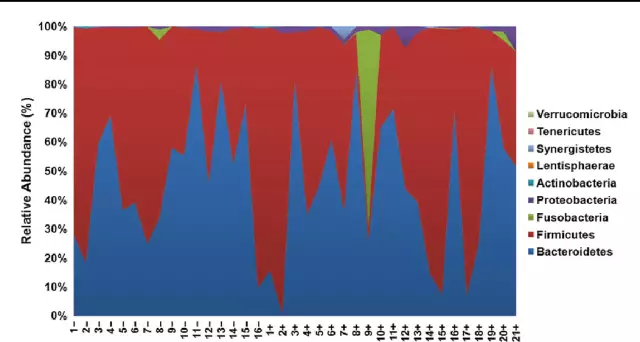
- violation of microcirculation of blood in the intestinal veins.
Diverticulosis forms
There are three main clinical forms of diverticulosis:
- asymptomatic;
- diverticulosis with clinical manifestations;
- complicated.
Because intestinal diverticula can be congenital or acquired, diverticulosis is divided into hereditary and acquired forms. With hereditary weakness of the connective tissue, they speak of its innate nature. In such cases, diverticula appear at a young age (5% of cases) and mainly affect the right large intestine.
The acquired form of the disease is based on an increase in pressure in the intestine (as a result of flatulence, constipation, disturbances of peristalsis), which leads to the appearance of areas (pockets) with high pressure, which facilitates pushing through the muscular and submucous layer of the intestinal mucosa. As a result of nutrition with a lack of plant food and fiber and a predominance of flour and meat products, frequent constipation begins, the motor function of the large intestine is impaired.

Source: pancreatit.info
Bowel diverticulosis symptoms
In most cases, diverticulosis is asymptomatic. Patients do not make any complaints, and the manifestations of the disease are usually accidentally detected during the examination of the intestines at a dispensary examination or during examination for another disease.
Later, with the development of an uncomplicated form, stool disorders appear. Such disorders are accompanied by intestinal colic, a feeling of fullness in the abdomen, flatulence, etc. In this phase, the symptoms of bowel diverticulosis are difficult to distinguish from those of irritable bowel syndrome.
The uncomplicated form of the disease has the following manifestations:
- recurring sharp or aching spastic abdominal pain without signs of inflammation;
- increased gas formation;
- feeling of incomplete bowel movements after bowel movement;
- pain worsens after eating and goes away after bowel movement or gas.
In the acute phase (complicated diverticulosis), pain appears in the iliac fossa on the left, and signs of acute inflammation increase.
With an increase in inflammatory processes occur:
- alternating diarrhea and constipation, unstable stools;
- loss of appetite;
- nausea, vomiting;
- sharp, intense pain in the left lower quadrant of the abdominal cavity;
- increased body temperature;
- the presence of mucus in the feces;
- tachycardia;
- local peritoneal phenomena;
- an increase in leukocytes in the blood.
In the future, when a local inflammatory process occurs, perforation of the intestinal wall may occur, while the disease becomes diffuse from a local one.
Diagnosis of diverticulosis
Diagnosis of diverticulosis is based on the data of the initial examination, anamnesis and the results of diagnostic procedures that reveal diverticula and the presence of functional changes in tissues:
- general blood and urine tests;
- coprogram;
- colonoscopy (flexible sigmoidoscopy);
- irrigoscopy (X-ray examination of the intestine with a contrast agent);
- Ultrasound;
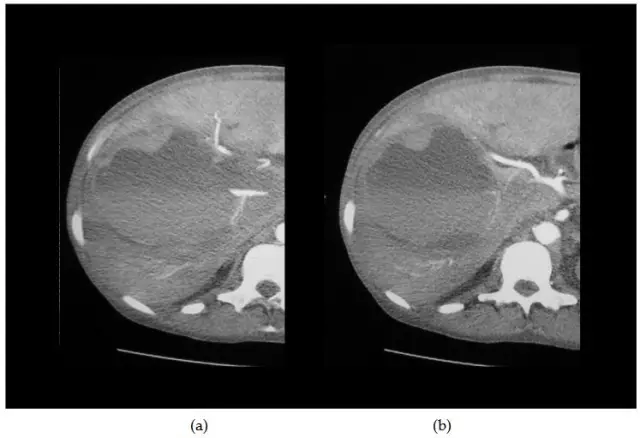
- CT scan;
- scintigraphy (scanning with erythrocytes labeled with technetium).
In the course of irrigoscopy, the progress of barium is observed on an X-ray monitor, visualizing hernia-like protrusions of any structure protruding beyond the outer contour of the intestine. Irrigoscopy with double contrast can be performed no earlier than a month and a half after the relief of acute diverticulitis.

Colonoscopy is prescribed in cases where it is impossible to reliably exclude the presence of carcinomas and small polyps in areas with diverticulosis. This method is also chosen in cases where the patient is presented with rectal bleeding. However, colonoscopy is difficult to perform in the presence of spasm, which is observed with extensive diverticular disease, in this case, the movement of the instrument is difficult when passing the segment of the intestine affected by diverticulosis.
In complicated cases, CT and sonography reveal a thickening of the intestinal wall and large abscesses.
Intestinal diverticulosis treatment
In the asymptomatic form, drug treatment of bowel diverticulosis is not prescribed. Therapy consists in following a special diet and maintaining water balance, which helps to eliminate constipation and normalize bowel function.
Diet for intestinal diverticulosis is the main part of therapy. The daily diet should be composed in compliance with several rules:
- the diet should include foods rich in fiber, vegetables and fruits (with the exception of cereals, seaweed, cauliflower);
- increase the content of natural fermented milk products in the diet;
- give up fried, smoked dishes, semi-finished products, flour products;
- limit the use of meat dishes and products containing animal fats;
- give up legumes and mushrooms;
- use prunes, dried apricots or herbal teas as a laxative.
In some cases, in order to normalize digestion, the administration of drugs that reduce gas production, enzymes, prokinetics and probiotics is indicated. The use of laxatives should be limited. they increase the pressure in the intestines.
In cases where the inflammatory process in the intestine has nevertheless occurred, but serious complications have not developed, treatment is practiced at home, in compliance with bed rest. In addition to strict adherence to diet and maintenance of water balance, drugs that stimulate peristalsis, enzyme preparations, antibiotics, antispasmodics (Mebeverin), analgesics, laxatives and drugs that increase stool volume, for example, ispaghula husk, are prescribed.
In case of complicated diverticulosis, the patient is shown hospitalization, additional diagnostic tests are carried out, therapy is prescribed, including antibiotics (cephalosporins, Amoxicillin with clavulanic acid, Metronidazole, Gentamicin), intravenous administration of salt and glucose solutions for detoxification and correction of water-electrolyte disturbances.
In the case of the development of diverticulitis, the presence of acute attacks of diverticulosis, conservative treatment is not used: the risk of intestinal perforation and the development of peritonitis is too great. During the surgical operation, the area of the intestine affected by diverticula is removed (hemicolectomy, resection of the sigmoid colon with the imposition of a primary anastomosis). The scope of the surgical intervention and its technique depend on the individual characteristics of the course of the disease. To reduce intraintestinal pressure, such operations are often combined with colon myotomy.
Indications for surgical treatment of diverticulosis:
- the presence of two acute attacks (for patients over forty years old - one) with the failure of conservative treatment;
- massive bleeding in the abdominal cavity;
- development of intestinal obstruction;
- phlegmon or retroperitoneal peritonitis;
- rupture of an abscess, internal or external intestinal fistulas.
Possible complications and consequences
The uncomplicated form of diverticulosis can proceed for years without making itself felt, but after a while (in 10-20% of patients) inflammation develops. With an increase in inflammatory processes, the development of serious diseases is possible:
- perforation;
- paracolic abscesses;
- intestinal obstruction;
- intestinal bleeding;
- accumulation of inflammatory infiltrate;
- internal and external fistulas.
With perforation (perforation) of the diverticulum, dangerous purulent complications can develop: phlegmon, peritonitis, abscesses.
With the breakthrough of an abscess diverticulum in a closed cavity, peritonitis, an internal or external fistula, develops. When a diverticulum is perforated into the bladder, a colovesical fistula is formed. Fistulas can open to other organs, and intestinal-cutaneous fistulas can form. In patients with colovesical fistulas, pneumaturia and urinary tract infections are sometimes noted in the absence of complaints of disturbances in the work of the gastrointestinal tract.
Sometimes bleeding occurs from the vessels that penetrate the neck of the diverticulum. Such bleeding is often profuse and is manifested by general symptoms of blood loss and an admixture of blood in the stool. Usually, profuse bleeding develops from a solitary diverticulum located in the right colon.
Fecal diffuse peritonitis associated with diverticular disease develops as a result of necrosis of the intestinal wall, leading to the leakage of purulent and fecal masses into the abdominal cavity. The patient's condition is characterized as extremely difficult, with acute manifestations of peritonitis, septic shock.
In the area where diverticulitis exists for a long time, an adhesion process often occurs, which can result in intestinal obstruction. Smooth muscle hypertrophy, scars from past bouts of diverticulitis, inflammatory changes can cause acute obstruction of the colon and complete closure of its lumen.
Forecast
In most cases, intestinal diverticulosis has a favorable prognosis, the success rate of conservative therapy increases in the case of treatment with the first episode of the disease and is 70%, however, in some situations, diverticulosis leads to the development of severe complications and life-threatening conditions.
Prevention of diverticulosis
Eating a daily diet high in fiber, drinking enough water, and exercising regularly can help prevent diverticulosis.
YouTube video related to the article:

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!