- Author Rachel Wainwright wainwright@abchealthonline.com.
- Public 2023-12-15 07:39.
- Last modified 2025-11-02 20:14.
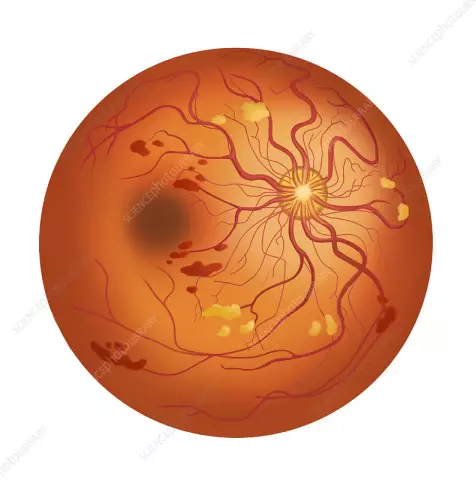
Retinal disinsertion

Retinal detachment is the most formidable eye disease that can lead to complete loss of vision in a fairly short time. According to statistics, 72% of all cases of blindness occur due to retinal detachment.
The retina is the membrane that lines the eye from the inside and consists of several layers of light-sensitive cells, which are the main link in the mechanism of image perception and transmission to the brain. This membrane is tightly connected to the choroid of the eye, and is pressed against it by the vitreous body.
In some cases, a pathological process occurs, as a result of which the retina is detached from the choroid in one or several areas. The vitreous fluid enters the rupture site, which exfoliates the retina. The retina, detached from the choroid, ceases to receive blood supply, as a result of which it atrophies and dies. If urgent measures are not taken at this stage, the fluid, penetrating further and further, can lead to total retinal detachment, which will lead to loss of vision in the affected eye.
Retinal Detachment Causes
The immediate cause of retinal detachment is the formation of micro-tears in it and liquefaction of the vitreous body, due to which free fluid enters the tears. This condition can occur as a result of trauma, and not necessarily a direct injury to the eye, but a blow to the head or even simply excessive physical exertion or stress. Also, the cause of retinal detachment can be general diseases of the body, such as diabetes mellitus, hypertension, kidney disease, systemic (scleroderma, rheumatoid arthritis, systemic lupus erythematosus, etc.) and infectious (especially viral infections) diseases, as well as diseases of the endocrine glands (thyroid, adrenal, parathyroid glands).
The age factor is also important, since retinal detachment most often occurs in people after sixty years, although it can occur at any age.
Types of retinal detachment
Retinal detachment can be primary or secondary.
- Primary. It occurs when fluid from the liquefied vitreous enters the retinal tear.
- Secondary. It occurs when a neoplasm appears between the retina and the choroid. These can be tumors, hemorrhages, diabetic retinopathy, or inflammatory infiltration.
According to the degree of mobility, the retinal detachment can be mobile or rigid. Diagnosis of retinal detachment to determine its mobility looks like this: the patient is prescribed a two-day bed rest, after which the position of the retina is checked. If the retina is completely adherent, it is said to be mobile, if not, then various degrees of mobility or complete rigidity are determined if there is no adherence throughout.
Retinal detachment can be high if the fluid accumulated under it has collected in a bladder, or flat, in which the retina is collected in folds.
The classification of retinal detachment by prevalence is also accepted:
- Local - within one quadrant
- Common - occupies two quadrants
- Subtotal - within three quadrants
- Total retinal detachment - the retina is detached all over
Retinal Detachment Symptoms
Retinal detachment symptoms manifest themselves as visual disturbances. Early symptoms of retinal detachment include the appearance of small, irregular dark spots in front of the eyes, in the form of soot flakes, as well as the appearance of a "dark curtain" or gray shading in the field of view.
At an early stage, a characteristic symptom of retinal detachment is morning improvement, when, after sleep, the curtain in front of the eyes almost completely disappears and vision is restored. But during daytime activity, the veil reappears, and by the evening the symptoms of retinal detachment reach their peak - the "curtain" becomes so dense that practically nothing can be seen through it.
Another symptom of retinal detachment is flashes of light at the periphery of the vision, and large moving spots may appear in front of the eyes. Pain is not common in retinal detachment because the retina does not have pain receptors, but sometimes pain is present during the formation of the primary tears.
As the disease progresses, the symptoms of retinal detachment increase and vision in the affected eye deteriorates.
Retinal detachment diagnostics
Retinal detachment is diagnosed by an ophthalmologist using the following studies:
- Ophthalmoscopy (fundus examination), direct and indirect. Allows you to identify the exact localization of breaks, the state of the detached retina.
- Electrophysiological study, which gives an idea of the degree of disorders that have occurred in the detached areas of the retina and optic nerve.
- Determination of visual acuity, which gives an idea of the central part of the retina
- Computerized perimetry showing the state of the peripheral retina.
- Ultrasound examination of the eye to assess the degree of retinal detachment.
- Tonometry is the measurement of intraocular pressure.
Retinal Detachment Treatment

Retinal detachment can only be treated surgically. Retinal detachment surgery is the only reliable method to eliminate pathology, therapeutic methods can only be used as additional ones.
In the event that this is a small retinal detachment, the operation can be performed using laser or cryotherapy (cryopexy). When exposed to a laser or cryoinflammation, aseptic (non-infectious) inflammation is formed at the rupture site, which subsequently causes the appearance of scar tissue, tightly soldering the retina with the choroid. The fluid that has penetrated under the retina is gradually absorbed.
If retinal detachment occurs over a large area, extrascleral or endovitreal surgeries are used.
- Extrascleral retinal detachment surgery. Surgical intervention is performed on the surface of the sclera. These include extrascleral ballooning or extrascleral filling, due to which they achieve a snug fit of the retina to the choroid, after which a point "welding" is performed with a laser.
- Endovitreal retinal detachment surgery. In this case, the retina is affected after vitrectomy (extraction of the vitreous humor).
The main thing in the treatment of retinal detachment is its onset as early as possible, since the retina, which has not been in contact with the choroid for a long time, atrophies and ceases to perform its functions. In this case, the retinal detachment is not treated.
YouTube video related to the article:
The information is generalized and provided for informational purposes only. At the first sign of illness, see your doctor. Self-medication is hazardous to health!