- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
Dyskinesia
The content of the article:
- Causes and risk factors
- Forms of dyskinesia
- Dyskinesia symptoms
- Diagnostics
- Dyskinesia treatment
- Diet for dyskinesia
- Possible complications and consequences
- Forecast
- Prevention
Dyskinesia is a collective name for disorders of coordinated motor acts (usually smooth muscles of internal organs).
Dyskinesia of the esophagus is a violation of its motor function, which can lead to a slowdown in the movement of food from the pharynx into the stomach or its retrograde, i.e., reverse movement. Dyskinesia of the esophagus is a fairly common pathology, one or another of its forms is detected in about 3% of patients who undergo esophagogastroduodenoscopy. To a greater extent, dyskinesia of the esophagus affects females (approximately 79% of cases) over 30 years old.
Dyskinesia of the stomach is a functional disorder of the contractile function of the stomach, which is one of the most common gastroenterological pathologies. Dyskinesia of the stomach is most often diagnosed in young people, as well as in patients with organic or functional diseases of the central nervous system.
Dyskinesia of the biliary tract is a functional pathology of the biliary system, which is based on motor-tonic dysfunction of the gallbladder, as well as the sphincters of the bile ducts. Pathology is one of the most common disorders of the hepatobiliary system, more often it develops in women aged 20-40 years with an asthenic body type.
Intestinal dyskinesia is a common functional disorder of the intestine that affects about 20% of the general population. Most often, the pathology is diagnosed at the age of 30-40, while at a young age, intestinal dyskinesia is more susceptible to women, and after 50 years, this pathology in males and females is detected with approximately the same frequency. The first signs of intestinal dyskinesia may appear already in childhood, but more often occur after 15 years.
Causes and risk factors
The reasons for the development of primary esophageal dyskinesias include:
- congenital anomalies of the neuromuscular apparatus of the esophagus;
- chronic alcoholism;
- stressful situations;
- age-related changes.
Secondary dyskinesias of the esophagus can develop against the background of hiatal hernia, esophageal neoplasms, esophagitis, diverticula, gastric ulcer and duodenal ulcer, chronic cholecystitis, muscular dystrophy, lesions of the central and peripheral nervous system, diabetes mellitus.
Both exogenous and endogenous causes can lead to dyskinesia of the stomach. Risk factors include:
- diseases of the central nervous system;
- diseases of the gastrointestinal tract;
- cardiovascular pathology;
- rheumatic diseases;
- allergic processes;
- avitaminosis;
- inappropriate nutrition (systemic dry food, eating too quickly, the prevalence of carbohydrates, spicy and fatty foods in the diet, etc.);
- bad habits;
- stress;
- high ambient temperature (living in hot climates);
- exposure to the body of ionizing radiation;
- taking certain medications.
The etiological factors of biliary dyskinesia include:
- congenital malformations;
- endocrine disorders;
- diseases of the digestive system;
- exposure to stress;
- sexual disorders;
- helminthic invasions;
- food allergy;
- overweight.

Source: online.org
The main cause of intestinal dyskinesia is acute or chronic stress. Risk factors: genetic predisposition, acute infections of the gastrointestinal tract, neurotic character, increased anxiety.
Forms of dyskinesia
Dyskinesias of the esophagus can be primary and secondary, as well as hypomotor and hypermotor.
Depending on the type of motility disorder, gastric dyskinesia is divided into hypertensive, hypotonic and atonic forms. Depending on the etiological factor, the pathological process can be exogenous or endogenous.
Dyskinesias of the biliary tract are subdivided into primary (developing against the background of disturbances in the neurohumoral regulation of the activity of the hepatobiliary system) and secondary (due to other diseases of the gastrointestinal tract), as well as hypokinetic (atonic) and hyperkinetic (spastic).
Depending on the change in the consistency of feces, intestinal dyskinesias are classified into the following forms:
- with constipation (more than 25% of all acts of defecation occur with constipation, less than 25% with diarrhea);
- with diarrhea (more than 25% of bowel movements occur with diarrhea, less than 25% with constipation);
- mixed (defecation with both diarrhea and constipation occurs in more than 25% of cases);
- unclassified.
Depending on the etiological factor, intestinal dyskinesia is divided into stress-related, post-infectious, associated with the use of certain foods.
Dyskinesia symptoms
Hypomotor dyskinesias of the esophagus are asymptomatic in about 20% of cases. In other cases, their main signs are: belching, disorder of the act of swallowing (dysphagia), a feeling of heaviness in the epigastric region after eating, aspiration of stomach contents into the respiratory tract, inflammatory processes in the esophageal mucosa.
Hypermotor dyskinesia of the esophagus is usually manifested by difficulty in swallowing, pain behind the sternum, which can radiate to the scapula, left half of the chest and left arm. The chest pains resemble an attack of angina pectoris, however, unlike the latter, they are not associated with physical exertion, and in some cases are stopped with a sip of water. With severe spasm, the patient develops a foreign body sensation in the esophagus, which increases with excitement and / or swallowing, accompanied by a lack of air and a burning sensation behind the sternum. An increase in motor activity and tone in hypermotor dyskinesia of the esophagus is noted not only when food is swallowed, but also outside the act of swallowing.
The symptoms of esophageal dyskinesia are aggravated by alcohol abuse, smoking, frequent stress, and also when eating too hot food.
With dyskinesia of the stomach, patients develop abdominal pain without clear localization. The duration of a painful attack can be from several minutes to several weeks. The pain can be cramping, aching, pressing.
The onset of pain is usually associated not with meals, but with emotional and psychological factors. In the presence of antiperistaltic contractions and the throwing of stomach contents into the esophagus, patients complain of heartburn, sour belching. In the case of a decrease in the contractile activity of the stomach, a rotten eructation occurs. With dyskinesia of the stomach, caused by pathologies of the central nervous system, repeated vomiting is observed, which does not bring relief. Stomach dyskinesia symptoms usually subside at night.
Among the main symptoms of biliary dyskinesia are pain in the epigastrium, as well as in the area of the right hypochondrium, which radiate to the right shoulder and scapula. With hyperkinetic dyskinesia of the biliary tract, pain, as a rule, is acute, occurring during physical exertion, stress, errors in the diet. Patients with this form of pathology may experience sleep disturbances, headaches, excessive sweating, irritability, and fatigue.
Pain in hypokinetic form of biliary dyskinesia is usually constant and not intense, it can be dull, aching, accompanied by a feeling of heaviness. Patients complain of bitterness and / or dry mouth, halitosis, belching of air, decreased appetite, nausea, vomiting, flatulence, constipation, or diarrhea. With dyskinesia in children, there is an intolerance to sweet and fatty foods, the use of which is accompanied by nausea and vomiting.
With intestinal dyskinesia, flatulence occurs (worse in the evening, after a meal), diarrhea and constipation, a feeling of incomplete emptying of the intestines, pain in the abdomen, usually localized in the iliac region, which can be sharp or aching, dull.
The pain increases after eating, subsides after defecation and passing gas. There is an admixture of mucus in the stool. With constipation, semi-liquid feces come out behind dense feces. Patients with intestinal dyskinesia complain of persistent headaches, a feeling of shortness of breath, dissatisfaction with inspiration, tremors.

Source: myshared.ru
Diagnostics
Diagnosis of dyskinesias is based on data obtained during the collection of complaints and anamnesis, an objective examination, as well as instrumental and laboratory studies, the volume of which depends on the existing clinical manifestations.
If esophageal dyskinesia is suspected, esophagoscopy, esophagomanometry, daily intraesophageal pH monitoring, and radiography of the esophagus are indicated. To identify complications or concomitant diseases, a fecal occult blood test is performed.
When diagnosing gastric dyskinesia, first of all, organic pathology should be excluded. Disorders of gastric motility can be detected by electrogastrography. For the purpose of differential diagnosis, gastric fluoroscopy, esophagogastroduodenoscopy with mandatory biopsy are performed.

Source: gastroscan.ru
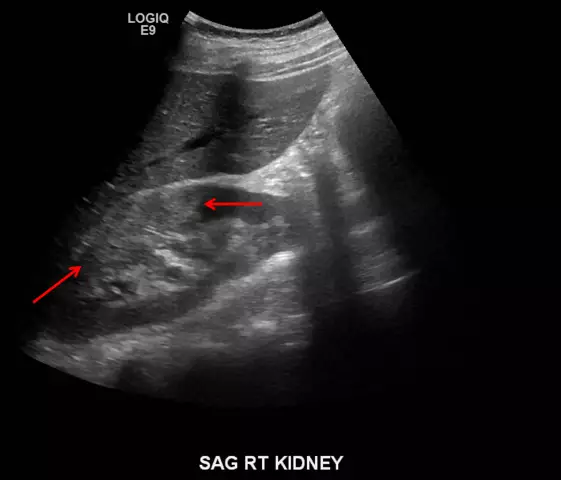
To diagnose biliary dyskinesia, duodenal intubation, X-ray, ultrasound, and, if necessary, hepatobiliary scintigraphy and magnetic resonance imaging of the liver and biliary tract are prescribed.
With dyskinesia in children, X-ray contrast studies are carried out relatively rarely and only for strict indications.
From laboratory diagnostic methods, a biochemical blood test is used (in particular, the determination of the concentration of cholesterol, high, low and very low density lipoproteins).
To diagnose intestinal dyskinesia, ultrasound of the abdominal cavity, irrigoscopy, sigmoidoscopy, colonoscopy, and general X-ray of the abdominal cavity are performed. A biochemical blood test is prescribed, a study of feces for occult blood, scraping for enterobiasis, analysis of feces for helminth eggs.
Differential diagnosis of esophageal dyskinesia is carried out with esophageal cancer, ischemic heart disease, gastroesophageal reflux disease, and achalasia of the cardia. Dyskinesia of the biliary tract is differentiated from inflammatory diseases of the gallbladder and biliary tract, neoplasms, cholelithiasis. Intestinal dyskinesia must be differentiated from infectious diseases of the digestive tract, intestinal neoplasms, endocrine disorders, and urogenital pathology.
Dyskinesia treatment
In the treatment of esophageal dyskinesia, antispasmodic and sedative drugs are used. If conservative therapy is ineffective and complications develop, surgical treatment may be required.
Treatment of gastric dyskinesia is also carried out with the use of sedatives, and in case of violations of the secretory function of the stomach, replacement therapy is indicated (enzymes are prescribed). Physiotherapy is effective: electrophoresis, ozokeritotherapy, paraffin therapy, mud applications.
Correction of biliary dyskinesia begins with the establishment and elimination of the cause of its development. Drug therapy consists in the appointment of choleretic, enzyme preparations, neurotropic drugs.
Odeston is the drug of choice for the TREATMENT of most diseases of the biliary system. acts pointwise in 3 directions: firstly, it increases the formation and secretion of bile without stimulating contraction of the gallbladder, therefore it is safe even for patients with stones in the gallbladder, and secondly, it has a selective (targeted) antispasmodic effect directed only on the biliary tract and, finally, it reduces the stagnation of bile, prevents the crystallization of cholesterol and the formation of gallstones. Thus, Odeston helps to restore normal bile circulation, and therefore, helps to improve digestion.
Odeston is indicated for the treatment of diseases of the gallbladder and biliary tract, including cholelithiasis (cholelithiasis).
Physiotherapeutic procedures are used: electrophoresis, microwave therapy, paraffin and ozokerite applications, massage.
Therapy for intestinal dyskinesia depends on the form. With a predominance of constipation, laxatives are prescribed, in the case of a predominance of diarrhea in the clinical picture, antidiarrheal drugs. With a mixed form of intestinal dyskinesia, anticholinergic and antispasmodic drugs are indicated. In some cases, work with a psychologist or psychiatrist is required, taking neuroleptics or antidepressants.
Diet for dyskinesia
For all forms of dyskinesia, a sparing diet is indicated, frequent fractional meals are recommended, overeating should be avoided.
With dyskinesia of the esophagus, it is not recommended to eat foods high in fiber, spicy and spicy foods, alcohol.

Source: qulady.ru
With the development of a hyperkinetic form of biliary dyskinesia, the use of products that stimulate bile secretion is limited (carbonated drinks, vegetable oil, mushrooms, fatty meat, fish, spices, spicy and smoked dishes). With a hypokinetic form of pathology, it is recommended to include fruits, vegetables, sour cream, cream, butter, eggs in the diet.
Possible complications and consequences
Aspiration of stomach contents into the airways with esophageal dyskinesia contributes to the development of chronic bronchitis or pneumonia.
Against the background of biliary dyskinesia, gastritis, duodenitis, chronic cholecystitis, cholelithiasis, cholangitis can develop.
Intestinal dyskinesia contributes to the development of gastritis, peptic ulcer, neoplasms.
Forecast
The prognosis for esophageal dyskinesia depends on the form and severity of the pathology. In the absence of adequate therapy, esophageal dyskinesia can significantly reduce the patient's quality of life.
With timely, correctly selected treatment, the prognosis for gastric dyskinesia is usually favorable. Dispensary observation is shown to patients.
The prognosis for life with biliary dyskinesia is favorable, if the diet and the prescriptions of the attending physician are followed, exacerbations can be avoided. In the absence of timely treatment, the prognosis worsens, the risk of complications is high.
With intestinal dyskinesia, the prognosis for life is also favorable, however, it is possible to achieve long-term remission only in 10% of cases. The prognosis decreases in patients with a long history of pathology, chronic stress, and concomitant psychiatric disorders.
Prevention
In order to prevent the development of dyskinesia of any kind, it is recommended:
- balanced diet;
- avoidance of excessive physical and mental stress;
- adequate treatment of somatic diseases;
- rejection of bad habits;
- rational mode of work and rest.
YouTube video related to the article:

Anna Aksenova Medical journalist About the author
Education: 2004-2007 "First Kiev Medical College" specialty "Laboratory Diagnostics".
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!