Liver abscess
The content of the article:
- What it is
- Causes of liver abscess
- Liver abscess symptoms
- Diagnostic methods
-
Liver abscess treatment
- Drug treatment
- Surgery
- Additional methods
- Prognosis and possible complications
- Video
A liver abscess is a purulent-destructive formation that is limited from the surrounding tissues by means of a capsule. The disease can occur for various reasons: impaired patency of the bile ducts, bowel disease, purulent processes of other localization, liver injury. Men get sick more often than women, the average age of the onset of pathology is 40 years. Treatment should be carried out in a hospital setting, antibiotics and minimally invasive procedures are prescribed.

Liver abscess is manifested by pain in the right hypochondrium and a general deterioration in well-being, inpatient treatment
What it is
An abscess is a disease characterized by the formation of a limited cavity filled with purulent contents. A purulent focus can form anywhere - both in the right and left lobes of the liver. Abscesses can be single or multiple, the sizes can also vary - from 1 mm to 10 cm or more.
Causes of liver abscess
The occurrence of an abscess is associated with the ingress of microorganisms into the liver - bacteria and parasites. The most common causative agents of the disease are:
- colibacillus;
- klebsiella;
- streptococci;
- Staphylococcus aureus;
- amoeba;
- bacteroids;
- proteas.
As a rule, an abscess develops as a complication of other diseases. Microorganisms can enter the liver in different ways: through the bile ducts, with the flow of blood and lymph, and direct spread of infection from nearby organs is also possible.
Depending on the way the infection spreads, several types of the disease are distinguished - cholangiogenic, hematogenous, intestinal, traumatic, cryptogenic.
| View | Explanation |
| Cholangiogenic |
The most common type of pathology. The infection spreads through the biliary tract. An abscess is formed against the background of the following diseases: • cholecystitis (inflammation of the gallbladder); Cholangitis (inflammation of the bile ducts); Gallstone disease (gallstone disease); · Violation of the patency of the bile ducts - cicatricial strictures, stenosis, atresia; · Malignant and benign neoplasms. |
| Hematogenous | The infection spreads through the bloodstream through the portal or hepatic vein. The cause is septic conditions (general blood poisoning). |
| Intestinal |
The cause of the formation of a purulent focus in the liver is inflammatory bowel diseases: · Destructive forms of appendicitis; Duodenitis; Colitis; · Diverticulitis. |
| Traumatic | The disease can develop after suffering a blunt abdominal trauma. As a result, a zone of necrosis is formed, which is initially filled with blood and bile, and when the bacterial flora is attached, with pus. |
| Cryptogenic | In the case when the cause of the formation of an abscess is unknown, we are talking about a cryptogenic abscess. The reason may lie in a latent disease. |
Liver abscess symptoms
In most cases, symptoms develop gradually. The severity of manifestations depends on the size of the abscess and the primary disease. Severity or pain in the hypochondrium, dyspepsia, yellowness of the skin, fever and other symptoms of intoxication may develop.
| Symptom group | Description |
| Pain in the hypochondrium |
Severity or pain in the right hypochondrium often appears with superficial formations that press on the liver capsule. The following symptoms are characteristic of the pain syndrome: The pain increases when lying on the left side; · Is dull, squeezing character; · Present constantly, little depends on food intake. |
| Dyspepsia |
The disease is often accompanied by the development of dyspeptic symptoms: • nausea; • deterioration in appetite; Diarrhea. Against this background, body weight can be significantly reduced. |
| Yellowness | Jaundice appears in the late stage of the disease due to compression of the bile ducts. First, the mucous membranes turn yellow, and then the skin. |
| Increased body temperature | An increase in body temperature indicates an active inflammatory process in the body. Fever is characteristic (an increase in body temperature above 38 ° C). |
| Intoxication syndrome |
The presence of a focus of purulent inflammation leads to intoxication of the body, which is accompanied by the following symptoms: General weakness, lethargy, increased fatigue; Chills; · headache; • impaired consciousness, daytime sleepiness. |
Diagnostic methods
What they pay attention to when diagnosing:
- symptoms suggesting liver damage;
- signs of intoxication;
- the presence of an underlying disease that led to the formation of an abscess;
- physical examination data: an increase in the size of the liver, local pain;
- data from additional research methods - laboratory and instrumental.
It is difficult to diagnose only on the basis of the clinical picture; additional tests are required.
| Method | Results, research features |
| Complete blood count (CBC) | In the KLA, signs of inflammation are revealed: an increase in the level of leukocytes due to neutrophils, the appearance of young forms of leukocytes, an acceleration of ESR. |
| Blood chemistry | In the biochemical analysis of blood, signs are revealed that indicate liver damage: an increase in the level of liver enzymes (ALT, AST), an increase in the level of bilirubin (mainly direct). |
| Bacteriological examination of the contents | To determine the pathogen and its sensitivity to antibiotics, bacteriological inoculation of the contents of the abscess is performed. |
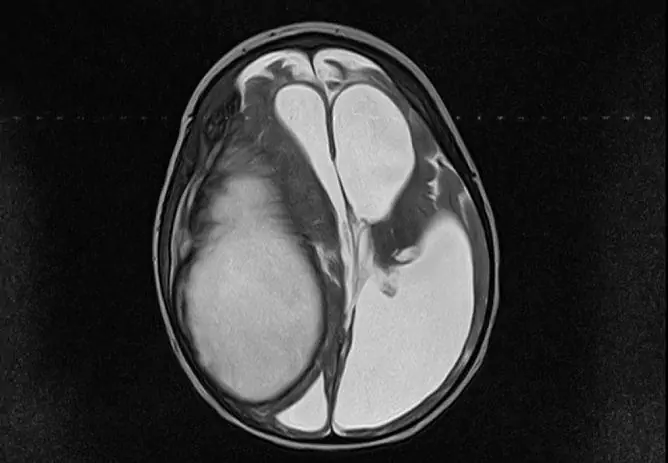
| Ultrasound examination (ultrasound) | One of the main diagnostic methods. With its help, you can find a cavity in the liver that is filled with liquid contents. The size of the abscess and its localization are determined. Abscesses larger than 1 cm are available for imaging. |
| Plain X-ray of the abdominal organs | On the X-ray, you can see a focus of enlightenment in the liver with a horizontal fluid level. |
| Computed tomography (CT) | A more informative and specific research method is carried out in cases where ultrasound data is insufficient. The exact size of the formation, its localization and location relative to the parenchyma (superficial, deep), the nature of the contents, the thickness of the capsule are determined. |
Liver abscess treatment
The tactics of therapy mainly depend on the size and number of abscesses. With a single formation or small multiples, conservative treatment is used. If the size of the cavity is more than 3 cm (with multiple more than 1.5 cm), surgical procedures are performed.

Treatment tactics depend on the results of ultrasound and plain radiography (and in some cases - CT)
Drug treatment
Conservative treatment consists in the use of antibacterial agents. At the beginning of treatment, antibiotics are selected empirically, after receiving the results of bacterial culture, the drug can be changed.
What antibiotics can be prescribed for the treatment of pathology:
- Metronidazole is an antibacterial and antiprotozoal drug. It is prescribed for suspicion of anaerobic or amoebic etiology.
- 3rd generation cephalosporins (Ceftriaxone) are broad-spectrum drugs that can be prescribed for the treatment of both anaerobic and aerobic infections.
- Penicillins and aminoglycosides - Used to treat aerobic infections.
Antibiotics are used for a long time, from 3 weeks or more.
Surgery
If conservative treatment is ineffective or if the abscess is large, surgical methods of treatment are used. All of them consist in evacuating pus from the cavity, flushing it or draining it.
What options for surgical treatment can be applied:
- Percutaneous puncture and drainage is the least invasive method. Evacuation of pus by puncturing an abscess through the skin or installing a drain. The procedure is performed under ultrasound control. Used for small abscesses.
- Laparatomy is the most radical and most invasive treatment. It is used when the abscess is inaccessible and when it is large.
- With cholangiogenic liver abscess, an additional operation is often required, which is aimed at restoring the patency of the biliary tract.
Additional methods
Additional treatment includes active bed rest, drinking plenty of fluids, and diet. Shown fractional meals 5-6 times a day in small portions. The diet should have a sufficient amount of vitamins and proteins, for this you need to eat more vegetables and fruits, fish and seafood, meat, cottage cheese.
Prognosis and possible complications
With the timely start of treatment, the prognosis is favorable, the disease ends with a complete recovery. Late start of treatment and the presence of concomitant pathology often lead to the development of complications:
- generalization of infection (sepsis);
- breakthrough of pus into the abdominal cavity or adjacent organs;
- bleeding.
With the development of complications, a large size of an abscess or multiple lesions, the disease can be fatal.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.