- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Bleeding with menopause
The content of the article:
- The concept of the climacteric period
- Causes of bleeding with menopause
- Dependence of the nature of bleeding on the period of menopause
- Therapeutic tactics
- Treatment of bleeding with menopause
- Video
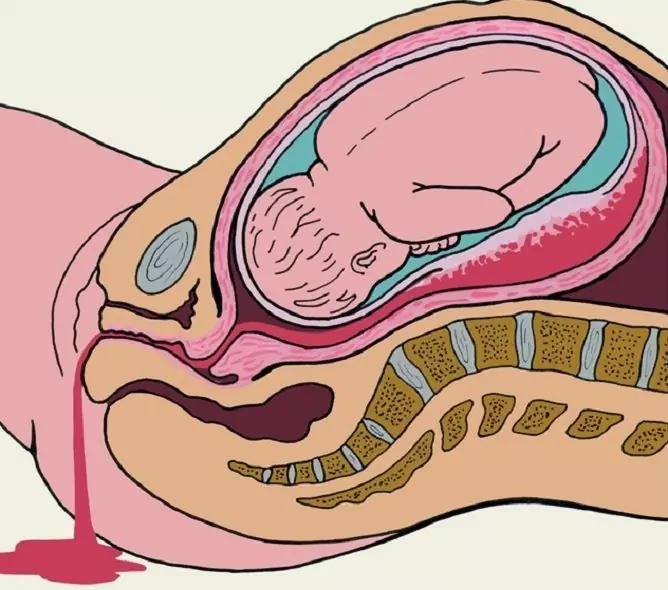
The period in a woman's life, characterized by the extinction of the function of the gonads due to age-related changes, is called menopause, or menopause. Involutive changes in the ovaries, which normally occur from 45 to 55 years of age, are often accompanied by profuse bleeding from the vagina. Bleeding during menopause can be associated with both hormonal imbalance and organic causes. Treatment of pathology should be preceded by examination and separate therapeutic and diagnostic curettage. The latter allows the doctor to exclude malignant neoplasms of the genital area and conduct etiologically justified therapy.

Bleeding during menopause is always a reason to see a doctor
The concept of the climacteric period
In order to understand the mechanism of development of bleeding during menopause, it is necessary to have an idea of the stages of the menopause (menopause).
| Stage | Characteristic |
| Premenopause | It is characterized by a gradual extinction of the hormonal function of the ovaries, which leads to an increase in the variability and duration of the menstrual cycle, a decrease in the ability to bear children, and the appearance of the first vegetative-vascular manifestations. It starts from the moment the first symptoms appear and lasts until the last independent menstruation. The duration of the period, as well as the severity of clinical manifestations, is very individual. In most women, it begins between the ages of 45 and 46 and lasts from 1 to 4 years. |
| Menopause |
This concept is customary to designate the last independent menstruation. The date is determined after a lapse of time, after the absence of menstrual flow for a year. The average age of onset is about 50 years. The cessation of menstruation before the turn of 40 years is considered to be premature menopause, up to 43-44 years - early. |
| Postmenopause | It begins after the last spontaneous menstrual bleeding and continues until the complete involution of the gonads. It is often accompanied by a disruption of the condition and clear functioning of organs that have prescriptions for female sex hormones - estrogens. Against the background of hormonal deficiency, there are age-related changes in the genitourinary organs, skin, mammary glands, bones. |
Causes of bleeding with menopause
The main causes of climacteric bleeding are presented in the table.
| Etiological factor | Characteristic |
| Hormonal imbalance |
The extinction of the functional activity of the female gonads, leading to a decrease in the synthesis of hormones, disrupts the cyclic work of the hypothalamic-pituitary-ovarian system. The consequence of this is a violation of the process of maturation of follicles, the absence of a full-fledged corpus luteum, insufficiency of the second phase of the menstrual cycle. In conditions of a lack of progesterone, there is a relative excess of estrogen, which provokes the proliferation of the mucous membrane of the uterus - the endometrium. Thickening, an increase in the volume of the latter is called hyperplasia and leads to abundant discharge of blood from the genitals during the period of hormonal changes. |
| Organic diseases |
The pathology of the genital area of an organic nature, leading to bloody discharge of varying intensity, includes uterine fibroids, internal endometriosis, or adenomyosis, hormone-producing ovarian tumors (granulosa cell or granulosa-teccellular). These diseases are often combined with hyperplasia of the mucous membrane of the uterus, which aggravates the resulting bleeding. Hormone-active formations of the ovaries, in addition to the fact that they can provoke abundant bloody discharge from the uterus, have a high risk of malignancy. The cause of the discharge of blood from the genitals can be diseases of the vagina of an atrophic nature, developing against the background of age-related estrogen deficiency. Lack of hormones in the body leads to thinning of the mucous membrane of the vagina and the vaginal part of the cervix, which, as a result, are easily injured, ulcerated and infected. |
|
Malignant neoplasms |
Bleeding arises from the vessels of the cervix or uterine body eroded by a malignant tumor. Its intensity depends on the depth of invasion and the caliber of the vessel, the integrity of which is violated. |
| Extragenital pathology | The release of blood from the genital tract can occur with liver pathology (cirrhosis), thyroid gland (hypothyroidism), disorders of the blood coagulation system (coagulopathy). It should be noted that the listed diseases very rarely act as an etiological factor, but such a possibility exists. |
Dependence of the nature of bleeding on the period of menopause
For each stage of menopause, certain etiological factors are characteristic that determine the occurrence of bloody discharge.
| Menopause phase | Characteristics |
| Premenopause | The main cause of bleeding at the initial stages of ovarian involution is hormonal imbalance. Menses become irregular and may be absent for several months and then return. For some women, they become less scarce, but more often the opposite. Perhaps a shortening of the menstrual cycle or the appearance of abundant, prolonged discharge during the intermenstrual period. |
| Postmenopause |
If menstruation is absent for more than 12 months, then the appearance of any kind of bloody discharge (pink, red, brown) from the genitals should be considered, first of all, as a formidable sign of a malignant neoplasm. It is this pathology that is the most common cause of bleeding after menopause. Minor discharge can be caused by estrogen deficiency and thinning of the vaginal mucosa. They often occur or worsen after vaginal procedures (douching) or sexual contact when additional trauma occurs. |
Therapeutic tactics
Treatment for menopausal bleeding depends on the cause. To establish it, the doctor conducts:
- patient survey;
- gynecological examination;
- ultrasound examination of the pelvic organs;
- laboratory examination (clinical, biochemical blood tests, determination of the level of hormones, tumor markers in the blood plasma).
The listed methods suggest the presence of a certain problem, but the final diagnosis is established only after histological examination. As for the vagina and cervix, in most cases, the gynecologist can take tissue samples during the examination. Pathology, localized in the uterus, requires separate therapeutic and diagnostic curettage or hysteroscopy.
| Method | Characteristic |
| Fractional (separate) therapeutic and diagnostic curettage |
Separate and sequential scraping of the mucous membrane of the cervical canal and the uterine cavity is performed with a special instrument - a curette. Scrapings are collected in separate containers filled with a special fixing solution and sent to the laboratory for further histological examination. Their study allows you to determine the nature of the process, the most accurate assessment of the functional activity of the ovaries. Curettage in the presence of hyperplasia, polyps of the inner lining of the cervical canal and the uterus acts as a therapeutic procedure. Removal of overgrown mucous membranes - surgical curettage, allows not only to collect material for research, but also in most cases to stop excessive spotting. In addition, during curettage curettage, it is possible to assume or confirm the presence of intrauterine pathology (submucosal myomatous nodes). |
| Hysteroscopy | The method allows you to study the cervical canal and the uterine cavity using an optical device - a hysteroscope. In addition, it makes it possible to take tissue samples for histology, remove polyps and submucous (submucous) myomatous nodes. |
With an abundant discharge of blood from the genitals during the period of age-related hormonal changes, accompanied by metabolic and endocrine disorders and physiological immunosuppression (decreased immunity), the specialist should be vigilant against malignant tumors.
Treatment of bleeding with menopause
When a malignant formation is detected, treatment is carried out by a gynecologist-oncologist in a specialized institution. The volume and direction of therapy are determined by the degree of tumor invasion, the presence of a process in regional lymph nodes, and the existence of distant metastases.
If large uterine fibroids, myomatous nodes of submucous localization, a combination of fibroids with internal endometriosis are found, surgical treatment is indicated: supravaginal amputation of the uterus, extirpation of the uterus (removal of the uterus and cervix). These operations can be done with and without the removal of the appendages (fallopian tubes and ovaries). The amount of surgery depends on many factors (age of the patient, ovarian condition) and is determined individually.

Treatment for menopause bleeding depends on what causes the bleeding
In the absence of organic pathology and the dysfunctional nature of bleeding, separate diagnostic curettage performs the function of surgical hemostasis: the discharge stops or significantly decreases. Further tactics are determined by the result of histological examination. Comprehensive treatment is aimed at preventing relapse.
| Therapeutic direction | Events |
| Restoring the normal functioning of the central nervous system | Elimination of emotional and physical strain, psychotherapeutic sessions, physiotherapy, herbal preparations (Remens, Klimadinon, Alora, etc.) |
| Hormone therapy | Most often, gestagens are used both in tablets (Norkolut, Duphaston, Primolut-Nor, Micronor) and in solution (17-hydroxyprogesterone capronate, Depo-Provera). They inhibit the proliferative activity of the endometrium, cause atrophic changes in the epithelium. The dosage and regimen of administration depend on the age of the patient and the nature of pathological changes in the uterine mucosa: up to 47 years, it is possible to preserve menstruation, after - the treatment is aimed at suppressing the function of the ovaries. |
| Symptomatic therapy | Vitamin therapy (vitamins K, C, P, E, group B), in the presence of anemia - iron preparations (Sorbifer, Totema, Maltofer, etc.) |
For successful treatment, it is necessary to monitor weight and control blood pressure. All therapeutic measures should be carried out under the supervision of a physician.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
Found a mistake in the text? Select it and press Ctrl + Enter.