- Author Rachel Wainwright [email protected].
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Intrauterine infections
The content of the article:
- Causes and risk factors
- Forms of the disease
- Symptoms
- Diagnostics
- Treatment
- Possible complications and consequences
- Forecast
- Prevention
Intrauterine infections are infectious and inflammatory diseases of the fetus and young children that occur during the antenatal (prenatal) and (or) intranatal (birth) periods with vertical infection from the mother.
It is necessary to distinguish between the concepts of "intrauterine infection" and "intrauterine infection". Infection implies the penetration of the pathogen into the child's body without unfolding the clinical picture, while intrauterine infection is a full-fledged implementation of intrauterine infection in the form of a clinical manifestation of an infectious disease.

Intrauterine infections in most cases complicate the child's health
According to the results of some studies, infection is detected in approximately 50% of term infants and 70% of premature infants. According to more "optimistic" data, every tenth fetus (child) is exposed to pathogenic agents during pregnancy and childbirth.
In 80% of cases, IUI complicates the child's health with various pathological conditions and developmental defects of varying severity. According to the autopsy results, it is determined that in every third case, perinatal infection was the main cause of the death of the newborn, accompanied or complicated the course of the underlying disease.
Long-term studies show that children in the first years of life who have undergone an intrauterine infection have weaker immune capabilities and are more susceptible to infectious and somatic diseases.
In the early 70s of the XX century, the World Health Organization proposed the name "TORCH syndrome". This abbreviation reflects the names of the most common intrauterine infections: T - toxoplasmosis (Toxoplasmosis), O - others (mycoplasma, syphilis, hepatitis, streptococci, candida, etc.) (Other), R - rubella (Rubella), C - cytomegalovirus (Cytomegalovirus), H - herpes (Herpes). If the etiological factor is not known for certain, they speak of TORCH syndrome.
Causes and risk factors
The main source of infection in IUI, as already noted, is the mother, from whom the pathogen enters the fetus during the ante- and (or) intrapartum period (vertical transmission mechanism).
The causative agents of intrauterine infection can be bacteria, fungi, protozoa, viruses. According to statistics, the first place in the structure of intrauterine infections is occupied by bacterial diseases (28%), followed by chlamydial and associated infections (21%).
Infectious agents that are the most common causes of intrauterine infection:
- rubella viruses, herpes simplex, chickenpox, hepatitis B and C, influenza, adenoviruses, enteroviruses, cytomegalovirus;
- pathogenic bacteria (Escherichia, Klebsiella, Proteus and other coliform bacteria, group B streptococci, Haemophylus influenzae, alpha-hemolytic streptococci, non-spore-forming anaerobes);
- intracellular pathogens (toxoplasma, mycoplasma, chlamydia);
- mushrooms of the genus Candida.

Herpes simplex virus is dangerous for the fetus
Risk factors for intrauterine infection:
- chronic diseases of the urogenital sphere in the mother (erosive lesion of the cervix, endocervicitis, colpitis, vulvovaginitis, ovarian cyst, urethritis, cystitis, pyelo- and glomerulonephritis, etc.);
- diseases of an infectious nature, suffered by the mother during pregnancy;
- long dry period.
Factors indirectly indicating a possible intrauterine infection:
- burdened obstetric history (spontaneous abortion, infertility, stillbirth, the birth of children with multiple malformations);
- polyhydramnios, the presence of inclusions and impurities in the amniotic fluid;
- fever, not accompanied by signs of inflammation in any organ system, developed in the mother during pregnancy or childbirth;
- the birth of a premature baby before the due date of birth;
- delayed intrauterine development of the child;
- Apgar score 0-4 points at the 1st minute of the child's life with the preservation of unsatisfactory indicators or deterioration of the assessment by the 5th minute of life;
- fever of a newborn of unknown etiology.
Forms of the disease
Depending on the duration of pregnancy, at which the infection occurred, there are:
- blastopathies - are realized during the first 14 days of pregnancy;
- embryopathies - appear in the period from 15 days of pregnancy to 8 weeks;
- fetopathies - develop after 9 weeks of pregnancy (early fetopathies - from the 76th to the 180th day of pregnancy, late fetopathies - from the 181st day of pregnancy until the moment of delivery).
An intrauterine infection that develops in the first 2 weeks of pregnancy most often leads to the death of the embryo (missed pregnancy) or the formation of severe systemic malformations similar to genetic developmental abnormalities. Spontaneous termination of pregnancy, as a rule, occurs 2-3 weeks after infection.

An intrauterine infection in the early stages most often leads to a frozen pregnancy
Since in the embryonic period all organs and systems are laid, the development of IUI at these periods will lead to the death of the embryo or, as in the previous case, to the formation of malformations of varying severity.
Fetopathies have a number of characteristics:
- congenital defects are realized only in those organs, the formation of which was not completed at the time of the birth of the child;
- infectious processes are often generalized (widespread);
- the infection is often accompanied by the development of thrombohemorrhagic syndrome;
- morphological and functional maturation of organs lags behind.
The World Health Organization (ICD-10) has proposed an extensive classification of intrauterine infections, the main forms of which are:
- congenital viral diseases;
- bacterial sepsis of the newborn;
- other congenital infectious and parasitic diseases;
- neonatal omphalitis with little or no bleeding;
- other infectious diseases specific to the perinatal period.
In this classification, there are separate sections that suggest the possibility of making a diagnosis of unspecified viral, bacterial and parasitic IUI.
Symptoms
Often, intrauterine infections do not have characteristic symptoms, therefore, nonspecific signs of an infectious and inflammatory process in a newborn can be suspected (their similarity has been noted in IUI provoked by various pathogens):
- decreased or lack of appetite;
- significant weight loss (weight loss more than 10% of the original birth weight);
- repeated weight loss, poor body weight recovery (slow gain, slight gains);
- inflammation of the skin and subcutaneous fat (sclera);
- lethargy, drowsiness, lethargy;
- grayish-pale coloration of the skin, anemic mucous membranes, possible icteric staining of the skin and mucous membranes, icterus of the sclera;
- edematous syndrome of varying severity and localization;
- respiratory disorders (shortness of breath, short-term episodes of respiratory arrest, involvement of auxiliary muscles in the act of breathing);
- dyspeptic disorders (regurgitation, including profuse, fountain, unstable stool, enlargement of the liver and spleen);
- symptoms of involvement of the cardiovascular system (tachycardia, decreased blood pressure, swelling or pastiness, cyanotic staining of the skin and mucous membranes, marbling of the skin, cold extremities);
- neurological symptoms (hyper- or hypotension, dystonia, decreased reflexes (including deterioration of the sucking reflex);
- changes in the blood formula (leukocytosis, accelerated ESR, anemia, decreased platelet count).
Signs of intrauterine infection often manifest in the first 3 days of a newborn's life.

An intrauterine infection in a newborn can be signaled by violations of cardiovascular activity
Diagnostics
When diagnosing IUI, data from anamnesis, laboratory and instrumental research methods are taken into account:
- complete blood count (leukocytosis with neutrophilic shift to the left, accelerated ESR);
- biochemical blood test (for markers of the acute phase reaction - C-reactive protein, haptoglobin, ceruloplasmin, plasminogen, alpha-1-antitrypsin, antithrombin III, C3-complement fraction, etc.);
- classical microbiological techniques (virological, bacteriological);
- polymerase chain reaction (PCR);
- direct immunofluorescence method using monoclonal antibodies;
- enzyme-linked immunosorbent assay (ELISA) with quantitative determination of specific antibodies of the IgM, IgG classes;
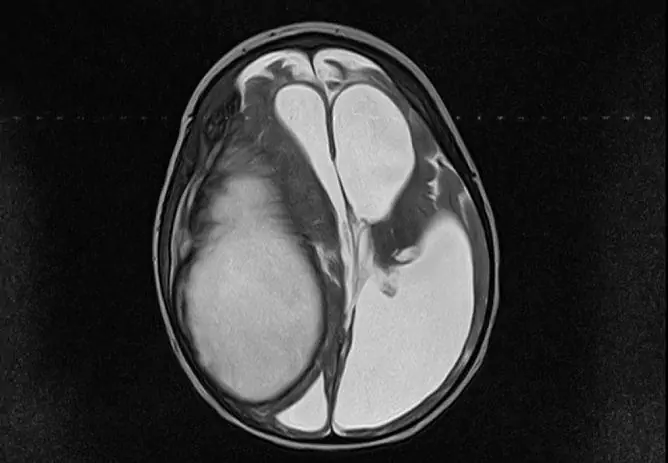
- Ultrasound of the abdominal organs, heart, brain.

A general and biochemical blood test allows you to suspect the presence of intrauterine infection
Treatment
Treatment of intrauterine infection is complex, consists of etiotropic and symptomatic components:
- antiviral, antiparasitic, antifungal, or antimicrobial drugs;
- immunomodulators;
- detoxifying agents;
- antipyretic drugs.
Possible complications and consequences
Pregnancy outcomes with IUI:
- intrauterine fetal death;
- stillbirth;
- the birth of a living viable or living non-viable (with malformations incompatible with life) a child with signs of intrauterine infection.
Complications of intrauterine infection:
- malformations of internal organs;
- secondary immunodeficiency;
- the child's lag behind peers in physical and mental development.
Forecast
With timely diagnosis and complex treatment of intrauterine infection that arose at a later date, the prognosis is generally favorable (the prognosis improves as the gestational age at which the infection occurs), although it is purely individual.
The likelihood of a favorable outcome of the disease depends on many characteristics: the virulence of the pathogen, its type, method of infection, the presence of concomitant pathology and aggravating factors on the part of the mother, the functional state of the pregnant woman's body, etc.
When IUI occurs in the early stages, the prognosis is usually poor.
Prevention
Prevention of IUI development is as follows:
- prevention of infectious diseases of the mother (sanitation of foci of chronic inflammation, timely vaccination, screening of pregnant women for the presence of TORCH infections);
- antibacterial or antiviral therapy for pregnant women with the development of acute or exacerbation of chronic infectious inflammation;
- examination of newborns from mothers of high risk groups;
- early vaccination of newborns.
YouTube video related to the article:

Olesya Smolnyakova Therapy, clinical pharmacology and pharmacotherapy About the author
Education: higher, 2004 (GOU VPO "Kursk State Medical University"), specialty "General Medicine", qualification "Doctor". 2008-2012 - Postgraduate student of the Department of Clinical Pharmacology, KSMU, Candidate of Medical Sciences (2013, specialty "Pharmacology, Clinical Pharmacology"). 2014-2015 - professional retraining, specialty "Management in education", FSBEI HPE "KSU".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!