- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2024-01-15 19:51.
- Last modified 2025-11-02 20:14.
Pancreatic cyst
The content of the article:
-
Varieties of pancreatic cysts
- Congenital and acquired cystic formations
- True and false cavities
-
Pancreatic cyst symptoms
Complications
- Diagnostics
- How to treat a pancreatic cyst
- Pancreatic cyst prognosis
- Video
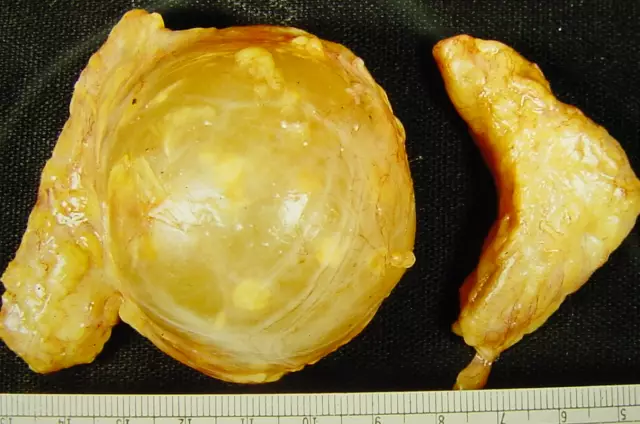
Pancreatic cyst is called a cavity formation in the tissue of the gland, consisting of a capsule and liquid contents. Pathology occurs equally often in both sexes. All age groups are affected. The cyst is congenital and acquired, true and false, benign and malignant. Therapeutic tactics and prognosis depend on its cause, mechanism of formation and size.

The type of pancreatic cyst depends on the approach to its treatment and prognosis
Varieties of pancreatic cysts
There are several classifications of pancreatic cysts, differing in the sign underlying the separation.
Congenital and acquired cystic formations
First of all, there are congenital and acquired pancreatic cavities. The former are the result of intrauterine malformations of the gland tissue and its ductal system, the latter are the result of various diseases and pathological effects on the organ.
Acquired cysts have a different formation mechanism.
| Type of acquired cyst | Formation mechanism |
| Retention | Narrowing of the lumen or persistent blockage of the excretory pancreatic ducts by tumors, stones, scar tissue after injuries, inflammatory processes. The accumulation of secretion in the duct, its stretching, the creation of a gradually increasing cavity. |
| Degeneration |
Necrosis, or death of the parenchyma of the gland as a result of traumatic injury, hemorrhage, tumor lesion, purulent fusion; the appearance of a cavity containing dead tissue and blood, which is gradually filled with pancreatic secretion. |
| Proliferative | Division and growth of cells of the epithelial lining of the capsule in benign cystadenomas, uncontrolled pathological process of cell division in malignant cystadenocarcinomas. |
| Parasitic | The vesicular larval stage of tapeworms, which occurs during infection with echinococcosis and cysticercosis: the formation of a capsule of connective tissue around the parasite surrounded by a shaft of inflamed gland tissue, foci of softening and hemorrhages in the membrane and in the cavity. |
True and false cavities
Cystic formations, depending on the characteristics of the formation of the cystic cavity and the structure of the wall, are divided into true and false, or pseudocysts. A distinctive feature of the former is the presence of a lining of epithelial cells on the inner surface of the capsule. These include:
- congenital;
- acquired retention;
- cystadenomas;
- cystadenocarcinoma.
True cavity formations make up only one fifth of all cystic neoplasms of the gland. They rarely reach significant sizes and are sometimes discovered by accident during operations carried out for another reason.
The walls of the pseudocyst do not have an epithelial cover, their formation is a sequence of the following processes:
- necrosis of the gland tissue with the opening of the acini into a closed space, mainly into the peri-pancreatic tissue, omental bursa;
- development of a dividing line around necrosis, followed by its replacement with fibrous tissue;
- the formation of a closed cavity into which the pancreatic secret is secreted.
Pseudocysts account for up to 80% of all cystic pancreatic formations and are most often a consequence of acute pancreatitis. Much less often, traumatic damage to the parenchyma is the cause of their development.
Pancreatic cyst symptoms
Clinical manifestations are determined by:
- structure;
- localization (head, body or tail of the gland);
- dimensions;
- the presence and severity of complications.
Small-volume cystic formations of the pancreas are often asymptomatic. Complaints in patients appear when the cavity formation, and this is most often a pseudocyst, reaches a large size and causes compression and / or displacement of adjacent organs. The most common symptoms include:
- pain;
- feeling of heaviness, overflow;
- nausea;
- vomiting;
- weakness;
- losing weight;
- unstable stool.
The pains are usually localized in the upper abdomen, in intensity they are dull or acute, in duration - constant or paroxysmal. Particularly strong painful sensations arise when the formation pressure on the celiac plexus. However, even with giant pseudocysts, minor symptoms are often noted, and patients complain only of a feeling of pressure and fullness in the epigastric region.
Complications
With the same frequency, there is both a slowly progressive course of the disease and a more acute one, when the pseudocyst reaches significant volumes in a short time. Both options can be complicated:
- hemorrhage into the cavity;
- suppuration;
- rupture with the development of peritonitis;
- the formation of an external or internal fistula;
- dysfunction of neighboring organs.
A large pseudocyst is able to displace the stomach, duodenum, squeeze the common bile duct, provoking the development of jaundice.
Diagnostics
Diagnosis of cystic formations of the pancreas is carried out on the basis of clinical data and additional special research methods. Laboratory indicators are nonspecific: there is a slight increase in the amount of pancreatic enzymes in blood serum and urine, sometimes a decrease in their level in the contents of the duodenum is determined.
A cyst of significant volumes can be detected already during the initial examination. An objective examination determines a tumor-like formation in the upper half of the abdomen of a round or oval shape, with clear boundaries and a flat surface. It can be palpated through the anterior abdominal wall in the epigastrium, in the navel, in the right or left hypochondrium.
When making a diagnosis, use:
- X-ray examination;
- ultrasound examination (ultrasound);
- computed tomography (CT);
- magnetic resonance imaging (MRI).
Plain radiography of the abdominal organs reveals the displacement of the stomach, transverse colon anteriorly and upward or downward from the usual position. CT and ultrasound help detect a well-defined and fluid-filled mass associated with the pancreas.
With ultrasound, benign pancreatic cysts are isolated from the gland tissue by a smooth thin wall, their cavity does not contain any partitions, and the contents are anechoic. Attention is drawn to the strengthening of the far wall contour and the effect of signal amplification in the tissues behind the formation.
If the formation has uneven walls, growths along the inner surface of the capsule, septa in the cavity, further examination is required. To exclude malignant transformation, a fine-needle biopsy of the wall and a biochemical study of its contents are performed.

Computed tomography is one of the high-precision methods used in the diagnosis of pancreatic cysts
How to treat a pancreatic cyst
The main method of treatment is surgery. Conservative tactics are used for insignificant (up to 5-6 cm) true cystic formations with thin (up to 1 mm) walls and the absence of pronounced clinical manifestations. In this case, a diet is prescribed, dynamic observation under ultrasound control.
Operational techniques are diverse.
| Operation type | Indications | Scope of surgery |
| Enucleation (husking) | Large true cystic formations accompanied by symptoms of chronic pancreatitis or complications. It is carried out only with benign formations. | Removal of the neoplasm while preserving the surrounding tissues, which are separated with a blunt instrument, if possible, by hand. |
| Distal pancreas resection | Multiple cystic formations of the body and tail of the gland | Removal of formations with part of the organ. |
| Cystojejunostomy - anastomosis (fistula, connection) between the pseudocyst and the loop of the jejunum | Giant pseudocysts of the head and body of the gland | Exposure of the anterior wall of the pseudocyst, placing a loop of the jejunum near it, turned off from the passage, creating an anastomosis. |
| Transgastric, or transgastric cystogastrostomy - the imposition of an anastomosis between the pseudocyst and the stomach | Large pseudocysts of the tail of the gland | Creation of an anastomosis between the pseudocyst and the stomach. For several days, the stomach is unloaded through a duodenal tube. The patient is fed by intravenous infusion of nutrients. |
| Transduodenal cystoduodenostomy - the imposition of an anastomosis between the pseudocyst and the duodenum | Small pseudocysts located in the head of the pancreas | Creation of an anastomosis between the cavity of the pseudocyst and the lumen of the duodenum for the outflow of the contents. |
| Marsupialization - External Drainage | Echinococcal pseudocysts or pseudocysts fused to adjacent organs, the removal of which is impossible without damaging the latter. | Dissection, emptying of the pseudocyst cavity, suturing of its walls to the parietal peritoneum and skin, allowing the cavity to gradually fill with granulations and heal. |
Which variant of surgical drainage to use is decided depending on the localization of the pseudocyst, the presence and degree of fusion with the surrounding organs. The purpose of the operation is to empty the contents of the pseudocyst into the lumen of the stomach, jejunum or duodenum. Subsequently, the cavity of the pseudocyst becomes infected and almost complete recovery in the absence of morphological and clinical signs of chronic pancreatitis.
In the absence of such a connection, it is possible to stage-by-stage hardening of the walls of the formation with a special solution, which leads to aseptic necrosis of the epithelium of the walls and subsequent overgrowth of the lumen. If there is a message with the excretory ducts, this method is not used, since there is a possibility of sclerosing solution getting into their lumen.
Pancreatic cyst prognosis
The prognosis depends on the nature of the formation, its location, size, and the presence of complications. With timely surgical treatment, smooth postoperative course, benign neoplasms, the prognosis is usually favorable.
The presence of tumor cystic neoplasms, even with their removal, may be accompanied by relapses. The prognosis, especially with the malignant nature of the formations, is doubtful. How long the patient will live depends on a number of factors.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!