- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Atopic dermatitis
The content of the article:
- Causes and risk factors
- Forms of the disease
- Disease stages
- Symptoms
- Diagnostics
- Treatment
- Possible complications and consequences
- Forecast
- Prevention
Atopic dermatitis is a chronic, genetically determined inflammatory-allergic skin disease with a recurrent course, characterized by primary itching, papular eruptions and lichenification.

Cutaneous manifestations of atopic dermatitis
Papular rashes are noncavity elements of various diameters (from 1 to 20 mm), consistency and color that rise above the skin level.
The term "lichenification" means thickening of the skin, their hyperpigmentation and increased skin pattern.
In 1891 L. Brock and L. Jacquet from a numerous group of skin diseases, accompanied by papular rashes and thickening of the skin, isolated an independent disease that develops as a result of scratching in places of primary itching, and designated it with the term "neurodermatitis". The term "atopic dermatitis" was proposed in 1935 by M. Sulzberger and is used to denote skin lesions resulting from hereditary pathology of the whole organism - atopy.
Atopy is a genetically fixed state of increased allergic readiness of the body, characterized by the presence of an excessive amount of immunoglobulins of class E (IgE) in the blood.
In developed countries, allergic diseases are a serious socio-economic problem - according to various sources, 35-40% of the population suffer from them. In the structure of allergic pathology, atopic dermatitis occupies one of the leading positions: according to the results of a global international study, it accounts for every fifth case of allergic dermatoses.
Since the 90s of the twentieth century, the incidence of atopic dermatitis has doubled, which is explained by the unfavorable environmental situation, chronic stress, the spread of artificial feeding, mass vaccinations, inappropriate nutrition with a large proportion of refined foods and the widespread prevalence of bad habits. However, the exact causes of dermatitis are unknown.
Women are more susceptible to atopic dermatitis (65%).
It was found that atopic dermatitis develops in 81% of children if both parents are sick, in 59% if only one of the parents is sick, and the other has an allergic airway pathology, and in 56% if only one of the parents is sick.
In 70% of cases, atopic dermatitis is a harbinger of conditions such as hay fever, urticaria, bronchial asthma, allergic rhinitis, Quincke's edema. In this case, the disease is regarded as the first manifestation of the "allergic march".
Causes and risk factors
Atopic dermatitis is a multifactorial disease, the causes of which lie in a complex combination of inherited characteristics and external influences.
The root cause of the disease - a hereditary predisposition to allergies - is provoked by a violation of the genetic control of the production of cytokines, in particular interleukin-4 and interleukin-17 (IL-4, IL-17), which is accompanied by an excessive production of immunoglobulin E, a specific reaction to allergens and general hypersensitivity. Local mechanisms of atopic dermatitis are also hereditary: the accumulation of Langerhans cells in the skin, an increase in the number of IgE receptors on their membranes, a violation of the permeability of the skin barrier, etc.
External provoking factors:
- unfavorable course of pregnancy, childbirth and the postpartum period;
- malnutrition of the mother during pregnancy (high antigenic load on the fetus) and lactation;
- late attachment to the breast;
- artificial feeding;
- disruption of immunological immunity to food allergens as a result of poor nutrition in the first year of life;
- neuroendocrine disorders;
- frequent contact with allergens;
- concomitant gastrointestinal pathology, especially disorders of the normal intestinal flora (89%), leading to damage to the digestive barrier and accelerated absorption of antigens;
- psychotraumatic effects (impaired functioning of the central nervous and peripheral systems that control the mechanisms of itching);
- irrational regime with excessive physical and emotional stress.

The cause of atopic dermatitis is a hereditary predisposition to allergies
Causal allergens (up to 100% of cases in young children):
- cow's milk (86%);
- chicken protein (82%);
- fish (63%);
- cereals (45%);
- vegetables and fruits of orange and red color (43%);
- peanuts (38%);
- soy proteins (26%).
In fact, food allergy is a starting sensitization, on the basis of which an increased sensitivity to other allergens is formed by cross mechanisms.
Forms of the disease
There is no generally accepted classification of atopic dermatitis. There are several criteria by which the disease is classified.
Options for the course of severity:
- mild - limited skin lesion (no more than 5%), mild itching that does not worsen the patient's sleep, unexpressed skin symptoms (slight hyperemia or swelling, single papules and vesicles), rare exacerbations (1-2 times a year);
- moderate - widespread skin lesions (up to 50%), moderate or intense itching, inflammatory skin reaction (significant hyperemia, exudation or lichenification, multiple scratching), exacerbations 3-4 times a year;
- severe - more than 50% of the skin is affected, intense, debilitating, severely disturbing the quality of life itching, severe hyperemia, tissue edema or lichenification, multiple scratches, cracks, erosion, continuously recurrent course.
By the intensity of the course: acute, subacute and chronic process.
By prevalence:
- limited dermatitis - no more than 5% of the skin area is affected;
- widespread dermatitis - up to 50% of the skin area is affected;
- diffuse dermatitis - more than 50% of the skin area is involved in the inflammatory process.
Clinical forms of atopic dermatitis:
- exudative ("wet");
- erythematous-squamous (there are areas of redness and scaling with fuzzy boundaries, small papules and scratching prone to merging);
- erythematous-squamous with lichenification;
- lichenoid;
- pruriginous (large, persistent, hemispherical papules, accompanied by severe itching).
Disease stages
In accordance with the age of patients, the following stages of the disease are distinguished:
- Infant (up to 2 years old), manifested by acute skin reactions localized on the face (in the forehead, cheeks, often extending to the neck), scalp, outer surface of the legs and buttocks. The process is represented by redness, swelling, oozing, followed by the formation of crusts.
- Children's (from 2 to 13 years old). There is a thickening of the skin, the presence of erythematous papules with typical localization in the folds of the skin (lichenoid form), in 52% of children at this stage there is a lesion of the face (atopic face), rashes in the flexor surfaces of the wrists, ankle joints, elbow and popliteal fossae.
- Adolescent and adult. It is characterized by a continuously recurrent course, pronounced lichenification, dryness and peeling of the skin with a predominant lesion of the skin of the face, upper body, extensor surfaces of the limbs.

Stages (stages) of atopic dermatitis
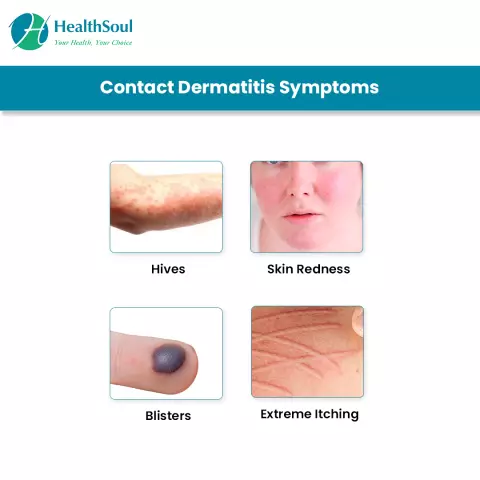
Symptoms
In 1980, J. Hanifin and H. Rajka introduced diagnostic criteria for atopic dermatitis, which are divided into two groups: mandatory symptoms and additional ones.
Mandatory manifestations of the disease:
- a certain appearance of the rashes and their location (in adults, lichenization and scratching are localized on the flexor surfaces, in children - on the face and extensor surfaces, the presence of crusts, cracks, and the symmetry of the process are characteristic);
- chronic course with episodes of exacerbations (under the influence of provoking factors) and remission, seasonal in nature, the onset of the disease no later than adolescence;
- itching;
- atopy in history or heredity aggravated by atopy.
Additional symptoms include:
- the onset of the disease at an early age;
- xerosis (dryness and roughness of the skin);
- ichthyosis, hair lichen or increased pattern on the palms;
- Denier-Morgan folds (deepened wrinkles on the lower eyelids);
- dark circles around the eyes (allergic glow);
- conjunctivitis;
- keratoconus (the so-called conical cornea);
- anterior subcapsular cataract;
- itching with increased sweating;
- the first type of skin reactivity (delayed-type hypersensitivity reaction);
- perifollicular localization of rashes;
- pallor or flushing of the face;
- folds on the front of the neck;
- frequent infectious skin lesions;
- dermatitis on the skin of the hands and feet;
- eczema of the nipples;
- white dermographism;
- elevated serum IgE levels.
Depending on the age of the patient and the stage of the disease, clinical manifestations can vary: the nature of skin rashes, their localization and severity of the process change.
Diagnostics
The diagnosis of "atopic dermatitis" is established on the basis of a characteristic clinical picture, hereditary allergic anamnesis (a correctly collected anamnesis in 90% of cases allows to formulate a correct diagnosis) and the results of additional studies:
- skin tests;
- provocative tests with allergens;
- studies of the level of immunoglobulin E.
To standardize the diagnosis of atopic dermatitis in European countries, the SCORAD system was introduced (Consensus Report of the European Task Force on Atopic Dermatitis, 1993), and a scale of atopic dermatitis was adopted. It combines indicators such as the area of the body affected, the intensity of clinical manifestations, and subjective symptoms (itching and insomnia). The severity of the symptoms of the disease is evaluated in points and summed up.

Assessment of the severity of atopic dermatitis using the SCORAD system
An atlas of reference photographs was compiled, demonstrating the intensity of erythema, edematous and papular elements, oozing, crusts, excoriation, lichenification and dry skin.
Treatment
Since atopic dermatitis belongs to the group of inflammatory-allergic skin diseases, the main directions of treatment are:
- prevention of contacts with causally significant allergens, for which elimination diet therapy and control of adverse environmental factors are recommended;
- systemic pharmacotherapy with antihistamines, anti-inflammatory drugs and allergy mediator blockers;
- immunotherapy;
- correction of concomitant pathology (treatment of diseases of the digestive tract, metabolic drugs and antioxidant therapy, normalization of the functional state of the nervous system, sanitation of foci of chronic infection);
- medicines for external use to relieve symptoms of the disease and special cosmetics to eliminate a defect in the protective function of the skin, soften and moisturize it.

As part of the complex therapy of atopic dermatitis, cosmetic emollients and moisturizers for the skin are shown
Possible complications and consequences
The main complication of atopic dermatitis is infection of the skin (pyoderma, viral infection or fungal infection) when scratching.
Forecast
Complex pathogenetic pharmacotherapy and the use of external agents, with strict adherence to the recommendations, ensure a stable remission of the disease and prevent its recurrence. The prognosis in this case is favorable.
Prevention
Creating a hypoallergenic environment is the most important preventive measure. Key recommendations:
- exclusion of food provocateurs;
- ensuring adequate ventilation in households;
- maintaining optimal humidity, temperature and air purity;
- refusal to use furniture and interior items that serve as dust collectors (carpets, books, flowers, heavy curtains, upholstered furniture, soft toys);
- a ban on the use of feather and down pillows and blankets;
- the use of hypoallergenic cosmetics;
- contact with household chemicals only with protective gloves;
- refusal to wear clothes made of fur and wool;
- refusal to keep animals, birds and aquariums at home.
In addition, it is recommended:
- dispensary observation of an allergist;
- long-term spa treatment in the summer;
- carrying out restorative procedures (hardening, UV irradiation, massage).
YouTube video related to the article:

Olesya Smolnyakova Therapy, clinical pharmacology and pharmacotherapy About the author
Education: higher, 2004 (GOU VPO "Kursk State Medical University"), specialty "General Medicine", qualification "Doctor". 2008-2012 - Postgraduate student of the Department of Clinical Pharmacology, KSMU, Candidate of Medical Sciences (2013, specialty "Pharmacology, Clinical Pharmacology"). 2014-2015 - professional retraining, specialty "Management in education", FSBEI HPE "KSU".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!