- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Rathke pocket cyst
The content of the article:
- The reasons
- Symptoms
- Complications
- Diagnostics
- Treatment
- Consequences and forecast
- Video
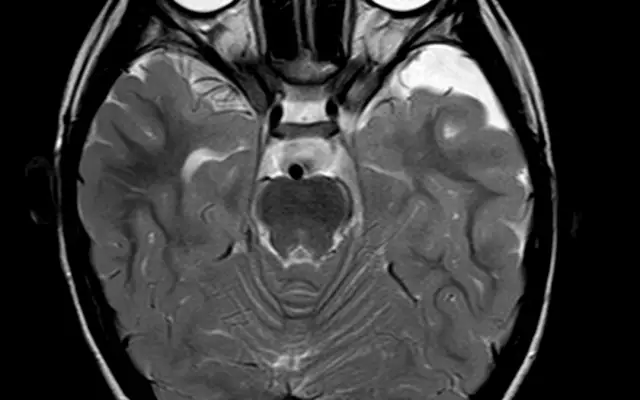
Rathke's pocket cyst (KKP) is a round-shaped benign formation that occurs as a result of improper involution of the Rathke's canal. It is located between the anterior and posterior lobes of the pituitary gland, as well as in front of its funnel, mainly in the area of the sella turcica. The diameter of the KKR can be from a few millimeters to 5-6 cm. The internal contents usually have a mucous (mucous) character, but sometimes the cavity of the cystic neoplasm is filled with the remnants of desquamated cells or serous fluid.

Rathke's pocket cyst develops deep in the brain and in most cases does not pose a serious danger
CCR is a fairly widespread pathology of the hypothalamic-pituitary region of the brain, which is second only to pituitary adenomas in frequency. At autopsy, CCR is detected in 13-33% of cases. The incidence of women is twice as high as that of men.
The reasons
The Rathke pocket, or pituitary passage, is the anatomical structure formed at an early stage of embryonic development, from which the anterior, posterior part of the pituitary gland and the funnel are subsequently formed. Normally, as the fetus develops, the pocket becomes obliterated (overgrown). But sometimes it remains in the form of a small gap or cysts filled with colloidal contents, which are more pronounced in children than in adults. The exact reasons why this happens have not been established. Presumably, a genetic factor plays a role.
Symptoms
In most cases, CRCs are completely asymptomatic and are detected by chance during autopsy. Clinical signs of the disease appear only when the neoplasm reaches a significant size and compression of the pituitary gland, chiasm of the optic nerves or structures of the cavernous sinus begins. This leads to the appearance of the following symptoms in the patient:
- persistent headaches;
- visual impairment.
Often, clinically significant CRCs are accompanied by hormonal disorders, presented in the table:
| Hormonal disturbance | Signs |
| Hypopituitarism |
Pathology is associated with a significant decrease in the production of hormones by the adenohypophysis (anterior pituitary gland). This leads to disruption of the proper functioning of the ovaries, adrenal glands and thyroid gland. Usually, patients go to the doctor with the following complaints: · Decreased elasticity and pallor of the skin; Hair loss in the armpit and groin area; · Atrophy of the mammary glands and dysmenorrhea in women; Hypotension; · amyotrophy. In children, dysfunction of the thyroid gland can lead to delayed psychomotor development. |
| Hyperprolactinemia |
A pathological condition, the development of which is associated with an increased level of prolactin in the blood. Its symptoms are: • menstrual irregularities, infertility, decreased libido; Hypermastia, galactorrhea; · Hirsutism; · Increased blood clotting; · Psychoemotional disorders (sleep disturbances, emotional lability, increased fatigue). |
| Lack of antidiuretic hormone (ADH) | With insufficient secretion of the anterior pituitary gland of ADH, the patient develops diabetes insipidus (diabetes insipidus). Its main symptoms are a strong feeling of thirst (polydipsia) and polyuria (the release of a significant volume of urine, often up to 15 liters per day) |
Often, the first clinical manifestations of Rathke's pocket cyst appear with the development of pituitary apoplexy or hemorrhage into the formation cavity. The symptoms of these conditions are:
- nausea, repeated vomiting;
- visual impairment;
- persistent intense headaches.
Complications
The main complication of CRC is its transformation into a benign tumor formed by epithelial cells (craniopharyngoma).
Diagnostics
If CCR is suspected, the patient should be examined by a neurologist and ophthalmologist in order to identify symptoms characteristic of compression of brain structures. Considering that with a cyst of Rathke's pocket, patients may develop hormonal disorders, an endocrinologist's consultation with a mandatory laboratory blood test for the level of pituitary hormones is indicated.
CRC must be differentiated from a number of other diseases:
- arachnoid cysts;
- epidermal cysts;
- cystic pituitary adenomas.
For this purpose, carry out:
- computed (CT) and / or magnetic resonance (MRI) tomography;
- angiography of cerebral vessels.
Since the tactics of managing patients with CRC and prolactinomas (adenomas) are different, in order to avoid possible diagnostic errors, a repeated radiological examination is necessary, which is better carried out in a specialized medical center. According to medical statistics, during the repeated examination of patients with a diagnosis of "prolactinoma", 20% of them revealed non-neoplastic formations, including Rathke's pocket cyst.
Treatment
Small cysts in Rathke's pocket with an asymptomatic course are not dangerous and do not require any treatment. With the growth of education and the appearance of signs of compression of the brain structures, surgical removal is indicated. Currently, it is most often performed by endoscopic endonasal transphenoidal access.
The essence of the intervention: the endoscope is advanced through the nasal cavity under computer visual control to the area of the Turkish saddle. Then, using special manipulators, the neurosurgeon removes the cystic formation and directs the resulting tissues for histological examination.
Consequences and forecast
After surgical removal of the CCR in patients, headaches decrease, visual function is restored, and the level of prolactin in the blood returns to normal. With hypopituitarism, the restoration of the hormonal function of the pituitary gland is observed in no more than half of the cases.
The likelihood of a relapse of the disease is quite high. The tumor can develop again in the period from a month to 25 years after the operation, but most often the time interval is 4-5 years. Therefore, after removal of the CCR, patients should be under the supervision of a neurologist or neurosurgeon for at least five years.
Video
We offer for viewing a video on the topic of the article.

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
Found a mistake in the text? Select it and press Ctrl + Enter.