- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Meningioma
The content of the article:
- Causes and predisposing factors
- Histological forms of meningioma
- Meningioma symptoms
- Diagnosis of meningioma
- Meningioma treatment
- Possible complications
- Meningioma prognosis
- Prevention
- Video
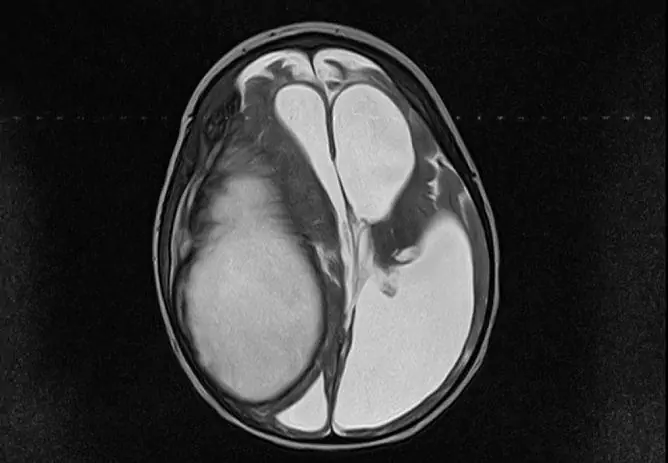
Meningioma, or arachnoid endothelioma, is a tumor arising from cells in the arachnoid (arachnoid) meninges, one of the three membranes that surround the brain and spinal cord. It is located between the surface of the brain, called the hard, and the deepest - the pia mater, and accounts for 25 to 30% of all primary tumors of the central nervous system. In most cases, meningioma is a benign neoplasm. Symptoms of the disease depend on the histological structure, localization and size of the tumor. The main treatment for meningioma is surgical removal.

Meningioma in most cases is benign, treatment consists in its removal
Causes and predisposing factors
There are a number of factors that contribute to the development of a tumor.
| Predisposing factor | Characteristic |
| Ionizing radiation | X-ray, radioactive irradiation, especially in high doses, is one of the significant etiological factors that significantly increase the likelihood of education formation. |
| Traumatic brain injury | The risk of meningioma formation and growth increases with various injuries to the bones of the skull and brain. |
| Genetic disorders |
Chromosomal abnormalities play a certain role in the development of pathology: the loss of a site or the entire 22 chromosome significantly increases the risk of arachnoid neoplasm. Arachnoid endothelioma is often found in patients with type II neurofibromatosis (NF2). It is a hereditary disease associated with mutations in the NF2 gene, which is localized on the long arm of chromosome 22. |
| Age | Most often, the pathology is detected in patients aged 35 to 70 years. The age peak of the incidence falls on 45-55 years. Tumors are rarely found in children and people over 75-80 years old. |
| Gender | The incidence in women is 2.5 times higher than in men. However, in males, a malignant type of tumor is detected 3 times more often. |
| Hormonal background | There is a connection between the tumor and the hormonal background in women: the incidence increases during menopause, the size of the meningioma may increase during pregnancy. |
The risk of developing a neoplasm becomes higher in the presence of several predisposing factors.
Histological forms of meningioma
Depending on the structure of the tissue, three types of tumor are distinguished, which characterize its malignancy.
| Grade of malignancy | Specific gravity among all meningiomas | Characteristic | Histological variant of the tumor |
| 1st degree | Up to 92-95% | Benign character, absence of atypia and invasion of surrounding tissues, slow growth, favorable prognosis, low relapse rate. | A typical variant of a tumor, including 9 subtypes: meningotelimatous, fibrous, transitional, psammomatous, angiomatous, microcystic, secretory, with an abundance of lymphocytes, metaplastic. |
| 2nd degree | Up to 4-5% | Atypical character, faster and more aggressive growth, higher recurrence rate, less favorable prognosis. | Atypical variant of a tumor, including 3 subtypes: atypical, chordoid, clear cell. |
| Grade 3 | About 1-3% |
Malignant character, aggressive growth, accompanied by invasion into surrounding tissues, a high percentage of relapses, poor prognosis. |
Malignant variant of a tumor, including 3 subtypes: anaplastic, rhabdoid, papillary. |
Meningioma symptoms
It is impossible to highlight any specific neurological symptoms characteristic of the disease. Very often, for several years, the patient does not know about the presence of an intracranial tumor, since the pathology is asymptomatic, and its first manifestation in most cases is headache. At first, it also does not differ in specific characteristics and is described as aching, dull or bursting.

Headache is the main symptom of a meningioma
The clinical manifestations of a meningioma of the brain largely depend on its localization in the cranial cavity.
| Tumor location | Typical clinical manifestations |
| Parasagital sinus, falx, or sickle of the brain (a sheet of the dura mater that extends into the longitudinal slit of the large brain between the two hemispheres) | If the growth of a tumor occurs in the frontal lobe, then higher nervous activity may suffer: thinking and memory. When located in the midsection, weakness, numbness and cramps in the lower extremities may occur. |
| Hemisphere surface | There are headaches, seizures, focal neurological manifestations due to the specific location of the neoplasm on the surface of the brain. |
| Main bone wings | Visual impairment, loss of sensitivity in the face, numbness, convulsive contractions. |
| Olfactory area |
Possible violation of the olfactory function as a result of compression of the corresponding nerve, with a significant tumor size - compression of the optic nerve, manifested by visual impairment. |
| Suprasellar region (above the diaphragm of the sella turcica) | Various disorders of visual function. |
| Posterior cranial fossa | Decrease or loss of hearing, lack of coordination, instability when walking are possible. |
| Brain ventricles | The outflow of cerebrospinal fluid may be disturbed, its excessive accumulation in the ventricular system may develop - hydrocephalus. The consequence is dizziness, headaches, changes in mental functions. |
Diagnosis of meningioma
The process of making the correct diagnosis is sometimes delayed due to the fact that the tumor in the overwhelming majority of cases is characterized by slow growth and the absence of pronounced specific manifestations. An additional factor hindering timely diagnosis is the age of the patients. Since the peak incidence occurs in the period after 50-60 years, the complaints of patients are often regarded as age-related processes accompanying natural aging.
The presence of signs of increasing mental dysfunction, persistent headache, symptoms of increased intracranial pressure should be the reason for a thorough neurological examination using modern neuroimaging methods.
| Diagnostic method | Characteristic |
| Magnetic resonance imaging (MRI) |
It is the main method for diagnosing meningiomas. The value, reliability and informational content of the method increases with contrast enhancement, which involves the intravenous administration of a special contrast agent that enhances the intensity of the magnetic resonance signal of the target tissues. The method gives a visual representation of the tumor vasculature, the degree of damage to the arteries and venous sinuses, the relationship between the meningioma and surrounding tissues. One of the characteristic features of meningioma on MRI, which is present in 65% of these tumors, is the "dural tail". This is the area of the dura mater that is involved in the process and intensively accumulates contrast agent. The method does not always allow for clear visualization of calcifications (accumulation of calcium salts in tissues) and foci of hemorrhage. |
| Computed tomography (CT) | The main role and clear advantage of CT in the diagnosis of meningioma is the detection and visualization of bone changes and calcifications in the tumor. The reliability of the method is enhanced by intravenous contrasting. |
| Positron Emission Tomography (PET) | The method is based on tracking a short-lived radioactive isotope injected into the cerebral bloodstream prior to the procedure. During scanning, data on the distribution of the isotope in the brain tissue are processed by a computer and converted into a three-dimensional image. The method is used to clarify the diagnosis in case of tumor recurrence. |
The listed methods are basic in the diagnosis of meningioma, which is most often a single node delimited from the surrounding tissues. In a much smaller percentage of cases, there is a lobular or multinodular growth pattern, infiltration of nearby structures. The size of the tumor can be both gigantic and insignificant.
Meningioma treatment
Among the many factors that determine the choice of treatment, the leading ones can be distinguished:
- the size of the meningioma;
- histological variant of the tumor;
- location of education;
- symptomatology;
- the general condition of the patient;
- the patient's ability to endure the therapeutic effect.
Patients with a diagnosis of meningioma may be offered several options for treatment tactics.
| Treatment method | Characteristic |
| Online removal | Since most arachnoid endotheliomas are benign, surgery is the main treatment. The volume of the operation and its final result largely depend on the proximity of the tumor to the functionally important brain structures and the degree of involvement of vascular formations and nerves in the process. In the case of complete removal of the meningioma, a cure is practically ensured and the likelihood of recurrence is significantly reduced. But for some meningiomas, the operation is not always possible in a radical volume. This applies to cases when the vital structures of the brain, blood vessels are affected. Although the main goal of surgery is to remove the tumor, it is equally important to improve or preserve the patient's neurological functions. In the case of a high risk of complications during radical surgery, partial removal of the tumor with subsequent dynamic observation is possible. |
| Radiation therapy |
The technique using conventional radiation therapy is practically not used to treat most types of meningiomas due to its low efficiency. It is possible to use a stereotaxic version of irradiation (focusing the radiation flux on a specific target) for the treatment of tumors localized in areas that are difficult to remove by surgery or adjacent to functionally important brain structures. The combination of stereotactic radiotherapy with an operative method also finds its application. In this case, the part of the tumor that remains after the surgical treatment is subject to radiation. This tactic reduces the risk of relapse. |
| Endovascular embolization | An intravascular X-ray surgical procedure, which consists in selectively blocking blood vessels with special emboli, which stops the flow of blood to the tumor. It is sometimes performed before surgery to remove the meningioma to reduce the risk of bleeding. For patients with absolute contraindications for surgical intervention, the method can be considered as the main treatment. |

Most meningiomas require surgical treatment
Chemotherapy is not used to treat benign meningiomas.
Not all patients need emergency surgery. Monitoring under the supervision of MRI and CT can be recommended for patients who:
- there are no neurological manifestations;
- the tumor exists for a long time and is accompanied by minor symptoms that do not have a pronounced negative effect on the quality of life;
- clinical manifestations progress very slowly, and there are restrictions on treatment, for example, related to age;
- treatment carries a high risk of complications.
Possible complications
In the absence of treatment, benign meningiomas can grow to a significant size, causing compression of brain structures and an increase in neurological symptoms. Malignant forms of meningiomas are dangerous for their infiltrative growth, metastasis to other organs, and frequent recurrence.
Meningioma prognosis
The prognosis of a typical type of meningioma with timely diagnosis and radical removal is favorable; further treatment is usually not required. Atypical, malignant, multiple variants of the tumor have a questionable and often poor prognosis. The recurrence rate within five years after complete removal is 38% for the first, and 78% for the second.
It should be noted that the forecast is influenced by many factors:
- concomitant somatic pathology (ischemic heart disease, diabetes mellitus, atherosclerosis, etc.);
- the patient's age;
- features of the tumor (localization, size, blood supply);
- anamnesis of the disease (the presence of brain surgery, radiation therapy earlier).
The dependence on age is as follows: the younger the patient, the more favorable the long-term consequences.
Prevention
There are no special measures to prevent the disease, but maintaining a healthy lifestyle is a universal method for preventing any pathology.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!