- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Radiculitis: causes of development, symptoms, treatment, prevention
The content of the article:
- Causes
-
Pathogenesis
Development of a chronic process
-
Symptoms
- Lumbosacral sciatica
- Cervical sciatica
- Thoracic sciatica
- Diagnostics
-
Treatment
Surgery
- Complications
- Forecast and prevention
- Video
Radiculitis, or radiculopathy (lat.radicula - root) is a disease based on damage to the roots of the spinal cord, which develops as a result of degenerative-dystrophic changes in the spinal column and manifests itself as a pain syndrome with irradiation along the damaged nerve, a local decrease in muscle strength due to atrophy fibers, and decreased sensitivity.

Radiculitis is characterized by pain syndrome with irradiation along the damaged nerve
The disease occurs as a result of pinching the roots and pinching the bundles of nerve fibers extending from the spinal cord. Depending on the part of the spine involved in the pathological process, cervical, thoracic and lumbosacral radiculitis are distinguished.
The most often affected is the lumbosacral, less often the cervical and thoracic regions. Usually, the pathology develops acutely, accompanied by sharp intense pain arising from weight lifting, awkward movement, inflammation, and often becomes chronic.
Causes
The main etiological factor in the development of the disease is considered to be degenerative-dystrophic processes in the spinal column, such as:
- osteochondrosis;
- osteoporosis;
- deforming spondylosis;
- age-related dystrophic changes in the intervertebral discs with the loss of their elasticity and shock-absorbing function;
- destruction of the vertebrae.
Other reasons could be:
- curvature of the spine: lordosis, kyphosis, scoliosis;
- spinal anomalies: sacralization, spondylolisthesis, vertebral aplasia, etc.;
- mechanical damage to the back;
- overweight, obesity;
- spinal neoplasms;
- chronic infectious process (tuberculosis, syphilis, cerebrospinal meningitis, etc.), viral infections, tropic to nerve fibers (tick-borne encephalitis, etc.);
- metabolic disorders;
- pathology of the neuroendocrine system.
Predisposing factors are distinguished, which in themselves usually are not the cause of the disease, but in combination can provoke and accelerate the onset of symptoms.

One of the predisposing factors for the development of pathology is the prolonged presence of the body in an uncomfortable position
Trigger factors:
- hypothermia;
- psycho-emotional overstrain;
- lifting heavy objects;
- long-term presence of the body in an uncomfortable position.
Pathogenesis
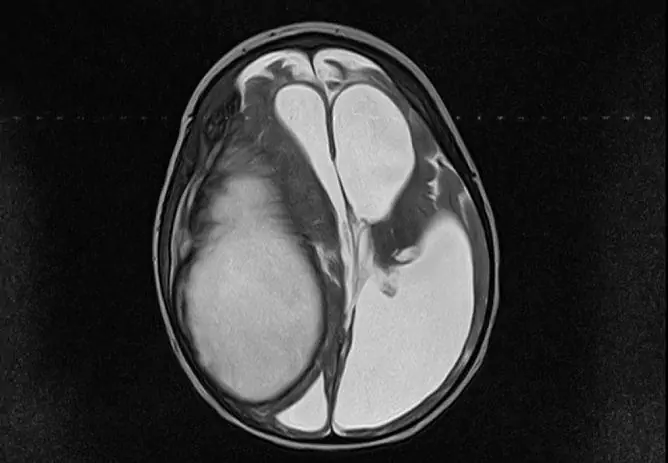
As a result of prolonged exposure to the pathological factor, the cartilaginous part of the spine - the intervertebral discs - is affected, rupture or stretching of the annulus fibrosus occurs with the extension of the gelatinous disc beyond its boundaries. Thus, an intervertebral hernia is formed.
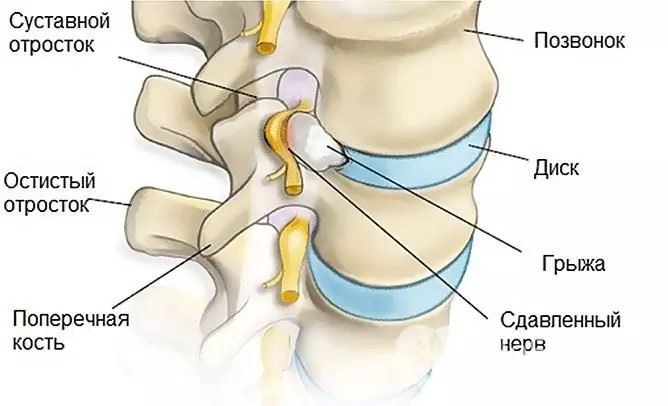
Radiculitis occurs as a result of the formation of an intervertebral hernia
The intervertebral disc loses its elasticity, the intervertebral distance is flattened, and the shock-absorbing function is lost. As a result of the reduction in space, nerve fibers extending from the spinal cord are impaired.
Then compensatory mechanisms in the osteo-ligamentous apparatus of the spine are activated again. An untimely eliminated pathological factor ultimately leads to a breakdown in compensation, the formation of marginal osteophytes - bone outgrowths, which, growing, connect the bodies of two vertebrae to each other, fixing them in a certain position.
The spine loses its flexibility, and any provoking factor (sudden movement, weight lifting, etc.) leads to pressure on the nerve roots, pinching them with intense pain and other symptoms.
Development of a chronic process
A timely untreated acute situation leads to chronic compression of the nerve roots. As a result of a long-term traumatic component, the innervation of muscles, blood vessels and other tissues is disrupted.
An additional link in pathogenesis that worsens the course of the process is muscle-tonic syndrome - a painful muscle spasm that occurs reflexively in response to irritation of the Lyushka nerve (the nerve that innervates the fibrous capsule of the intervertebral disc).
Symptoms
The disease causes sensory, motor and autonomic disorders, accompanied by the following symptoms:
- pain syndrome: the first attacks of pain occur as a result of rupture or stretching of the fibrous capsule and are diffuse in nature, resemble myositis or lumbago; the following attacks of pain are caused by radicular syndrome - compression of the nerve root;
- violation of sensitivity: due to a violation of the innervation of a certain zone, tactile, temperature and pain sensitivity may decrease, up to its complete loss;
- movement disorders: develop due to a violation of innervation, in the initial stages there may be a decrease in muscle strength, as the process aggravates, complete atrophy of muscle fibers develops in the area of action of the affected nerve.
Typical symptoms depend on the localization of the pathological process.
Lumbosacral sciatica
It can take three forms:
| The form | Symptoms |
| Lumbago | Sudden acute pain in the lumbar region is caused by weight lifting, sudden movement, hypothermia. It is characterized by increased muscle tone, limited mobility and pain on palpation in the lumbar region. Often, severe pain prevents the patient from standing or walking |
| Lumbodynia | Subacute, dull, recurrent lower back pain that worsens while sitting, walking, or any movement in the lower back |
| Sciatica | Acute or subacute low back pain radiating to one or both lower extremities, accompanied by a local increase in muscle tone, restriction of movement, alignment of the lumbar lordosis and other neuromuscular, dystrophic and vascular disorders of the lower extremities |
A specific forced position of the patient is characteristic: in a sitting position with a leg bent under him, leaning his hands on the bed, or lying down, placing a pillow from a pillow under his stomach.
Cervical sciatica
Intense one-sided neck pain develops, characterized by a specific forced position of the head - hypoplastic torticollis, local increase in muscle tone, pathological neck lordosis. The pain increases with any movement of the neck, with coughing, turning the head, sneezing.

With cervical localization of pathology, increased pain is noted with any movement of the head
The spread of pain to the proximal parts of the upper limb, chest, scapula, development of paresthesias, and decreased reflexes is possible.
Thoracic sciatica
Sensitive disorders in the limb are characteristic, motor disorders are manifested by paresis of the hand or extensors of the fingers. When sympathetic nerve fibers are involved in the process, vegetative-vascular disorders may appear, which are manifested by excessive sweating, cold snap, and swelling in the zone innervated by the nerve affected.
Often the process is accompanied by cardialgic syndrome, especially when turning, bending, flexing and extending the trunk.
Diagnostics
After the establishment of complaints, a thorough collection of anamnesis, an external examination, the doctor proceeds to determine the neurological status with the study of reflexes, sensitivity, motor activity of the limbs, autonomic disorders, and the intensity of the pain syndrome.
To verify the diagnosis and carry out differential diagnostics with other diseases, it is possible to prescribe:
- analyzes: general analysis of blood, urine, biochemical blood test;
- myelography;
- studies of cerebrospinal fluid, etc.

To clarify the diagnosis, an x-ray is prescribed
Among the instrumental studies, X-ray of one or more parts of the spinal column is shown, which allows you to identify osteochondrosis.
For a more detailed study, computed tomography or magnetic resonance imaging is prescribed. These methods allow visualizing the state of the intervertebral discs, identifying osteophytes, which indirectly indicate the osteochondral structure of the area under study.
Electromyography is a method that allows you to assess the passage of a nerve impulse along a nerve fiber, muscle response to it and the localization of a nerve impulse block.
Treatment
Basically, the treatment is conservative, aimed at reducing the intensity of the pain syndrome and restoring the nervous trophism of the affected area.

As part of complex treatment, B vitamins are used
For this purpose, appointed:
- pain relievers: diclofenac, ibuprofen, ketorolac, meloxicam, etc.; oral, rectal, injection dosage forms are prescribed, depending on the severity of the pain syndrome;
- local irritants: gels, ointments with a warming component, pepper patches, rubbing; in order to find out which drug will be most effective, you need to consult a doctor;
- B vitamins: vitamin therapy improves the trophism of the nervous tissue, high doses of vitamin B 12 have an analgesic effect.
After elimination of pain, physiotherapy, manual therapy, and physiotherapy should be included in the treatment. In extreme cases, when conventional pain relievers do not help, novocaine blockade with vitamin B 12, hormonal drugs or intravenous sedation are prescribed.
Surgery
In some cases, in order to cure the disease, surgical intervention is required, which consists in removing the intervertebral hernia.
Indications for surgical treatment:
- incessant severe pain during 3-4 months of therapy;
- paralyzing sciatica (compression of the cauda equina and dysfunction of the pelvic organs), etc.
Complications
Complications with radiculopathies are rare.
They are mainly due to local compression of large veins and arteries, a decrease in blood supply. The most common complications of radiculitis are:
- ischemia and spinal cord infarction;
- spinal epiduritis, arachnoiditis (inflammation of the membranes of the spinal cord);
- peripheral paralysis of the limbs;
- atrophic phenomena.
Forecast and prevention
Timely diagnosis and complete treatment leads to recovery, the prognosis in this case is favorable. With the development of complications, complete recovery usually does not occur, as it entails disorders of the motor or sensory sphere.
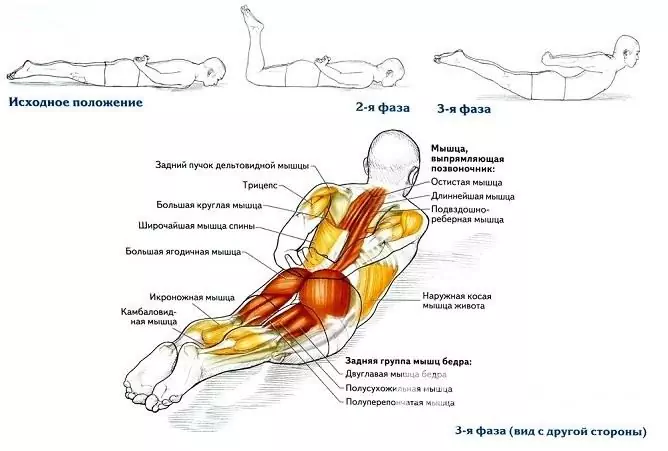
Prevention of the disease is aimed at training the back muscles, maintaining correct posture during sleep and wakefulness. You should not buy too hard mattresses, sleep on a hard surface, as they change the physiological position of the spine. It is recommended to use small pillows, semi-hard mattresses.
When lifting objects from the floor on a daily basis, you should not bend over, you need to use the hip and knee joints to perform this task, that is, perform a squat. This will reduce the stress on the spine and transfer it from the back to the stronger lower limbs.
An active lifestyle, regular non-intensive sports and gymnastics play an important role in prevention.
Video
We offer for viewing a video on the topic of the article.

Anna Kozlova Medical journalist About the author
Education: Rostov State Medical University, specialty "General Medicine".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!