- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Thrombophlebitis
The content of the article:
- Forms of the disease
- Thrombophlebitis reasons
- Thrombophlebitis symptoms
- Diagnostics
- Thrombophlebitis treatment
- Potential consequences and complications
- Forecast
- Prevention
Thrombophlebitis is an inflammatory process that affects the inner wall of a vein and is accompanied by the formation of blood clots (thrombi). The disease is characterized by a high risk of developing potentially life-threatening complications (thrombosis of the pulmonary artery or its branches, sepsis, portal vein thrombosis), and therefore in most cases requires timely surgical treatment. The most dangerous is deep vein thrombophlebitis. According to medical statistics, in developed countries, thrombophlebitis occurs with a frequency of 1-2 cases per 1,000 adults.

Thrombophlebitis is an inflammation of the venous walls with the formation of blood clots in the lumen of the vein
Forms of the disease
Depending on the depth of the location of the vessels affected by the inflammatory process, thrombophlebitis of the superficial (subcutaneous) and deep veins is isolated.
According to the activity of inflammation and the duration of the course of the disease, thrombophlebitis can be acute, subacute and chronic. Quite often, the outcome of acute thrombophlebitis is the chronicity of the inflammatory process and its further recurrent course.
Depending on the nature of pathological changes, thrombophlebitis can be purulent and purulent.
Thrombophlebitis reasons
Absolutely any veins can be affected by thrombophlebitis, but its favorite localization is the vessels of the lower extremities. As a rule, the disease develops against the background of long-term varicose veins. In this case, the inflammatory process affects initially the superficial veins, and then, in the absence of the necessary treatment, and deep ones.
The pathological mechanism for the development of thrombophlebitis is complex, several factors are involved in it at once:
- increased blood clotting;
- violations of the composition of the blood;
- slowing down the speed of blood flow;
- damage to the walls or valve apparatus of the veins caused by any reason (trophic or endocrine disorders, diseases, trauma);
- accession of infection.
Quite often, iatrogenic factors (venesection, venipuncture) become the cause of thrombophlebitis of superficial veins.

Increased blood clotting can lead to the development of thrombophlebitis
The following conditions and diseases are predisposing factors for the development of thrombophlebitis:
- phlebeurysm;
- trauma;
- local and systemic purulent-inflammatory processes;
- postpartum period;
- post-thrombophlebitic syndrome;
- some blood diseases;
- condition after abortions and surgical interventions;
- chronic diseases of the cardiovascular system;
- oncological diseases;
- infectious diseases;
- prolonged vein catheterization or frequent venipuncture.
Thrombophlebitis symptoms
The clinical picture of thrombophlebitis is largely determined by which veins are involved in the inflammatory process.
Acute superficial thrombophlebitis most often affects the varicose veins of the lower third of the thighs and the upper third of the legs. In more than 95% of cases, the inflammation is localized in the basin of the great saphenous vein. The main signs of thrombophlebitis in this case are:
- hyperemia (redness) of the skin in the form of stripes along the affected veins;
- an increase in body temperature to subfebrile values (37.5-38 ° C);
- pulling sharp pain along the affected vein, which increases significantly with physical activity.
During palpation, the inflamed vein is defined as a dense cord, and a local increase in temperature along the course of the vein is also noted.

Hyperemia of the skin, acute pain along the affected veins - a symptom of thrombophlebitis
Acute thrombophlebitis of superficial veins under favorable conditions, i.e., timely treatment ends with recovery within 1 to 3 months. In most patients, the lumen of the affected vein is completely restored. In a minority of patients, the disease ends with obliteration (closure, closure) of the damaged blood vessel.
With an unfavorable course, the outcome of acute thrombophlebitis of superficial veins can be:
- ascending thrombophlebitis (proximal spread of infection);
- deep vein thrombophlebitis.
The likelihood of developing deep vein thrombophlebitis increases in patients with varicose veins of the lower extremities and accompanied by severe insufficiency of the valve apparatus of the vessels connecting the superficial and deep veins (perforating veins).
In about 50% of patients, deep vein thromboembolism is asymptomatic and is diagnosed only with the appearance of complications and, above all, pulmonary embolism (PE), which is a life-threatening condition. In other patients, signs of the disease may be:
- bursting pain in the affected limb;
- persistent edema of the affected limb;
- an increase in body temperature over 39 ° C (with acute thrombophlebitis);
- Pratt's symptom (the skin becomes glossy and the pattern of the saphenous veins is clearly visible on it);
- the affected limb feels colder than the healthy one.
Symptoms of pelvic vein thrombophlebitis are mild signs of peritoneal irritation, possibly the development of dynamic intestinal obstruction.
Diagnostics
The clinical picture of thrombophlebitis is determined by many factors:
- the location of the blood clot;
- the prevalence of the inflammatory process;
- severity of pathological changes in soft tissues;
- the duration of the disease.
The border of inflammation is not a dense cord, but the point of tenderness of the palpable vein.
To establish the length, localization and nature of the thrombus, the degree of patency of the thrombosed vein and the state of its wall, a number of instrumental studies are carried out:
- Doppler ultrasound of the affected veins;
- ultrasound angiography;
- rheovasography.
A laboratory blood test (general and biochemical analysis) is also carried out.

To diagnose thrombophlebitis, Doppler ultrasound of the affected veins is performed
Thrombophlebitis treatment
Conservative treatment of thrombophlebitis is indicated only with a limited pathological process that has developed in the superficial veins. In this case, patients are prescribed bed rest. The affected limb is bandaged with an elastic bandage, which allows you to fix the thrombus in the superficial vein, and give it an elevated position. A warming semi-alcoholic or oil compress, a compress with Vishnevsky ointment is applied locally.
Physiotherapeutic methods of treatment (UHF, iontophoresis with thrombolithin) have a good effect.
In order to arrest the activity of the inflammatory process, patients are prescribed non-steroidal anti-inflammatory drugs. With severe inflammation, antibiotic therapy may be necessary. Acetylsalicylic acid is prescribed as a weak anticoagulant.
Ascending thrombophlebitis of superficial veins always carries the threat of deep vein involvement in the pathological process. Therefore, the patient must be hospitalized in the vascular surgery department and assigned to bed rest with an elevated limb. In the first 48 hours after the formation of a thrombus, in order to dissolve it, the administration of fibrinolytic drugs is indicated. Also, the therapy regimen includes non-steroidal anti-inflammatory drugs, phlebotonizing drugs, anticoagulants. Topically used gels or ointments with heparin.

To dissolve the thrombus, the administration of fibrinolytic drugs is indicated
If the patient has contraindications to the appointment of anticoagulants (open form of tuberculosis, kidney and liver diseases, hemorrhagic diathesis, fresh wounds, ulcers and other conditions characterized by increased bleeding), treatment with leeches (hirudotherapy) can be an alternative.
To reduce the intensity of pain and improve collateral circulation, infiltrative novocaine blockade according to Vishnevsky is performed.
If you suspect the development of purulent thrombophlebitis and the presence of severe hyperthermia, antibacterial therapy is immediately started, which is carried out with broad-spectrum antibiotics.
Patients with thrombophlebitis are not recommended to stay in bed for a long time. As soon as the signs of inflammation begin to subside, physical activity should gradually increase. Muscle contraction improves blood flow in deep veins, thereby reducing the likelihood of thrombosis, and eliminating the inflammatory process faster. However, before activating the patient, the affected limb should be bandaged with an elastic bandage. This exercise significantly reduces the risk of developing severe thromboembolic complications.
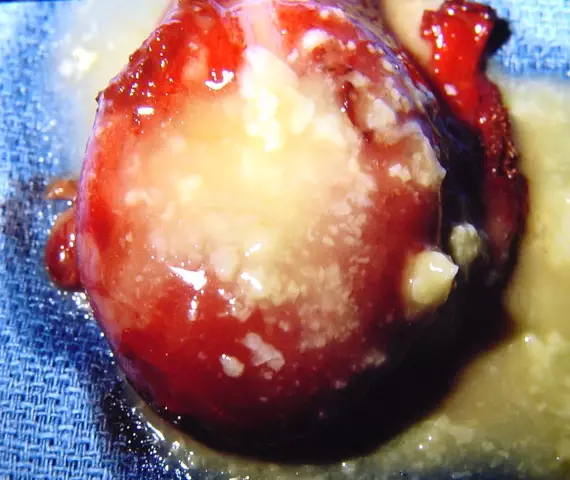
Deep vein thrombophlebitis is often accompanied by the formation of a floating thrombus. In its shape, such a blood clot resembles a tadpole and can reach a length of 20 cm, and sometimes even more. The tail of a floating thrombus under the influence of blood flow makes constant movements and at any moment is able to come off, causing the development of pulmonary embolism and almost instant death of the patient. Therefore, in the presence of such a thrombus, phlebologists insist on surgical treatment. The essence of the operation is to install a cava filter (a special filter that traps a blood clot, which will not allow it to lead to a blockage of the vessel, i.e. thromboembolism), into the inferior vena cava at a level below the renal veins.
Currently, phlebology uses various methods of surgical interventions for thrombophlebitis of superficial veins. Such operations for thrombophlebitis, especially performed in the early stages of the disease, prevent the spread of the inflammatory process from superficial veins to deep ones through the system of communicating veins, prevents the transition of the disease to a chronic recurrent form and shortens the rehabilitation period.
In acute ascending thrombophlebitis of the superficial veins of the leg, emergency surgery is indicated, since there is a high risk of deep vein thrombophlebitis.
When a thrombus is localized at the mouth of the great saphenous vein, it is removed (surgery for thrombophlebitis according to Troyanov - Trendelenburg).
After the acute inflammatory process subsides, patients with thrombophlebitis are recommended sanatorium treatment (radon, hydrogen sulfide baths, physiotherapy, exercise therapy).

If a thrombus is located in the mouth of the great saphenous vein, the Troyanov-Trendelenburg operation is performed
With an exacerbation of chronic recurrent thrombophlebitis, therapy is carried out similar to the treatment of the acute form of the disease. After the transition of the disease to the stage of remission, patients are also shown sanatorium-resort treatment.
Potential consequences and complications
Thrombophlebitis in the absence of treatment can lead to very serious complications. The most common ones are:
- streptococcal lymphangitis;
- pulmonary embolism;
- white painful phlegmas (develops as a result of reflex spasm of an artery running next to a thrombosed vein);
- blue pain phlegmas (develops against the background of complete cessation of blood flow in the femoral and iliac veins);
- purulent fusion of a blood clot.
Forecast
About 20% of untreated proximal deep vein thrombosis, that is, when the thrombus is located above the lower leg, ends with the development of pulmonary embolism, which, in turn, can be fatal. Aggressive anticoagulant therapy reduces mortality from complications of thrombophlebitis by 6-10 times.
Deep vein thromboembolism of the lower leg is almost never complicated by serious thromboembolic complications and therefore does not require anticoagulant therapy. However, blood clots from the deep venous network of the lower leg can invade the proximal veins. Therefore, if there is a danger of such penetration, patients undergo duplex ultrasound or impedance plethysmography every 3 days for 10 days. If penetration is detected, then anticoagulant therapy is immediately started.
Prevention
Prevention of thrombophlebitis development includes the following measures:
- timely diagnosis and adequate treatment of venous diseases;
- early activation of patients after operations and injuries;
- compulsory wearing of elastic compression means for varicose veins of the lower extremities;
- inclusion in the daily diet of foods rich in ascorbic acid and routine (vegetables, fruits, berries).
In chronic thrombophlebitis, to prevent the occurrence of exacerbations, patients are prescribed physiotherapeutic treatment (magnetotherapy, laser therapy, electrotherapy) every three months and taking medications with phleboprotective action.
YouTube video related to the article:

Elena Minkina Doctor anesthesiologist-resuscitator About the author
Education: graduated from the Tashkent State Medical Institute, specializing in general medicine in 1991. Repeatedly passed refresher courses.
Work experience: anesthesiologist-resuscitator of the city maternity complex, resuscitator of the hemodialysis department.
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!