- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Pharyngitis in children
The content of the article:
- Causes and risk factors
- Forms of the disease
- Symptoms
- Diagnostics
- Pharyngitis treatment in children
- Possible complications and consequences
- Forecast
- Prevention
Pharyngitis in children is an acute or chronic disease characterized by an isolated inflammation of the mucous membrane of the pharyngeal cavity (total or one of its parts) without involving the lymphoid tissue of the tonsils in the pathological process.

Symptoms of acute pharyngitis
The pharynx is an organ belonging to the respiratory and digestive systems, which is reflected in the symptoms of the disease during its inflammation. It is a structure from 10 to 12 cm long, communicating with the nasal cavity (the corresponding section is called the "nasopharynx"), oral (oropharynx) and larynx (hypopharynx).
The inflammatory process can develop in any one part of the pharynx, which is quite rare. Much more often, pharyngitis in children is diffuse, migrating from the nasopharynx and spreading to the underlying structures.
Chronic sluggish inflammatory process occurs in pediatric practice much less frequently than acute pharyngitis. Most cases of acute pharyngitis, which in children almost always occurs with the involvement of neighboring ENT organs, is more often combined with rhinitis or tonsillitis. In these cases, rhinopharyngitis develops, when inflammatory changes affect not only the pharyngeal cavity, but also the nasal mucosa or tonsillopharyngitis - involvement in the pathological process along with the pharyngeal mucosa of the palatine tonsils.
Acute pharyngitis in children of primary school and preschool ages occurs up to 4-6 times a year, and in those who are often sick it reaches 8 or more episodes annually. At an older age, the incidence decreases to 1-4 cases per year.
Causes and risk factors
In children, pharyngitis in the overwhelming majority of cases (according to some reports - in 80-90%) is the first sign of acute respiratory infections, as an independent disease is much less common.
Pharyngitis in children can be provoked by viral (8-9 out of 10 cases in pediatric practice) or bacterial agents. In addition to pathogenic microorganisms, various adverse physical and chemical influences can cause pharyngitis in children.
Viruses that most often provoke pharyngitis in children:
- rhinoviruses;
- coronaviruses;
- respiratory syncytial virus;
- adenoviruses (most common between 6 months and 3 years of age);
- influenza and parainfluenza viruses;
- enteroviruses (Coxsackie A and B, ECHO);
- picornaviruses;
- reoviruses; and etc.
There is a high susceptibility to infection with the respiratory syncytial virus in young children, especially in the first half of life; in adolescents and adult patients, it is of little significance as a causative factor of pharyngitis.

Most pharyngitis is caused by viruses
In approximately 30-40% of cases (according to other sources - up to 80%), acute pharyngitis in children is provoked by a rhinovirus, since receptors of intercellular adhesion molecules to this virus are located on the mucous membrane of the nasopharyngeal cavity, which is the entrance gate for infection in this case. The opinion about the immunity acquired after the transferred pharyngitis in children is erroneous, since only for rhinoviruses about 110 serotypes (varieties) are determined.
In addition to viruses, the following pathogens are the cause of pharyngitis in children in about 10% of cases:
- β-hemolytic streptococcus of group A (more than a third of cases of acute pharyngitis in children), C and G (much less often);
- anaerobic microorganisms;
- corynebacteria;
- fusobacteria;
- yersinia;
- neisseria;
- mycoplasma;
- chlamydia;
- mushrooms of the genus Candida; etc.
In children under 5-7 years old, the microflora of the upper respiratory tract is in the process of formation. A sharp change in the social environment and, as a result, a change in the microbial biocenosis can provoke the activation of opportunistic microorganisms and the development of acute or chronic pharyngitis.
In addition to pathogenic microorganisms, the following environmental factors can be the cause of pharyngitis in children:
- mechanical trauma to the pharyngeal mucosa;
- taking extremely hot or cold food, liquids, steam;
- exposure to ionizing radiation;
- inhalation of aggressive vapors of volatile substances;
- exposure to dust, aerosols;
- contact with allergens;
- the effect of acids and alkalis on the mucous membrane of the pharynx; etc.
Risk factors for developing pharyngitis in children:
- anatomical prerequisites (age-related narrowness of the nasal passages and the pharyngeal cavity, insufficient development of the elastic tissue of the respiratory tract, under-formed local microflora, etc.);
- delayed maturation of local immunity;
- unfavorable living conditions;
- unsatisfactory ecological situation;
- the presence of older brothers or sisters in the family;
- second hand smoke;
- the presence of an allergic predisposition;
- foreign chemically active impurities in drinking water, air, food;
- chronic infectious diseases of the ENT organs and other organs and systems (bronchial asthma, diabetes mellitus, etc.);
- general hypothermia;
- violation of nasal breathing (adenoids);
- being in places where a large number of children congregate (nurseries, kindergartens, schools, summer camps, etc.).
Forms of the disease
Depending on the intensity of the painful manifestations, pharyngitis in children can be acute or chronic (the latter is practically not recorded until 3 years old).
Forms of acute pharyngitis:
- bacterial;
- viral;
- mycotic (fungal);
- allergic;
- traumatic;
- provoked by aggressive physical and chemical factors of the external environment.
Forms of chronic pharyngitis:
- simple or catarrhal;
- hypertrophic (granular);
- atrophic;
- mixed form.

Types of chronic pharyngitis
For catarrhal pharyngitis in children, hyperemia and slight edema of the mucous membrane, the presence of a transparent viscous secretion on the posterior pharyngeal wall, and an increase in individual lymphoid follicles are characteristic.
In the atrophic form of chronic pharyngitis, the mucous membrane is pale, thinned, often looks like a varnished (with a characteristic shine), there is an injection of blood vessels, traces of dried secretions.
The hypertrophic form is characterized by significant swelling, looseness and redness of the pharyngeal mucosa with punctate hemorrhages, on the surface of which hyperemic, enlarged follicles are randomly scattered; along the back wall of the pharynx, there are streaks of thick vitreous or mucopurulent mucus.
Symptoms
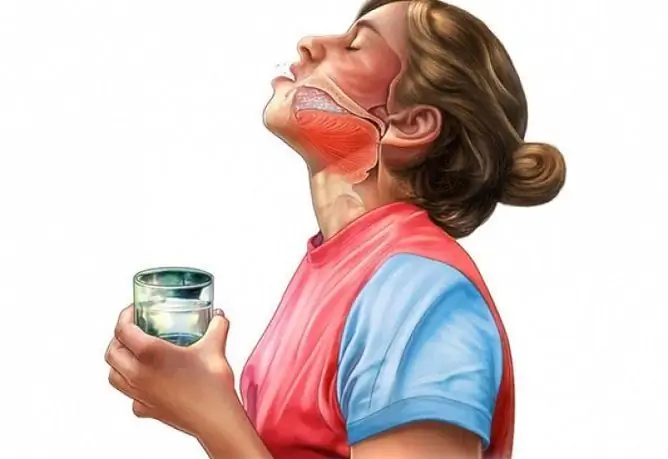
The main symptom of pharyngitis in children is pain (due to the saturation of the mucous membrane with nerve endings). The painful sensations are most intense with the so-called empty throat (when swallowing saliva) or immediately after the start of drinking, as you continue to drink the liquid, the pain sensations decrease significantly. The pain can radiate to the ear, lower jaw, neck.
Other symptoms of pharyngitis in children:
- perspiration, dryness, burning sensation in the throat;
- coughing that is reduced by swallowing saliva or drinking fluids;
- feeling of a lump in the throat;
- rawness;
- in young children, a general deterioration in well-being is expressed, accompanied by irritable weakness: restless behavior, tearfulness, refusal to eat and drink, sleep disturbance (daytime sleepiness along with intermittent superficial night sleep).
The disease in children begins, as a rule, acutely, accompanied by an increase in body temperature, intoxication syndrome (headache, general weakness, muscle pain, drowsiness). There is an increase in regional lymph nodes, their soreness.

The main symptom of pharyngitis in children is pain when swallowing saliva
In chronic pharyngitis, the symptoms of the disease are less pronounced, they bother the child during the period of exacerbations, during remission, slight discomfort may remain due to the influence of provoking factors.
In the case of rhinopharyngitis, the listed symptoms are accompanied by nasal congestion, a burning sensation or soreness in the nasal cavity, profuse mucous discharge (sometimes acquiring a mucopurulent character after a few days), sneezing. With tonsillopharyngitis, the clinical picture of the disease does not change significantly, characteristic signs are enlargement, hyperemia and swelling of the palatine tonsils, revealed during examination of the oropharyngeal cavity.
The incubation period for pharyngitis in children of viral etiology is 1-4 days. On average, an acute illness lasts from 3-5 to 7-10 days, during which the symptoms gradually subside until complete recovery occurs. With inadequate therapy or refusal to treat acute pharyngitis, the disease can transform into a chronic form.
Diagnostics
The diagnosis of pharyngitis in children is established on the basis of an assessment of complaints and an objective picture of changes in the mucous membrane of the pharynx: hyperemia of the posterior wall of the pharynx and palatine arches, inflamed lymphoid follicles, randomly scattered over the surface of the mucous membrane, while there are no signs of inflammation of the tonsils characteristic of angina.
Research methods and intended results:
- a general blood test (leukocytosis with a neutrophilic shift to the left, accelerated ESR; if the cause of acute pharyngitis is infectious mononucleosis - the initial decrease in the number of leukocytes is replaced by pronounced leukocytosis (up to 20-30 / 109 / l), up to 90% of the leukocyte formula is performed by mononuclear cells and atypical lymphocytes);
- biochemical blood test (acute phase indicators);
- sowing the material of the pharyngeal cavity on a nutrient medium in order to isolate group A β-hemolytic streptococcus;
- determination of streptococcal antigen in smears by agglutination;
- immunodiagnosis of increased titers of anti-streptococcal antibodies.

A complete blood count allows you to confirm the diagnosis of pharyngitis in children
Detection of β-hemolytic group A streptococcus in the materials of a smear from the pharyngeal cavity is carried out in order to determine the tactics of treatment, since in this case antibiotic therapy is necessary. This type of microorganism is the most pathogenic in the group of streptococci, it can cause damage to the kidneys, cardiovascular system, articular apparatus, etc., therefore, its timely detection and elimination is necessary to prevent complications.
Pharyngitis treatment in children
Treatment of pharyngitis in children has a number of features:
- safety of the drug, permission for its use in pediatric practice;
- ease of use (for example, the use of rinsing solutions in some cases is difficult, since it requires the ability to hold your breath and not swallow the drug);
- pleasant taste;
- lack of addiction to the components of the drug with frequent use.
Preference in the treatment of pharyngitis in children is given to local antimicrobial drugs in the form of sprays or tablets (lozenges) for resorption:
- chemotherapeutic antiseptics (chlorhexidine, hexetidine, benzydamine, ambazone, thymol and its derivatives, alcohols, iodine derivatives, etc.);
- phytopreparations with an antiseptic effect;
- antimicrobial agents of natural origin (lysozyme);
- beekeeping products;
- bacterial lysates.

In the treatment of pharyngitis in children, preference is given to local antiseptic agents
Herbal preparations or bee products in the treatment of pharyngitis in children must be used with caution, as they can cause allergic reactions. It is also necessary to accurately dose drugs containing chlorhexidine, due to their possible adverse effects on the liver tissue of the child.
In addition to antimicrobial therapy, it is necessary to prescribe immunocorrectors, emollients, anesthetics; antipyretics are indicated when the body temperature rises. For the period of therapy, a fortified diet, abundant drinks, and warming compresses on the front of the neck are recommended.
According to the results of numerous studies, the inexpediency of prescribing antibiotics for the non-streptococcal nature of the disease in children has been shown. The appointment of systemic antibiotics for acute pharyngitis or exacerbation of chronic is indicated only for infection caused by group A b-hemolytic streptococcus.
It has been proven that in 90% of patients, sore throat (as the main symptom of pharyngitis) disappears within 3-5 days without antibiotic therapy.
Possible complications and consequences
Complications of pharyngitis in children can be:
- tonsillopharyngitis;
- rhinopharyngitis;
- eustachitis, labyrinthitis;
- laryngitis;
- paratonsillar or pharyngeal abscess;
- paratonsillitis;
- mediastinitis;
- secondary damage to the heart, kidneys, joints.
Forecast
With timely diagnosis and complex treatment, the prognosis is favorable.
Prevention
- Prevention of hypothermia.
- Limiting contacts during epidemics of acute respiratory infections (ARI).
- Restricting a child's attendance at kindergarten, school if there are fresh symptoms of the disease.
- The wearing of masks by family members with signs of ARI.
- Restriction of travel by public transport in the spring-autumn period, when there is a peak in the incidence of ARI.
- Timely treatment of chronic diseases of the ENT organs.
- Hardening.
YouTube video related to the article:

Olesya Smolnyakova Therapy, clinical pharmacology and pharmacotherapy About the author
Education: higher, 2004 (GOU VPO "Kursk State Medical University"), specialty "General Medicine", qualification "Doctor". 2008-2012 - Postgraduate student of the Department of Clinical Pharmacology, KSMU, Candidate of Medical Sciences (2013, specialty "Pharmacology, Clinical Pharmacology"). 2014-2015 - professional retraining, specialty "Management in education", FSBEI HPE "KSU".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!